-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 537-541
doi:10.5923/j.ajmms.20241403.01
Received: Sep. 15, 2023; Accepted: Jan. 31, 2024; Published: Mar. 2, 2024

Cytokine Status in Pregnant Women with Fetoplacentary Dysfunction Associated with COVID-19
Kholova Z. B.1, Shukurov F. I.2, Anvarova Sh. A.3
1Assistant of the Department of Obstetrics and Gynecology Termez Branch, Tashkent Medical Academy, Tashkent, Uzbekistan
2Doctor of Medical Sciences, Head of the Department of Obstetrics and Gynecology, Tashkent Medical Academy, Tashkent, Uzbekistan
3Assistant of the Department of Obstetrics and Gynecology, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Shukurov F. I., Doctor of Medical Sciences, Head of the Department of Obstetrics and Gynecology, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study included 150 pregnant women with fetoplacental dysfunction associated with COVID-19. The patients were divided into three groups based on the clinical course of COVID-19: Group I consisted of 40 pregnant women with a mild form of COVID-19, Group II included 40 pregnant women with a moderate form of COVID-19, and Group III comprised 40 pregnant women with a severe form of COVID-19. Additionally, a control group of 30 healthy pregnant women was established for comparison. All participants underwent clinical-laboratory and immunological examinations. The levels of cytokines in the blood serum were determined using the immunoassay method and the ELISA device. The study focused on analyzing the levels of cytokines IL-1β, IL-4, IL-6, IL-8, IL-10, and IFN-γ during the first week of hospitalization and two weeks after treatment. The results showed that the majority of women with fetoplacental dysfunction associated with COVID-19 exhibited a significant increase in certain cytokines. Specifically, there was an 8-fold increase in IL-1β levels, a 10-fold increase in IL-6, and a 4-fold increase in IFN-γ. These changes in the quantitative indicators of cytokines emphasize their important role in the development of fetoplacental dysfunction in women infected with COVID-19.
Keywords: Pregnant women, Fetoplacental dysfunction, COVID-19, IL-1b, IL-4, IL-6, IL-8, IL-10, IFN-γ cytokines
Cite this paper: Kholova Z. B., Shukurov F. I., Anvarova Sh. A., Cytokine Status in Pregnant Women with Fetoplacentary Dysfunction Associated with COVID-19, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 537-541. doi: 10.5923/j.ajmms.20241403.01.
1. Introduction
- The COVID-19 pandemic has profoundly impacted public health, with pregnant women facing particular challenges. Pregnancy induces unique physiological changes that can significantly affect the course and consequences of viral infections like COVID-19. Understanding the interplay between COVID-19 and pregnancy is crucial for developing effective clinical practices [1-4].The placenta plays a central role in fetal development, facilitating nutrient and gas exchange and waste elimination between the mother and fetus. Abnormalities in placental function, known as fetoplacental dysfunction, can adversely impact pregnancy outcomes. The effect of COVID-19 on placental function and structure is a critical area of investigation, as it can significantly influence these outcomes [5-8].Cytokines, key signaling molecules in immunity, inflammation, and hematopoiesis, have distinct profiles in pregnant women, crucial for maintaining a healthy pregnancy. However, COVID-19 can disrupt this balance, potentially leading to complications. Research into the cytokine status in the context of COVID-19 is vital for understanding the pathophysiology of the disease during pregnancy and its impact on both mother and fetus [9-10].Despite increasing research on COVID-19, a significant gap remains in our understanding of how the virus affects pregnant women and their fetuses, particularly in terms of cytokine responses and fetoplacental health. Understanding these cytokine profiles in COVID-19-affected pregnancies is essential for developing targeted therapies and management strategies, helping identify at-risk pregnant women for timely intervention [11-14].This research is also pivotal in understanding the long-term health outcomes for mothers and their offspring, informing postpartum care and future health policy. The widespread impact of the COVID-19 pandemic makes this research not only academically significant but also crucial for public health. It can guide the care of pregnant women during pandemics and improve preparedness for future global health challenges.Pregnant women infected with COVID-19 are susceptible to various complications, including fetoplacental dysfunction. This condition, a dysfunction of the maternal-placental-fetal system, disrupts the supply of nutrients and oxygen to the fetus, potentially leading to fetal growth restriction and premature birth [15-18]. The study of cytokine status in pregnant women with COVID-19-associated fetoplacental dysfunction is lacking. Changes in cytokine status may relate to the development of pregnancy complications, including fetoplacental dysfunction. Our literature review revealed no studies on cytokine status in pregnant women with COVID-19-related fetoplacental dysfunction, highlighting the need for our investigation [19-20].In conclusion, studying the cytokine status in pregnant women with fetoplacental dysfunction associated with COVID-19 is vital. This research is essential for enhancing our understanding of COVID-19's pathophysiology in pregnancy and for developing effective strategies to manage and mitigate its impact on maternal and fetal health.The aim of the study is to evaluate cytokine status in pregnant women with fetoplacental dysfunction associated with the disease of COVID-19.
2. Material and Methods
- 120 pregnant women with fetoplacental dysfunction related to COVID-19 were included in the study. According to the clinical course of the COVID-19 disease, all patients were divided into 3 groups: Group I - 40 pregnant women with mild COVID-19 disease, Group II - 40 pregnant women with moderate COVID-19 disease, and Group III - 40 pregnant women with severe cases of COVID-19. The control group consisted of 30 healthy pregnant women. All women underwent clinical-laboratory and immunological studies. The content of cytokines in blood serum was studied using the enzyme immunoassay ELISA device. Quantitative levels of IL-1β, IL-4, IL-6, IL-8, IL-10, and IFN-γ cytokines were analyzed on the day of hospital admission and 1 and 2 weeks after treatment.Ethical Aspects. The study procedure doesn't interfere with any ethical basics and oral agreement was taken to all patients.
3. Results
- Analysis of cytokine levels in the blood serum of pregnant women included in the study during the first week of the disease showed that many cytokines were at a high level. Among the 40 pregnant women with mild COVID-19 disease included in group I:20 were infected in the II trimester of pregnancy and 20 were infected in the III trimester of pregnancy. Women infected in the II trimester and 20 in the III trimester of pregnancy, Group III - 40 pregnant women with severe COVID-19 disease: 20 women in the second trimester of pregnancy and 20 women in the third trimester of pregnancy. The analysis of cytokine levels in the blood serum of pregnant women included in the study during the first week of the disease showed that many cytokines were at high levels. When analyzing cytokine levels in the blood taken in the first week of the disease in pregnant women of group I compared to women in the control group, the level of cytokine IL-1β was 4 times higher – 44.0±9.19, the level of cytokine IL-4 was 3 times higher – 75.0±9.38, and the level of cytokine IL-6 was 8 times higher – 56.0±9.05. It was also found that the level of cytokine IL-8 was 4 times higher – 40.0±7.79, the level of cytokine IL-10 was 3 times higher – 93.0±8.98, and the amount of IFN-γ was 4 times higher – 512.0±8.80 (p<0.01).The analysis of cytokine levels in the blood taken in the first week of the disease in pregnant women of group II showed that the levels of cytokines IL-1β, IL-4, and IL-6 were respectively 6 times – 66.6±8.96, 5 times – 125.1±8.96, and 10 times higher – 70.0±8.96. Also, the amount of cytokine IL-8 was 6 times higher – 60.4±8.32, the amount of cytokine IL-10 was 5 times higher – 155.0±8.96, and the amount of IFN-γ was 6 times higher – 768.0±8.96 (p<0.01).The analysis of cytokine levels in the blood taken in the first week of the disease in pregnant women of group III showed that the levels of cytokines IL-1β, IL-4, and IL-6 were respectively 8 times – 88.2±8.96, 6 times – 150.6±8.96, and 20 times higher – 140.6±8.96. Also, the amount of cytokine IL-8 was 8 times higher – 80.4±8.32, the amount of cytokine IL-10 was 6 times higher – 186.0±8.96, and the amount of IFN-γ was 8 times higher – 1024.0±8.96 (p<0.01) (see Table 1).
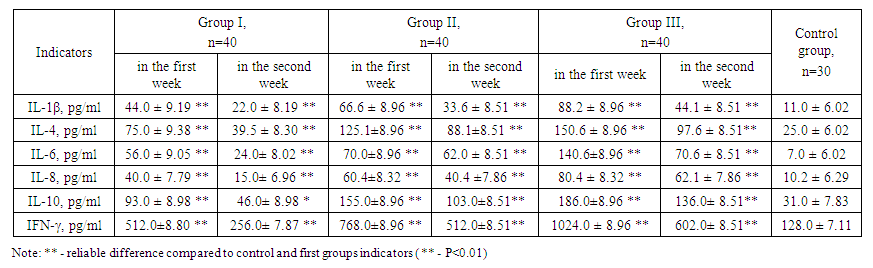 | Table 1. Indicators of cytokine levels in the first and second weeks of the disease in pregnant women with fetoplacental dysfunction associated with COVID-19, M±m |
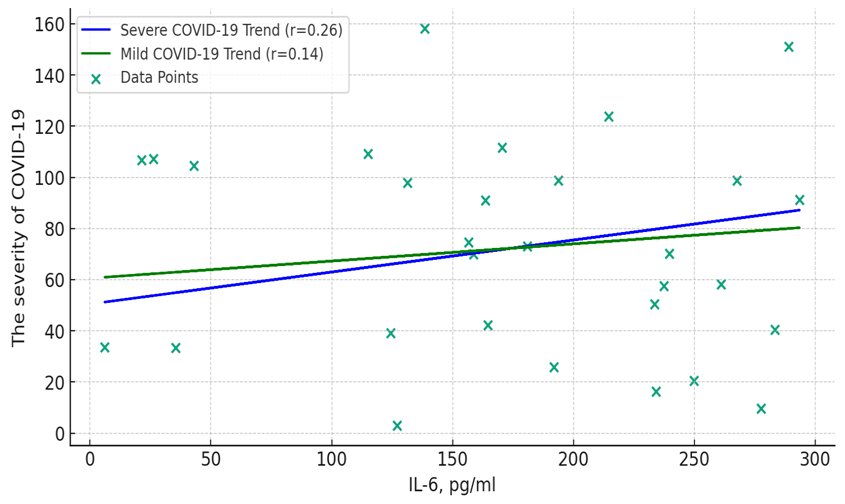 | Figure 1. Correlation between the clinical course of the disease of COVID-19 and the level of IL-6 cytokine in pregnant women included in the study |
4. Discussion
- This study presents a comprehensive and integrated analysis of cytokine levels in pregnant women with fetoplacental dysfunction associated with COVID-19, highlighting the crucial role cytokines play in the body's immune response and their impact on placental function and fetal well-being. The results reveal a significant elevation in cytokine levels, particularly IL-1β, IL-4, IL-6, IL-8, IL-10, and IFN-γ, during the first week of the disease, with a notable decrease in the second week across all groups. This pattern indicates an intense inflammatory response in the early stages of COVID-19, more pronounced in women with moderate to severe forms of the disease. Elevated levels of cytokines, especially IL-6, IL-8, and IFN-γ, are consistent indicators of the development of fetoplacental dysfunction.The varying cytokine levels depending on the severity of COVID-19 suggest a direct correlation between these levels and the clinical course of the disease. The initial elevation and subsequent reduction in cytokine levels reflect the body's adaptation to the infection or the result of medical intervention. This dynamic response underlines the importance of regular monitoring of cytokine levels in managing pregnant women with COVID-19, as it can assist in predicting the severity of the disease and tailoring appropriate clinical interventions.Pregnancy induces immunological and physiological changes that might exacerbate the cytokine response to COVID-19, thereby increasing the risk of complications such as fetoplacental dysfunction. Elevated cytokine levels can disrupt placental function, potentially leading to complications like fetal growth restriction and premature birth. These findings underscore the need for targeted therapies, particularly anti-inflammatory treatments, in cases with elevated cytokine levels.Furthermore, the study confirms that cytokines play a significant role in the development of fetoplacental dysfunction in pregnant women infected with COVID-19. It is essential to conduct further research to understand better the role of cytokines in the development of this pathology and to develop more effective treatment methods. Future studies should also explore how elevated cytokine levels affect newborn health and potential implications for their future development.The results obtained can serve as a foundation for developing more effective methods of diagnosis, treatment, and prevention of fetoplacental dysfunction in pregnant women with COVID-19. This research adds significantly to the growing body of knowledge about COVID-19's impact on pregnant women, which is vital from a public health standpoint. It emphasizes the need for special care and protocols for managing pregnant women during pandemics and can guide postpartum care and future health policy.In conclusion, this study underscores the complexity of COVID-19's impact on pregnant women, particularly those with fetoplacental dysfunction. The cytokine profile is critical in understanding the disease's pathophysiology and offers a pathway for developing more effective treatment and management strategies for this vulnerable population. The findings highlight the importance of cytokine monitoring in pregnant women with COVID-19 and lay the groundwork for future research and clinical practice improvements.
5. Conclusions
- The study emphasizes the significant impact of the COVID-19 pandemic on public health, particularly on pregnant women. It demonstrates how COVID-19 can cause substantial changes in the cytokine profile of pregnant women, which is especially important in the context of fetoplacental dysfunction. The observed increase in cytokine levels, such as IL-1β, IL-4, IL-6, IL-8, IL-10, and IFN-γ, in the first week of the illness followed by a decrease in the second week indicates an intense inflammatory response, especially in women with moderate and severe forms of COVID-19. These findings underscore the importance of cytokines as indicators of the development of fetoplacental dysfunction. Differences in cytokine levels depending on the severity of COVID-19 suggest a direct correlation between these levels and the clinical course of the disease. The study highlights the necessity of regular monitoring of cytokine levels for managing the condition of pregnant women with COVID-19, which can assist in predicting the severity of the illness and in developing appropriate clinical intervention strategies. This research emphasizes the complexity of COVID-19's impact on pregnant women, particularly those suffering from fetoplacental dysfunction. The cytokine profile plays a key role in understanding the pathophysiology of the disease and opens a pathway for developing more effective treatment and management strategies for this vulnerable population. The obtained results highlight the importance of monitoring cytokine levels in pregnant women with COVID-19 and lay the foundation for future research and clinical practice improvements.Conflict of interests. The authors declare no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML