Abdurazakova Mukhayo Dilshodovna, Babajanova Gulzhakhon Sattarovna, Razzakova Nilufar Saidakhmadovna
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Chronic diseases of the gallbladder and biliary tract are one of the most common diseases, ranked third after cardiovascular disease and diabetes. The study was conducted in the department of pathology of pregnant women of the maternity complex №9, Tashkent city for the period 2019-2022, the history of patients admitted to inpatient treatment for chronic cholecystitis, gestational hypertension, preeclampsia were studied.
Keywords:
Chronic cholecystitis, Calculous cholecystitis, Gestational hypertension, Preeclampsia
Cite this paper: Abdurazakova Mukhayo Dilshodovna, Babajanova Gulzhakhon Sattarovna, Razzakova Nilufar Saidakhmadovna, The Role of Chronic Cholecystitis in the Development of Obstetric Complications, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 532-536. doi: 10.5923/j.ajmms.20241402.75.
1. Introduction
The latest studies conducted by WHO experts show that complications such as preeclampsia and eclampsia, spontaneous abortion, premature births, birth defects, and postpartum bleeding have increased significantly in the case of diseases of the hepatobiliary system. These listed obstetric pathologies are important factors leading to maternal and perinatal morbidity and mortality. In clinical practice, joint diseases of the liver and biliary tract are often noted, for example, chronic hepatocholecystitis [1].The symptomatic course of chronic calculous cholecystitis is repeated in 80% of cases against the background of conservative therapy during pregnancy, and in 9% of cases it ends with spontaneous abortion and premature birth. Chronic cholecystitis affects the complications of the gestation period. Suffering persistent nausea, vomiting, and salivation are observed in such patients. There is information in the scientific literature that early toxicoses last until the third trimester and are difficult to treat [1,2,3,4]. Rios-Diaz A. J. and colleagues in the USA, according to the conclusion of the research conducted by colleagues in the USA, 603 (15.3%) of 3950 pregnant women with cholecystitis had preeclampsia, 216 (5.5%) had gestational hypertension, and 69 (1.7%) had delayed fetal development, 331 (8.4%) had premature birth, 759 (19.2%) had a cesarean section on the background of cholecystitis [8]. According to the observations of the chief researchers, early toxicosis in patients with cholecystitis can last up to 20-30 weeks of pregnancy and turn into liver pathology [1].A number of other scientific researchers, based on the study of the effects of bile duct diseases on the course of pregnancy, determined the following: early toxicosis and spontaneous abortion of the fetus in the early stages of pregnancy, in the II and III trimesters - premature birth, preeclampsia, and especially life-threatening HELLP syndrome [6,7,10].Such data can also be seen in the results of a study conducted by RR Thamil Selvi and his colleagues (2011). They reported that 11.4% of 44 pregnant patients had preterm labor and 65.1% had a caesarean section [8]. A British study compared the rates of obstetric and perinatal complications between pregnant women who underwent cholecystectomy and those who received conservative treatment: spontaneous abortion 6.6% vs. 5.8%, stillbirth vs. 0.9%. 0.6%, preterm delivery 11.1% vs 7.5%, cesarean delivery 28.23% vs 23.9%. Another US government study shows that cholecystectomy performed in the third trimester has a negative effect on maternal and fetal outcomes compared to postpartum. Nevertheless, data from most scientific sources confirm the safety of surgical intervention for biliary pathology during pregnancy [9].Obstetric complications included antepartum and postpartum hemorrhage, rehospitalization within 90 days postpartum, and maternal morbidity and mortality. Maternal diseases explain the indications for hospitalization and a number of negative consequences in childbirth, namely, disorders of blood circulation in the brain, shock, cardiomyopathy, etc..Neonatal complications include preterm birth, low Apgar score, perinatal morbidity and mortality. Neonatal death is an indicator of a number of serious adverse outcomes, namely intraventricular hemorrhage, respiratory failure, sepsis, blood transfusions, and surgical procedures before discharge from the delivery room [5]. Based on the data of a number of scientific studies and scientific literature presented above, it can be concluded that biliary tract pathology is one of the important factors in the development of complications that can be observed during pregnancy, including hypertensive conditions.
2. Aim
To study the importance of gallbladder pathology in the development of obstetric complications.
3. Research Materials and Methods
The study included patients with biliary tract pathology and hypertensive syndrome who were treated in the Department of Pregnant Women's Diseases of the City Maternity Complex No. 9 in Uchtepa District of Tashkent City from January 2019 to September 2022.The subjects of the study (267 pregnant women) were divided as follows:We conducted a retrospective review of 237 patients with biliary tract disease at 22-41 weeks of pregnancy, during labor and early postpartum. All examined pregnant women were divided into 3 groups:Group I - the main group consisted of 133 pregnant women with diseases of the biliary tract, which were divided into 2 subgroups:I A group - pregnant women with bile duct diseases, n=101;Group I B - pregnant women with hypertensive syndrome at the same time as bile duct pathology, n=32.Group II - comparison group - pregnant women with hypertensive syndrome, but no pathology of the hepatobiliary system, n=104.The control group consisted of practically healthy pregnant women who did not have gall bladder and biliary tract pathology and hypertensive conditions at the same time as the physiological course of pregnancy and childbirth, n=30.The following indicators were selected as criteria for the inclusion of patients in the study:- pregnant women aged 19-41;- pathologies of the biliary tract, including chronic noncalculous cholecystitis, chronic calculous cholecystitis, and pregnant women with gallbladder polyps;- gestational hypertension, preeclampsia caused by pathology of bile ducts, as well as other etiological factors;- voluntary consent of the patient to participate in the study.The criteria for excluding the patient from the study are as follows:- age < 19 years;- scar and iatrogenic damage of bile ducts, mechanical jaundice caused by parasitic diseases;- accompanying diseases in the decompensation stage;- refusal of the patient to participate in the study.
4. The Obtained Results and Their Discussion
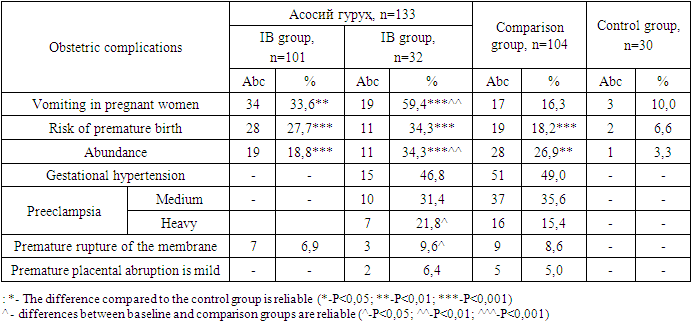
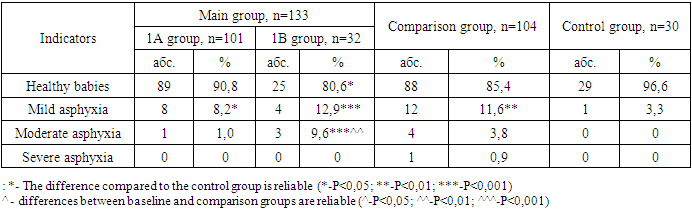
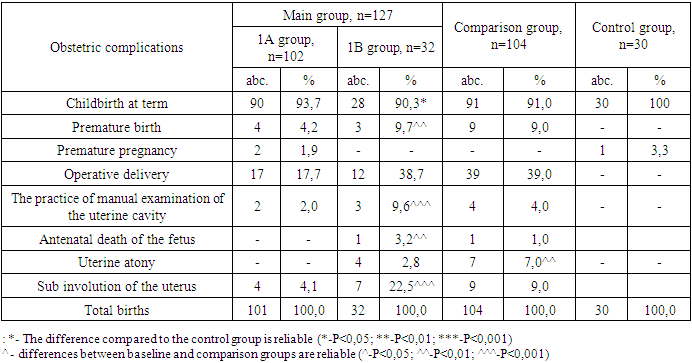
The age limit of the patients included in the study was between 19 and 41 years. The mean age in the main IA group is 26.5±5.3 years, in the IB group 28.1±5.5 years, in the comparison group it is 25.5±6.1 years, and in the control group it is 26.4±2.7 years. Pregnant women in the control group are also women of active reproductive age between 20 and 31 years old. The main difference is felt in the 19-23 age group, that is, this age group is the majority in the comparison group, statistically different from the main group by r<0.05.In order to study the importance of biliary system pathologies in the development of pregnancy and childbirth, obstetric and perinatal complications in patients under our control, we examined pregnant women with chronic cholecystitis and pregnant women without biliary tract pathology, hypertensive conditions of other etiologies, including gestational hypertension and preeclampsia. We compared and studied the obtained data.One of the most common complications of bile duct disease is vomiting in pregnant women. Among the examined patients, chronic cholecystitis and hypertensive conditions have the highest rate in pregnant women. 1 The difference between the indicators in group A and the comparison group was not significant. Table 1. Obstetrical complications observed in this pregnancy, n=267
 |
| |
|
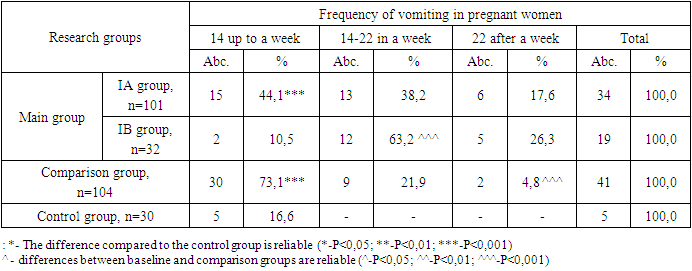
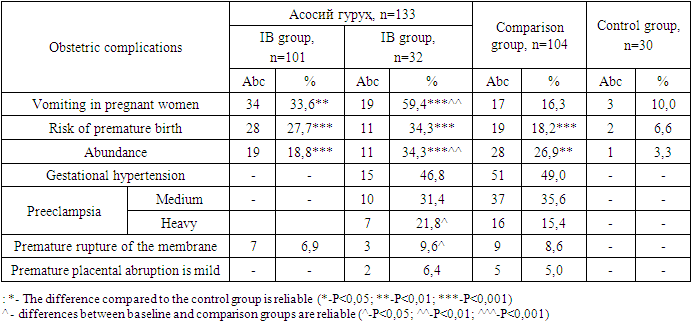
It can be seen that vomiting of pregnant women occurs frequently in bile duct pathologies, as well as in hypertensive cases without this pathology. This condition may be persistent and treatment may not be effective in all cases. According to the results of the study, vomiting in the case of preeclampsia, which occurred on the background of cholecystitis, is distinguished by its duration compared to other groups. In the 1A and comparison groups, the vomiting syndrome was mainly observed up to 14 weeks. In the period of 14-22 weeks and after 22 weeks, the prevalence of vomiting was found in 63.2% (12), 26.3% (5) subjects of group 1B.Table 2. Description of vomiting in pregnant women
 |
| |
|
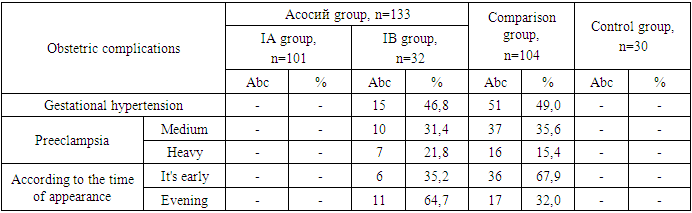
The role of the pathology of the hepatobiliary system in the pathogenesis of early toxicosis of pregnant women is not fully elucidated. The correlation between early toxicosis and chronic cholecystitis was shown in the research. In patients with toxicosis of pregnancy, chronic cholecystitis was manifested earlier than in women without toxicosis. We can explain this situation by the fact that in our women with toxicosis, the limited diet, the inability to eat timely and full meals motivates the early development of cholecystitis. On the other hand, cholecystitis can aggravate the toxicosis of pregnant women.One of the complications of obstetrics is premature birth. When we studied the level of their occurrence, it was found that the group with preeclampsia had a higher rate, that is, 7.1% and 7.8%. This may be due to severe preeclampsia induced or surgically induced births. However, this indicator was 4.3% in the group with chronic cholecystitis. Table 3. Description of hypertensive syndrome
 |
| |
|
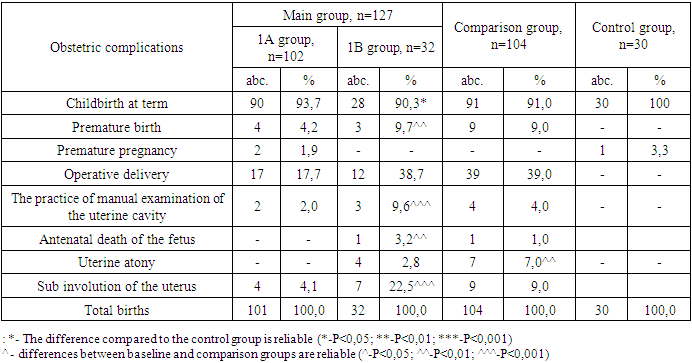
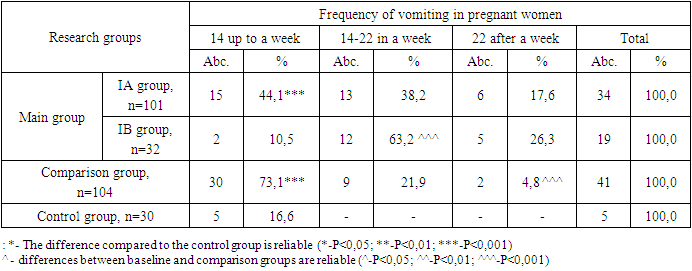
According to severity of preeclampsia in group 1B moderate level is 31.4% (10), severe level is 21.8% (7) and group 2 is 35.6% (37) and 15.4% (16), respectively. If we analyse according to the time of manifestation of preeclampsia, early preeclampsia, that is, manifested before 34 weeks, in the comparison group, 67.9% (36) cases of early preeclampsia occurred, and in group 1B, 64.7% (11) of late preeclampsia (appeared after 34 weeks) dominate with observation. This shows that late preeclampsia phenotype in group 1B is related to diseases of modern development, such as obesity, calculous cholecystitis, while in group 2, it confirms the data that early preeclampsia is related to kidney, liver, and systemic diseases.Table 4. Birth outcomes and obstetric complications
 |
| |
|
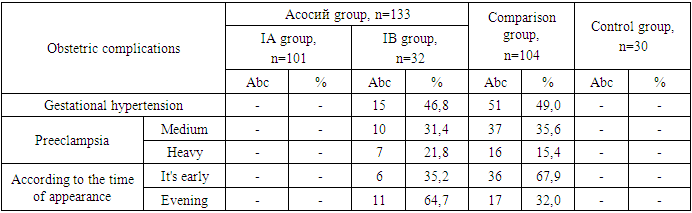
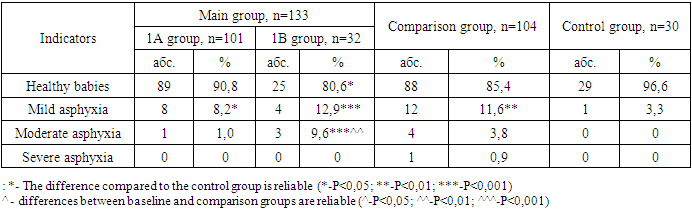
127 out of 133 pregnant women in the main group, 100 out of 104 in the comparison group, all pregnant women in the control group gave birth in maternity complex No. 9. In the analysis of the number of births at term, there is no significant difference between the groups. Premature delivery was twice as common in groups 1B and 2, where preeclampsia was recorded in comparison to group 1A and was 9.7 and 9.0%, respectively. Premature births are caused by preeclampsia and its complications. Their share corresponds to situations where preeclampsia is diagnosed in a severe degree.The rates of cesarean deliveries in groups 1B and 2 are almost the same, while in group 1A they are 2 times less frequent. Indications for operative deliveries in groups 1B and 2 are related to hypertensive syndrome and its complications, while in group 1A uterine scar after cesarean section, caused by various somatic and obstetrical pathologies, is considered. The fact that NJYBK occurs in 6.4 and 5.0% of hypertensive groups confirms our above opinion. No such birth complications were observed in the control group.In patients of groups 1 and 2, obstetric complications such as premature rupture of membranes (QPMOYo) and premature rupture of membranes (QPTOYo) were 2.0% (2) in group 1A, 9.6% (3) in group 1B, 7.0% in the comparison group. % (7) was noted in patients.In patients with gestational hypertension and preeclampsia, that is, in groups 1 B and 2, death of the fetus in the antenatal period was determined in one case (3.2% and 1.0%).The postpartum period in patients was complicated by uterine subinvolution. They are distributed among groups with the highest rate in group 1B with 22.5% (7), group 2 with 9.0% (9), and group 1A with 4.1% (4). Such a high result in group 1B is explained by the combination of multiple births, level of obesity and hypertensive conditions.In group 1B, the average amount of blood loss during childbirth was 340.83±22.8 ml, and in group 2, the average amount of blood loss was 385.1±30.32 ml. The results of both groups were significantly different from those of the control group, 275.0±15.3. The high volume of bleeding is explained by atonic bleeding observed after delivery 4 (12.8%) and 7 (7.0%) observed in the 1B and comparison group, as well as surgical deliveries. Atonic bleeding was stopped conservatively in all cases. Manual examination of the uterine cavity was performed in almost the same proportion of patients in groups 1 and 2 (3.9 and 4.0%). There was no need for blood transfusions, and infusion therapy was sufficient for the treatment to be effective.During the study, we studied the condition of the babies born from this pregnancy, based on the information of the history of the newborns. The condition of newborns was assessed using the Apgar scale. Due to the birth of 2 twins in group 1 and 3 twins in group 2, the number of children was greater than the number of women who gave birth, that is, the number of women who gave birth in group 1 is 127, the number of babies is 129, the number of mothers is 100, the number of babies is 103 in group 2. In almost all studied groups, the number of children born with a score of 7-8 and above was the majority. In group 1A, the number of children born with mild asphyxia was 8.2%, while in group 1B, 1.5 times more babies were born with 6-7 points, in group 2, this figure was 11.6%. Infants born from moderate asphyxia were mainly born to women with hypertensive conditions, distributed from 2(6.4%) and 4(3.8%) in groups 1B and 2, respectively. One infant with severe asphyxia was recorded in the comparison group. In the control group, only 1 out of 30 children (3.3%) was born with 6-7 points.Table 5. Analysis of the condition of newborns, n=267
 |
| |
|
The weight of newborns was 3393.6±73.6 g in group 1, 3206±62.1 g in group 2, and 3355.2±66.9 g in the control group, that is, there was no significant difference. In group 1, the smallest weight of babies was 2130.0 g, the largest weight was 5150.0 g. The same indicators were 2040.0 and 3860.0 gr. in the 2nd group, 2860.0 gr. and 3950.0 gr. in the control group. It can be explained by the fact that the weight of more than 4000.0 g among babies was found only in group 1A, the fact that such a large weight was not found in babies of women with hypertensive conditions, and the high rate of placental insufficiency observed in groups 1B and 2.Summary. Thus, the study of indicators describing the reproductive function of patients with chronic stoneless and calculous cholecystitis showed that they differ in many ways compared to the indicators of healthy patients. This was especially evident in women with cholecystitis and hypertensive conditions. On the background of chronic cholecystitis, pregnancy is complicated in most cases by continuous and painful vomiting, the risk of premature birth, and the development of hypertensive disorders.
References
| [1] | Vakhrushev Ya.M., Khokhlacheva N.A. Gallstone disease: epidemiology, risk factors, clinical features, prevention. Archives of Internal Medicine • № 3(29) • 2016. |
| [2] | Ostrik D. A. Features of the course of pregnancy in women with diseases of the biliary tract // Forcipe. – 2019. – No. Application. – P. 158-159. |
| [3] | Palieva N.V. et al. Course of pregnancy, childbirth, condition of the fetus and newborn with cholestatic hepatosis in pregnant women // Chief Physician of the South of Russia. – 2023. – №. 1 (87). – P. 40-43. |
| [4] | Spiridenko G.Yu., Petrov Yu.A., Chernavsky V.V., Palieva N.V. Acute fatty hepatosis in pregnant women: clinical manifestations, early diagnosis and treatment // Modern problems of science and education. – 2022. – № 2.; URL: https://science-education.ru/ru/article/view?id=31656. |
| [5] | Ibiebele I, Schnitzler M, Nippita T, Ford JB. Outcomes of gallstone disease during pregnancy: a population-based data linkage study. Paediatr Perinat Epidemiol 2017; 31: 522–530. |
| [6] | Mirzayeva D. B. Features of the course of pregnancy and childbirth after in vitro fertilization (IVF), taking into account the factor of infertility // Journal of education and scientific medicine. – 2023. – Т. 1. – №. 1. – С. 12-17. |
| [7] | Mukhayyo Dilshodovna Abdurazakova, Guljakhon Sattarovna Babadjanova, Diseases of the biliar system in pregnant women. Journal of Biomedicine and Practice 2020, vol. 6, issue 5, pp. 54-63. |
| [8] | R.R. Thamil Selvi, Pammy Sinha, P.M. Subramanian, P.G. Konapur, C.V. Prabha; Clinicopathological study of cholecystitis with special reference to analysis of cholelithiasis, International Journal of Basic Medical Sciences, 2011, vol 2: issue 2: pp 68-72. |
| [9] | Rios-Diaz, A. J., Oliver, E. A., Bevilacqua, L. A., Metcalfe, D., Yeo, C. J., Berghella, V., & Palazzo, F. (2020). Is It Safe to Manage Acute Cholecystitis Nonoperatively During Pregnancy? Annals of Surgery, 272(3), 449–456. doi:10.1097/sla.0000000000004210. |
| [10] | Sattarova K. A. et al. Clinical and Biological Importance of Micro RNA in the Formation of Women Reproductive Losses // Indian Journal of Forensic Medicine & Toxicology. – 2020. – Т. 14. – №. 4. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML