Mirzamurodov Kh. Kh.1, Khodjanov I. Yu.2, Novikov K. I.3, Klimov O. V.4, Khakimov Sh. K.5
1Department of Traumatology and Neurosurgery, Bukhara State Medical Institute named after Abu Ali ibn Sina, Bukhara, Uzbekistan
2Doctor of Medical Sciences, Scientific Director of the Department of General Orthopedics of the Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Tashkent, Uzbekistan
3Doctor of Medical Sciences, Traumatologist-orthopedist LLP No. 13, National Medical Research Center for Traumatology and Orthopedics named after Academician G.A. Ilizarov. Kurgan, Professor, Institute of Clinical Medicine, Department of Traumatology and Orthopedics, Tyumen State Medical University, Tyumen, Russia
4Doctor of Medical Sciences, Traumatologist-orthopedist, Department of Rehabilitation, National Medical Research Center for Traumatology and Orthopedics named after Academician G.A. Ilizarov, Kurgan, Russia
5Candidate of Medical Sciences, Assistant at the Department of Traumatology and Neurosurgery, Bukhara State Medical Institute named after Abu Ali ibn Sina, Resident Doctor at the Department of Consequences of Trauma and Pediatric Orthopedics at the Bukhara Regional Children's Multidisciplinary Medical Center, Bukhara, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Purpose research was to study the structures of possible errors and complications in patients with hypo and achondroplasia after the technique of minimally invasive counter corticotomy of the femur. The study involved 35 patients aged 7 to 18 years treated in clinics Bukhara Regional Multidisciplinary Medical Center and the Federal State Budgetary Institution “National Medical Research Center for Tomorrow named after Academician G.A. Ilizarov of the Russian Ministry of Health with polysegmental deformities and shortening of the lower extremities of genetic etiology of development. At the clinic, we improved the technique of classical corticotomy, as a minimally invasive counter corticotomy (first from the medial side and then from the anterior outer surface) with osteosynthesis using an external fixation device (AFD), with the obligatory “final” stabilization of the device systems with tension rods or hinge units. The above analysis of the clinical significance of recorded errors and complications and their impact on the final result of treatment clearly showed the relative informativeness of quantitative data. Thus, the final line of the table shows 35 negative events, which amounted to 175% of the number of patients treated and 56.45% of the number of operated segments, but in 33 cases (94.3% of all errors and complications) a negative impact on the final there was no treatment result, and only two negative events became complications, which amounted to 10% of the number of patients treated and 3.2% of the number of operated segments and 5.7% of all errors and complications. Thus, after analyzing errors and complications, we identified the most risky periods of treatment in terms of the likelihood of unforeseen negative situations occurring, and also characterized each period of treatment in terms of the errors and complications inherent in them. Transosseous osteosynthesis with an external fixation device according to Ilizarov allowed the doctor to eliminate problems without allowing them to develop negatively and turn into complications.
Keywords:
Achondroplasia, Corticotomy, Osteogenesis, Hyperemia, Polysegmental, Musculoskeletal system
Cite this paper: Mirzamurodov Kh. Kh., Khodjanov I. Yu., Novikov K. I., Klimov O. V., Khakimov Sh. K., Errors and Complications in Operated Patients with Congenital Diseases of the Lower Limb, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 491-498. doi: 10.5923/j.ajmms.20241402.67.
1. Introduction
The rapid development of modern traumatological and orthopedic surgery has led to a steady increase in the type of orthopedic surgical interventions both for the consequences of injuries and for orthopedic diseases of the musculoskeletal system, which dictates the search for new methods of osteotomy of long tubular bones while preserving the biological properties of the bone marrow.Achondroplasia is a rare genetic disease that leads to severe short stature and abnormal body proportions. This occurs due to shortening of the limbs due to improper conversion of cartilage into bone. As a result, the height of adults with achondroplasia does not exceed 125-130 sm [3,4,5,6,7,8,12,13,14].Scientists from different specialties have extensively studied the problem of increasing height in patients with achondroplasia and have come to the conclusion that there is currently no alternative to surgical limb lengthening in the treatment of this group of patients [1,2,6,9,10,11].A widely known and proven method of treating achondroplasia throughout the world is surgical correction of deformities and limb lengths using the Ilizarov method using special internal or external devices. Surgical correction today is the most effective way to equalize body proportions and eliminate orthopedic disorders characteristic of the disease. However, despite being highly effective, the surgical route is extremely traumatic. Treatment takes a long time and is associated with a high risk of complications.Various types of femoral osteotomy allow for correction of deformities, lengthening and replacement of defects. But, the mechanical approach to performing distraction- compression transosseous osteosynthesis using an external fixation device (EFD) with performing osteotomy of the femur without taking into account the characteristics of osteogenic tissues with bone marrow damage is often the reason for obtaining undesirable treatment results in the form of delayed consolidation, nonunions and pseudarthrosis and, as a rule, with the need for repeated, initially unplanned operations, which requires additional time, money and resources to achieve the desired treatment result.Purpose: The study was to study the structure of possible errors and complications in patients with hypo- and achondroplasia after the technique of minimally invasive counter corticotomy of the femur.
2. Materials and Methods of Research
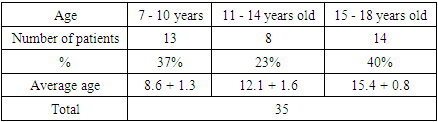
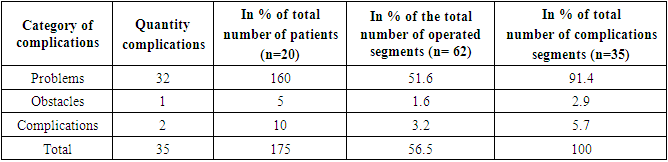
The study included 35 patients aged 7 to 18 years who were treated at Department “Consequences of Trauma and Orthopedics” on the basis of the Bukhara Regional Multidisciplinary Medical Center and the Federal State Budgetary Institution “National Medical Research Center for Trauma and Orthopedics named after Academician G.A. Ilizarov" of the Ministry of Health of Russia. The patients had polysegmental deformities of the lower extremities, the cause of which was a systemic lesion of the patient’s musculoskeletal system as a consequence of a genetic abnormality.A characteristic feature of patients with systemic lesions of the musculoskeletal system is the closure of the growth zone of long tubular bones 3 to 4 years earlier than in patients with undisturbed osteogenesis. The age distribution of patients is given in Table 1.Table 1. Age composition of patients in the general study group
 |
| |
|
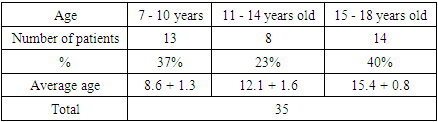
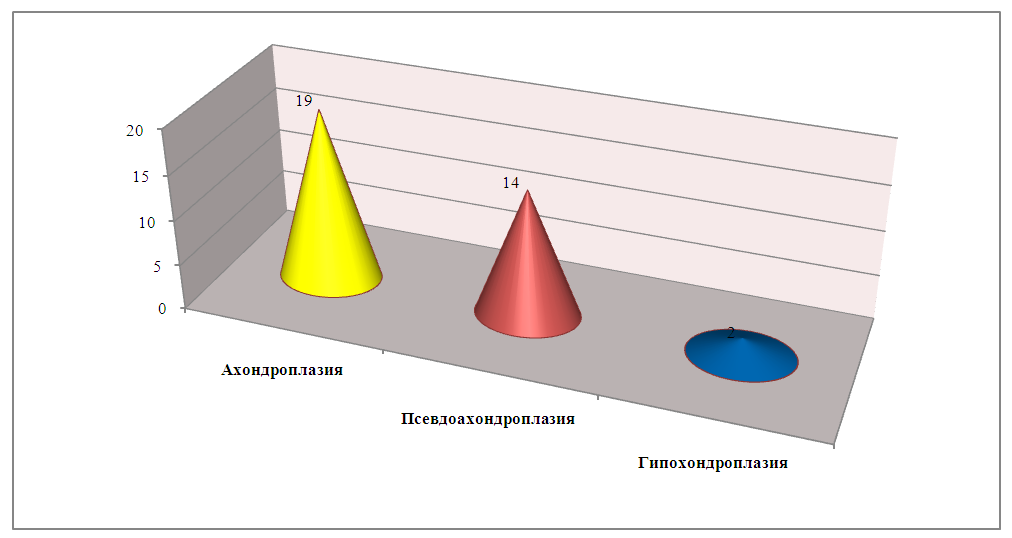
According to Table 1, it can be concluded that patients with shortenings and deformities of the lower extremities were noted in the 1st junior (7-10 years) and 3rd school age (15-18 years) in 13 and 14 cases, respectively.Also, patients are distributed according to nosological units, the data is shown in Diagram 1.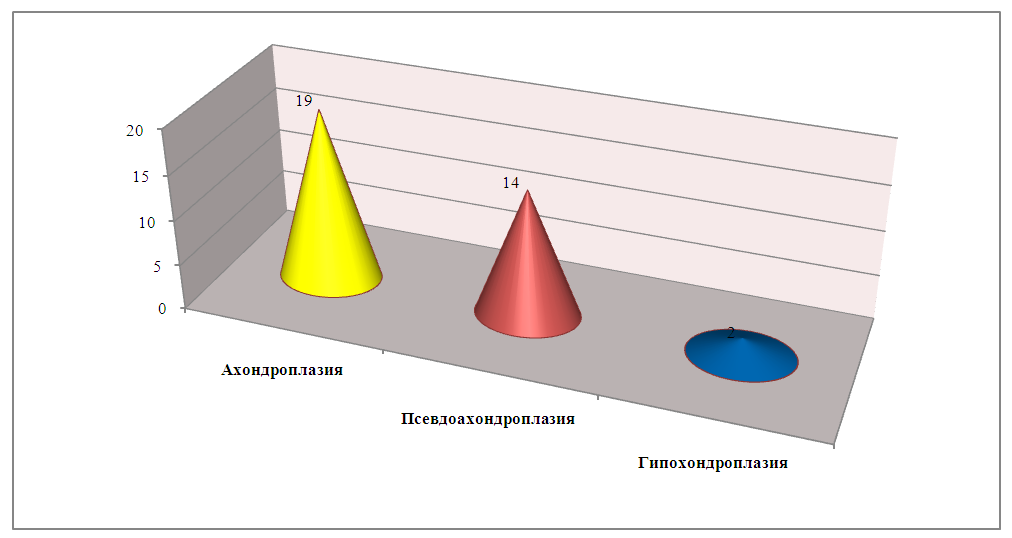 | Diagram 1. Distribution of patients by nosological units |
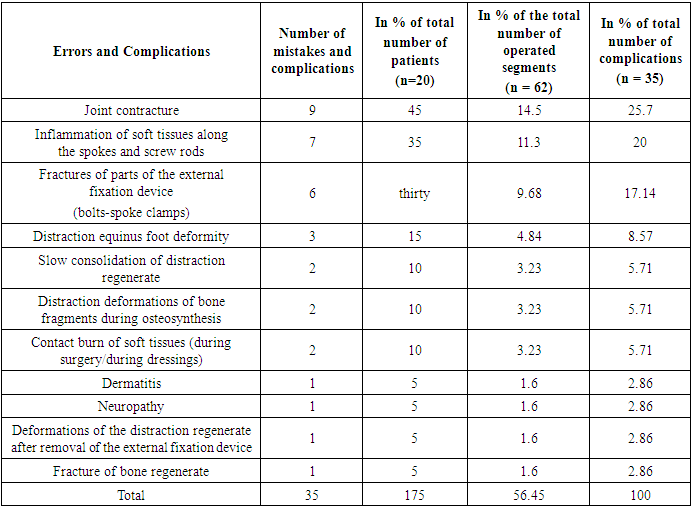
From the data in Diagram 1 it is clear that most often patients were diagnosed with achondroplasia in 19 cases and pseudoachondroplasia - 14 cases out of 35 patients.We at the clinic improved the corticotomy technique, taking into account some of the shortcomings identified during the analysis of retrospective data. The technique is called counter corticotomy, which requires a list of standard orthopedic operating room equipment to perform in the distal third of the femur. In addition to a scalpel, a set of levators, an orthopedic hammer, an osteotome or a chisel, this list must include a power unit (medical drill), drills and trocars of various diameters for corticoperforations.Possible errors and complications, ways to level them out and prevention of complications.We are impressed by the opinion of the Ilizarov Center, which initially considers unplanned negative events that arise during treatment using the Ilizarov method as temporary negative events requiring conservative measures, but not as complications that require unplanned surgical treatment. In our main group of patients, the list of errors and complications changed its usual gradation, so inflammation of the soft tissues gave way to the leading position usual for transosseous osteosynthesis, and the entire list of negative events and their quantitative data are shown in Table 2.Table 2. List of errors and complications encountered during treatment in patients of the main group
 |
| |
|
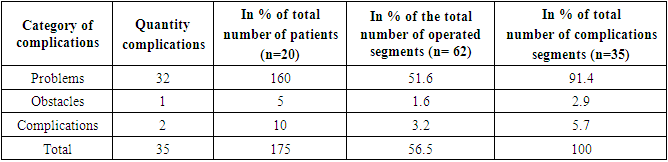
In Table 2 we reflected all the negative events mentioned not only in the diaries of medical histories, but also those that arose after discharge from the hospital and which were not noted in the medical histories and about which the doctor learned from correspondence or during control examinations in an outpatient setting ( which were observed both during osteosynthesis and after removal of the device). The following analysis of the clinical significance of the recorded errors and complications and their impact on the final result of treatment clearly showed the relative informativeness of quantitative data. Thus, the final line of the table shows 35 negative events, which amounted to 175% of the number of patients treated and 56.45% of the number of operated segments, but in 33 cases (94.3% of all errors and complications) a negative impact on the final there was no treatment result, and only two negative events became complications, which amounted to 10% of the number of patients treated and 3.2% of the number of operated segments and 5.7% of all errors and complications, which can be considered correct indicators and reflective their real clinical significance.In our list of observed errors and complications, distraction contractures of joints adjacent to the segment being lengthened took the first line of problems during lengthening, which clearly demonstrated the need for high-quality, timely and permanent exercise therapy. Limitations of movement in the joints were noted in 9 patients (45% of the total number of patients and 14.5% of the number of operated segments), which can partly be explained by the early discharge of patients from the hospital and the lack of necessary conditions for the development of joints at their place of residence. During the period of distraction, contractures were gradually progressive. But during the fixation period, almost all patients were able to increase the range of motion in adjacent joints and finally restore range of motion after removal of the device. Only one patient (5% of the total number of patients and 1.6% of the number of operated segments) retained persistent contracture of the knee joint, which requires intensive rehabilitation measures.We observed inflammation of soft tissues along the wires and rod-screws in 7 patients of the main group (35% of the total number of patients and 11.3% of the operated segments). In most cases, the problem was stopped in a short time and without consequences, at the stage of hyperemia, and only in two patients (10% of the total number of patients and 13.23% of the number of operated segments) inflammatory discharge was observed, but these inflammations did not have a negative continuation and were successfully resolved. The standard treatment regimen: changing the dressing regimen, prescribing antibiotics, temporarily reducing physical activity, allowed all patients not only to save the problematic wires and continue distraction or fixation, but also to successfully complete the treatment; replacement of the wires was not required. But one problematic rod-screw on the femur was removed and, in order to maintain the necessary stability of the support and rigidity of fixation of the bone fragment for lengthening the femur, a new rod-screw was introduced.Unexpectedly, we were faced with a problem that was not of a medical nature, but which could have significantly affected the progress of osteosynthesis if it had not been eliminated in time. So in 6 patients of the main group (30% of the total number of patients and 9.68% of the number of operated segments) a fracture occurred in the fixing parts of the external fixation device: the pin-fixing bolts broke, both in the operating room and during the process of osteosynthesis. This category also includes “thread failure” in threaded parts, which occurred, but we did not record these mechanical problems. The solution to this problem relates to materials science and compliance with GOST standards in the manufacture of all parts of the Ilizarov apparatus set, as well as an unresolved ethical problem - the problem of reusing parts.In 3 patients (15% of the total number of patients and 4.84% of the number of operated segments) developed distraction equinus foot deformity. But in no case did we require additional surgical treatment; in all patients, the foot deformity was eliminated conservatively: by prescribing enhanced exercise therapy and corrective gymnastics, using an elastic footpad and reducing the rate of distraction.Slow consolidation of the distraction regenerate was noted in 2 patients of the main group (10% of the total number of patients and 3.23% of the operated segments). In the first case, the situation arose due to the patient’s parents’ violation of the doctor’s recommendations, who categorically recommended stopping lengthening due to the appearance of radiological signs of the formation of a pathological type of distraction regenerate of the tibia and the continuation of distraction led to a decrease in the reserve capacity for the formation of a full-fledged distraction regenerate. The fixation period lasted significantly longer than planned. No additional treatment was performed. In the second case, the patient had little use of the operated limb during the lengthening and fixation period, and the distraction regenerate was deprived of the necessary component of its formation - adequate and regular axial load on the limb.Distraction deformation of bone fragments during osteosynthesis was noted in two cases (10% of the total number of patients and 3.23% of the operated segments). Carrying out a schedule of control x-rays gave us the opportunity to detect the appearance of segment deformations at the earliest stages. A timely change in the rate of distraction along the working rods in advance of the deformation made it possible to prevent not only further progression of the deformity, but in most cases to eliminate the deformation completely. If necessary, the doctor remounted the device and reinstalled the hinges. No additional unplanned treatment was performed.In two patients (10% of the total number of patients and 3.23% of the number of operated segments), we encountered an extremely rare situation when we observed a contact burn of the skin of I-II degree after treatment with an antiseptic. In the early postoperative period, in one patient we observed a problem that was not directly related to osteosynthesis, but which had a negative effect on the course of osteosynthesis for a long time. During surgery, the patient received a contact burn to the sacrum and buttocks with an aggressive antiseptic, which required long-term treatment, and the patient could not lie on her back during this entire period and needed special placement in bed. The error was successfully fixed without any negative consequences. In another patient, we received a local contact burn of the soft tissues of the thigh after performing a planned dressing with betadine, which can be regarded as a hyperreaction to an early, repeatedly used antiseptic drug. The problem was quickly resolved by replacing the antiseptic.In one patient (5% of the total number of patients and 1.6% of the number of operated segments) we observed dermatitis. An extremely rare general disease that affected the course of osteosynthesis, its timing and the final result of treatment. A sharp exacerbation of atopic dermatitis required emergency intensive treatment in a specialized hospital at a time when removal of the device was still premature. But on the recommendation of dermatologists, the devices were removed from the thigh and lower leg.Peroneal nerve neuropathy developed in one patient (5% of the total number of patients and 1.6% of the number of operated segments), at the end of distraction, by 7 cm of lengthening of the tibia (37% of the initial segment length). A temporary cessation of distraction, and then a decrease in its rate, and the administration of neurotropic drugs for a short time made it possible to completely eliminate the phenomena of neuropathy.Deformation of the distraction regenerate of the lower leg after removal of the external fixation device We observed one patient (5% of the total number of patients and 1.6% of the number of operated segments), in whom delayed consolidation of the distraction regenerate of the tibia was previously noted. On the day of removal of the device, a mobility test was carried out in the area of the bone regenerate; no pathological mobility was detected at the time of removal of the device; clinically, the axis of the tibia was correct. A plaster splint was applied. After removing the device, all patients are required to perform “safety-educational” plaster immobilization for a period of two to four weeks. Typically, we apply a deep plaster splint to the elongated segment, covering adjacent joints, and recommend a gradually increasing load using additional means of support. A few days after removal of the device, when the swelling of the soft tissues decreases and the splint becomes “large,” we remove the “old” splint, control the wounds from the needles and apply a new splint, which more rigidly performs the fixation function. This patient, while at home, from the first days began to walk without additional means of support and with full load on the limb, did not appear for a follow-up examination to change the splint and the immobilization characteristics of the “old” splint were not enough to prevent the development of valgus deformity of the tibia. The deformity occurred “inside” the splint and after its removal three weeks later, valgus deformity of the tibia was visible clinically. The girl’s parents refused manual correction “without delay”. We plan to correct the deformity of the lower leg during the next stage of treatment, with sequential lengthening of the thighs.A fracture of the tibial regenerate bone occurred in the next year after the removal of the apparatus. one patient (5% of the total number of patients and 1.6% of the number of operated segments), which, in our opinion, in this case can be considered a complication only conditionally related to osteosynthesis. The patient fell on a train during a trip to the next stage of treatment, lengthening and correction of deformities of the contralateral tibia. He underwent simultaneous osteosynthesis of the legs. In addition to stabilizing the tibia fracture to eliminate the deformity, it was additionally lengthened. No special stage for surgical treatment was required; the patient was very satisfied with the final result of the treatment.
3. Clinical Example
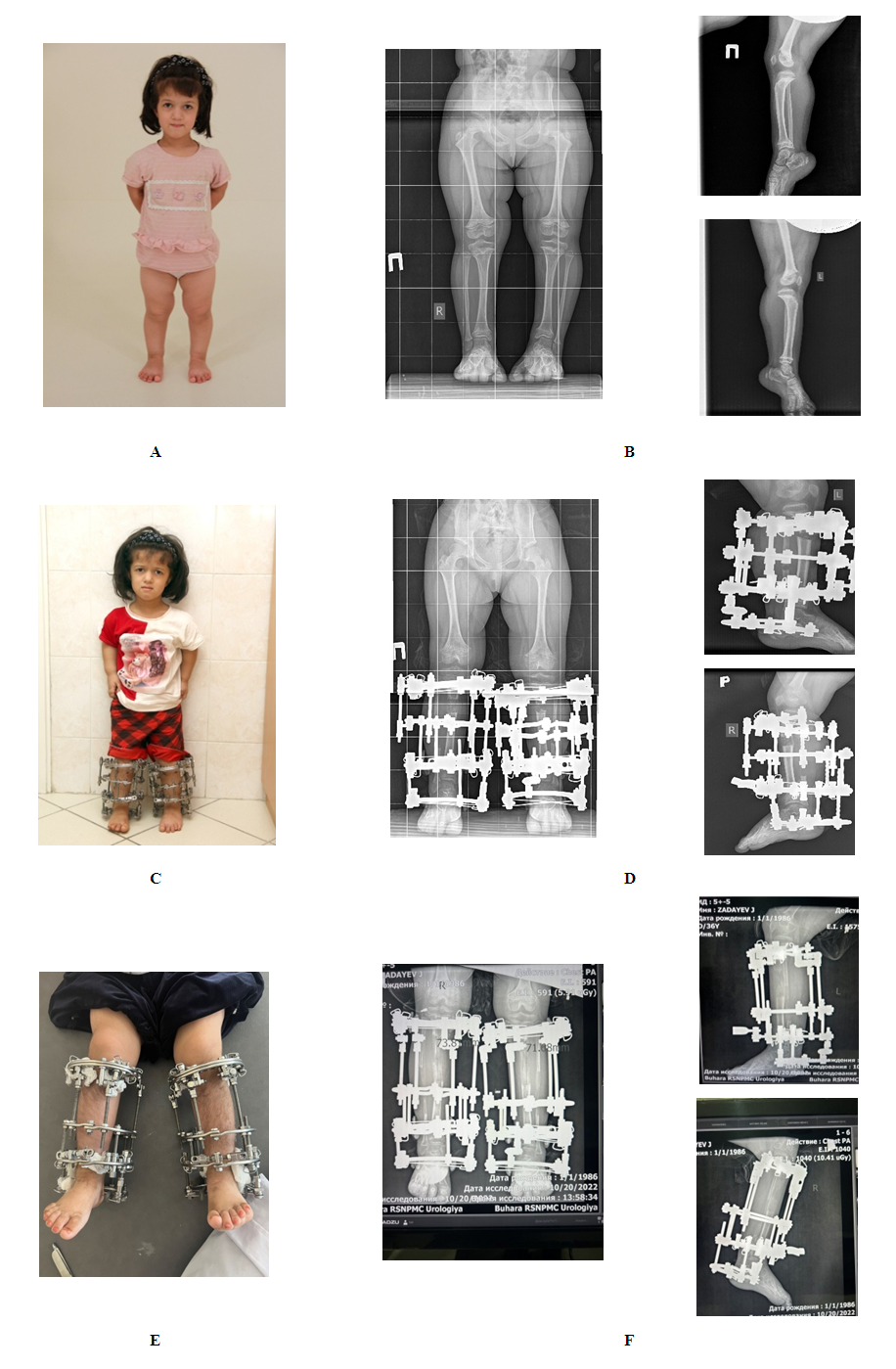
Patient M., 7 years old (ICSB No. 8404). Diagnosis: Achondroplasia. Low height 94cm. Disproportional shortening of the upper and lower extremities (Fig. 1, a, b). To restore growth, correct deformity and anatomical proportions of the patient's body, a two-stage increase in the longitudinal dimensions of the limbs was performed using options for one-stage simultaneous lengthening of the legs.At the first stage, the legs were lengthened (Fig. 1, c, d) by 7 cm, respectively. The duration of traction during osteosynthesis was 75 and 79 days; fixation 73 and 116 days. As a result, the patient's height increased by 7.5 cm.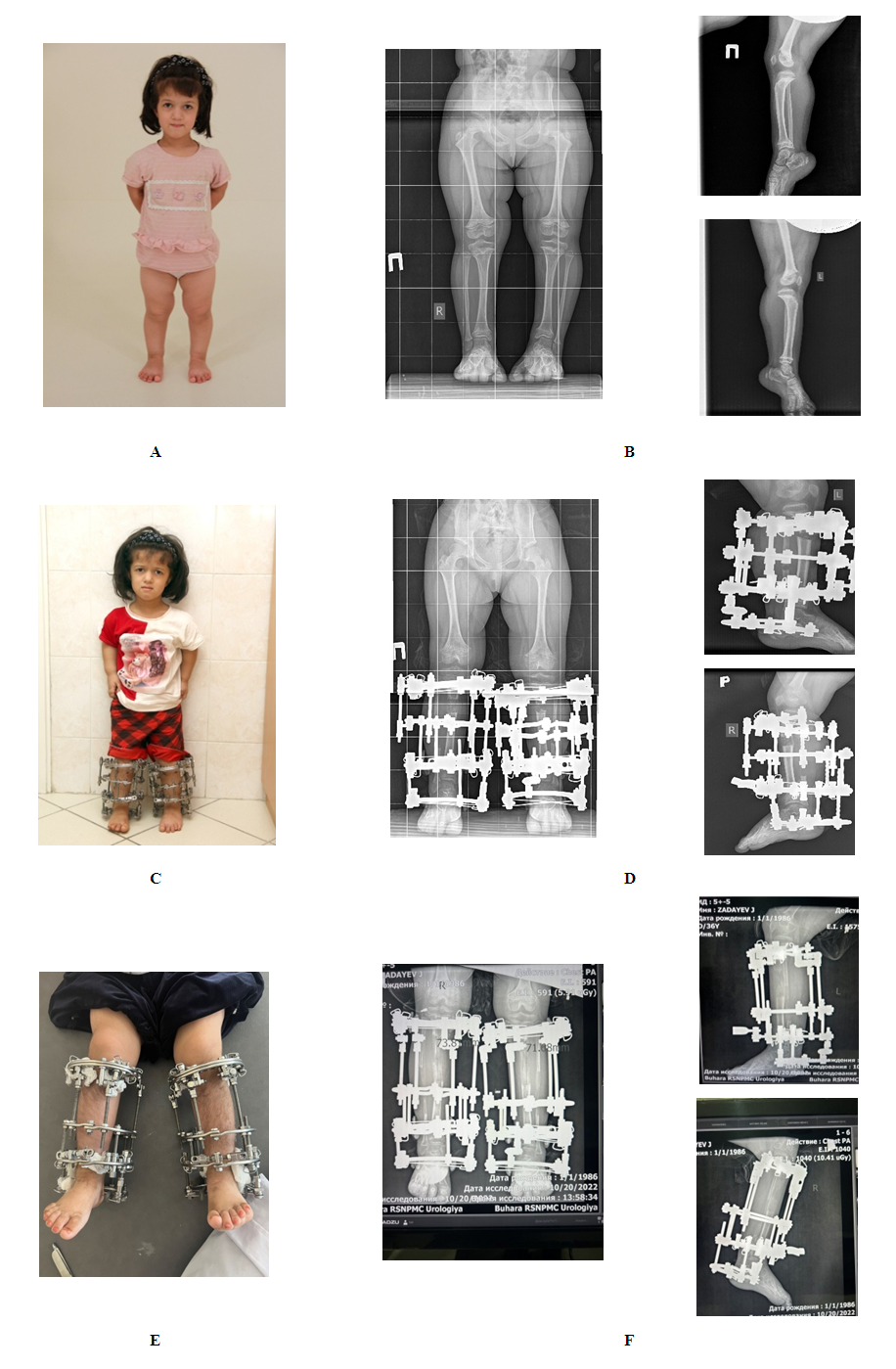 | Figure 1. Photos and radiographs of the legs of patient M. (ICSB No.8404): a, b – nature and radiographs of the lower leg before treatment; c, d – on the first days of the stage of growth increase; e, f – at the beginning of the stage of fixation of the legs |
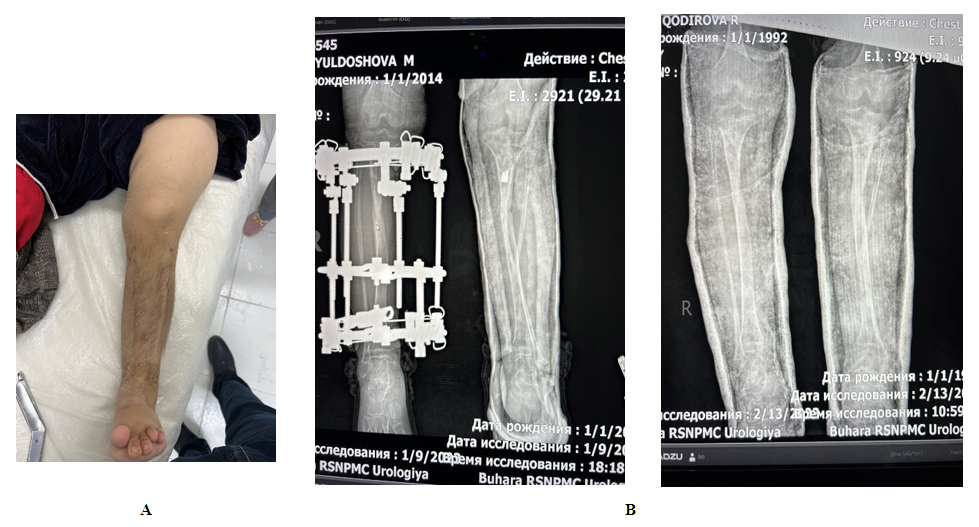
After the end of the fixation period, the device was removed from the left leg, and a splint plaster cast was applied from the middle third of the thigh to the heel area. At the time of the patient's visit, 10 days after applying a plaster cast to the left shin, a deformity (fracture) was discovered in the regenerated area of the left shin. The device was removed from the area of the right leg and a splint plaster cast was applied for 3 days, and after 3 days the splint was replaced with a circular plaster cast. Thus, the result on the right shin was maintained. (Fig. 2, a, b).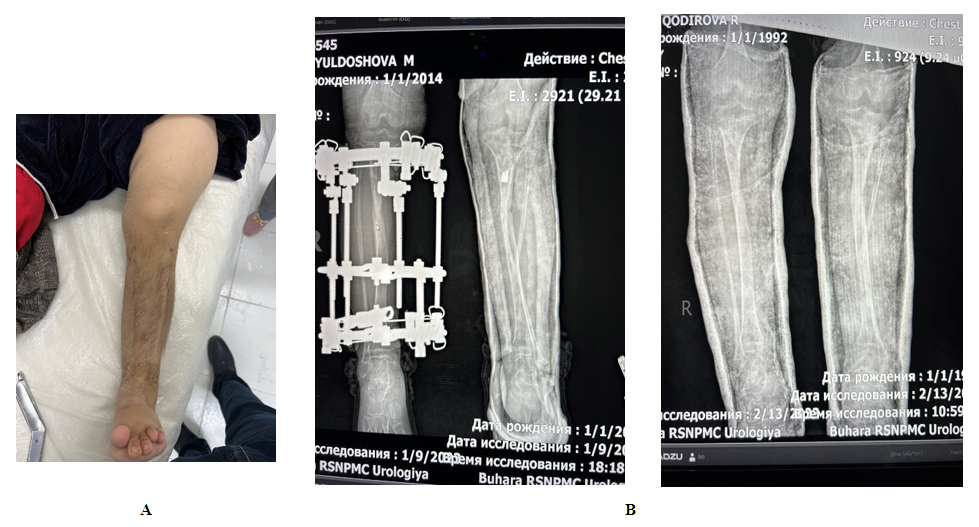 | Figure 2. Photos and radiographs of the legs of patient M. (ICSB No. 8404) after lengthening the segments of the lower extremities: a, b – photos and radiographs of the legs after removal of the device |
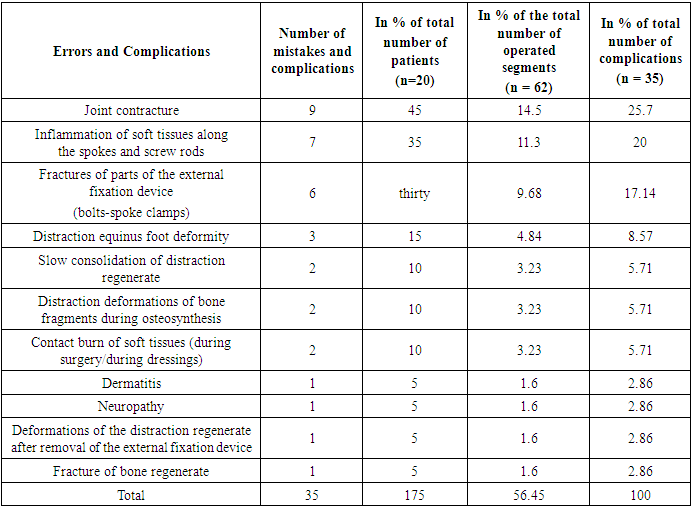
We assessed the clinical significance of negative events according to the classification of Paley D. (1999) with clarification of their percentage ratios to the number of patients and operated segments. According to the criteria of this classification, negative events were divided according to the degree of their negative impact on the treatment process and the final result of treatment. We classified negative events that were reversible and quickly eliminated by conservative methods as problems. We classified negative events that required additional surgical intervention, but did not have a negative impact on the final outcome of treatment, as obstacles. The category of complications included negative events that required surgical correction and reduced the quality of the final result (Table 3).Table 3. List of errors and complications, according to the classification of errors and complications Paley D. (1999) in patients of the main group
 |
| |
|
According to Table 3, the vast majorityout of 35 negative events (175% of the number of treated patients and 56.45% of the number of operated segments) in 32 cases (160% of the number of treated patients and 51.6% of the number of operated segments) were attributed to problems, in one case (5% of the number of treated patients and 1.6% of the number of operated segments) to obstacles and only two observations (10% of the number of treated patients and 3.2% of the number of operated segments) were classified as complications. More than 90% of all negative situations observed in the main group were reversible and temporary.During the fixation period, we more often encountered inflammation of the soft tissues along the wires and rods-screws - 4 patients (11.4% of the total number of errors and complications), which can be explained by several factors: a decrease in both general and local immunity, an increase in interstitial swelling of the tissues of the segment being lengthened, decreased stability of the device, and difficulty in carrying out hygienic procedures.During the period after removal of the device, we encountered complications that affected the final result of the treatment. One patient (2.9% of the total number of errors and complications) experienced a deformation of the distraction regenerate, and another patient (2.9% of the total number of errors and complications) experienced a fracture of the bone regenerate. And if a fracture of the bone regenerate cannot be predicted, then deformation of the distraction regenerate can be easily prevented by following the recommendations of this period.
4. Conclusions
1. Thus, after analyzing errors and complications, we identified the most risky periods of treatment in terms of the likelihood of unforeseen negative situations, and also characterized each period of treatment in terms of the errors and complications inherent in them.2. Transosseous osteosynthesis with an external fixation device according to Ilizarov allowed the doctor to eliminate the problems, preventing their negative development and transition into complications.
References
| [1] | Unstressed corticotomy (experimental study) / V. I. Shevtsov, S. A. Erofeev, N. V. Petrovskaya, A. M. Chirkova, B. I. Litvinova // Genius of orthopedics. - 1999. - N 4. - P. 24-27. Key words (non-standardized): biomechanics - transosseous osteosynthesis - reparative regeneration - bone. |
| [2] | Ilizarov G. A. Closed osteotomy of tubular bones in an experiment [Text] / G. A. Ilizarov, A. A. Shreiner // Theoretical and practical aspects of transosseous compression and distraction osteosynthesis: abstract. report All-Union scientific-practical conf. (Kurgan, June 22-23, 1976). - Kurgan, 1976. - pp. 38-40. |
| [3] | Ilizarov, G. A. Corrective osteotomy with anatomical lengthening of the lower limb / G. A. Ilizarov // 13th anniversary regional scientific conference dedicated to the 300th anniversary of the city of Kurgan: [collection. scientific tr.] / Kurgan. region scientific about surgeons. - Kurgan, 1963. - [Vol. 4.]. - pp. 355-358. Key words (unstandardized): methodology. |
| [4] | Ilizarov G. A.Elimination of deformities according to Ilizarov: dependence of the result of fragment rotation on the location of the axis of rotation, level and direction of osteotomy / G. A. Ilizarov // Ilizarov method: theory, experiment, clinic: abstract. report All-Union conf., dedicated 70th anniversary of G. A. Ilizarov. - Kurgan, 1991. - pp. 296-298. |
| [5] | Orlyansky V.Corrective osteotomies in the area of the knee joint / V. Orlyansky, M. Golovakha, R. Shabus. - Dnipropetrovsk: Thresholds, 2009. - 159 p. |
| [6] | Savchenko N. I.Corticotomy in the upper third of the tibia // Method of transosseous osteosynthesis in the treatment of patients with diaphyseal fractures of the femur and tibia bones of the same limb / N. I. Savchenko. - Mariupol: [b. i.], 2006. . - pp. 147-156. |
| [7] | Shevtsov V. I.Methods of treating patients with combined deformities of the bones of various parts of the foot // Transosseous osteosynthesis in foot surgery: handbook. for doctors / V. I. Shevtsov, G. R. Ismailov. - M.: Medicine, 2008. – P. 112-148. Key words (unstandardized): osteotomy- methods. |
| [8] | Shevtsov V. I.Method for eliminating deformities of long tubular bones / V. I. Shevtsov, A. A. Shreiner, K. N. Smelyshev // Genius of Orthopedics. - 2000. - N 1. - P. 104-107. Key words (unstandardized): correction - corticotomy - experiment. |
| [9] | Shreiner, A. A.Closed osteotomy of long tubular bones according to G. A. Ilizarov in an experiment / A. A. Shreiner // 1st med.-biol. conf. young scientists of Kurgan: abstract. report - Kurgan, 1976. - pp. 82-84. |
| [10] | Support osteotomies according to Ilizarov/ E. A. Volokitina, L. N. Solomin // Fundamentals of transosseous osteosynthesis: [in 3 volumes] / ed. prof. L. N. Solomina. - 2nd ed., revised. and additional - M.: Binom, 2015.- T. 3. - P. 1117-1132. |
| [11] | Novikov, K. I. Lengthening of the femur in children and adolescents with achondroplasia: dis... cand. honey. Sciences / K. I. Novikov; Ministry of Health of the Russian Federation. RRC "WTO" named after. acad. G. A. Ilizarova. – Kurgan, 2001. – 202 p. |
| [12] | Planning corrective osteotomy of the femur using 3D modeling. Part I / Baindurashvili Alexey Georgievich, Baskov Vladimir Evgenievich, Filippova Anastasia Viktorovna, Bortulev Pavel Igorevich, Barsukov Dmitry Borisovich, Pozdnikin Ivan Yurievich, Voloshin Sergey Yurievich, Baskaeva Tamila Vladimirovna, Poznovich Makhmud Stanislavovich // Orthopedics, traumatology and reconstructive surgery of children. 2016. No. 3. URL: https://cyberleninka.ru/article/n/planirovanie-korrigiruyuschey-osteotomii-bedrennoy-kosti-s-ispolzovaniem-3d-modelirovaniya-chast-i (date of access: 07/27/2023). |
| [13] | Planning corrective osteotomy of the femur using 3D modeling. Part II / Baskov Vladimir Evgenievich, Baindurashvili Alexey Georgievich, Filippova Anastasia Viktorovna, Barsukov Dmitry Borisovich, Krasnov Andrey Ivanovich, Pozdnikin Ivan Yurievich, Bortulev Pavel Igorevich // Orthopedics, traumatology and reconstructive surgery of children. 2017. No. 3. URL: https://cyberleninka.ru/article/n/planirovanie-korrigiruyuschey-osteotomii-bedrennoy-kosti-s-ispolzovaniem-3d-modelirovaniya-chast-ii (access date: 07/27/2023). |
| [14] | Lee, A.D. Guide to transosseous compression-distraction osteosynthesis / A. D. Lee, R. S. Bashirov. - Tomsk: Red Banner, 2002. Contents: Indications, types and technique of osteotomy for transosseous osteosynthesis of pseudarthrosis and long bone defects. - P. 160 Ilizarov osteotomy technique. - P. 161. |
| [15] | Ilizarov G.A. Basic principles of transosseous compression and distraction osteosynthesis / G.A. Ilizarov // Orthopedics, traumatology and prosthetics.-No. 11. -1971. -P. 7-15. |
| [16] | A comparison of two osteotomy techniques for tibial lengthening / L. Eralp [et al.] // Arch. Orthop. Trauma Surg. 2007. Vol. 124, No. 5. P. 298300. |
| [17] | Guidelines for safetybilateral tibial lengthening for stature / KI Novikov, KN Sudramanyam, E. S. Kolesnikova, OS Novikova, J. Jaipuria // JLLR. - 2017. - Vol. 3, No. 2. - P. 93-100. - DOI: 10.4103/jllr.jllr_7_17. |
| [18] | A technique of percutaneous multidrilling osteotomy for limb lengthening and deformity correction / N. Yasui [et al.] // J. Orthop. Sci. 2000. Vol. 5, No. 2. P. 104-107. |
| [19] | Bari Mofakhkharul, Shahidul Islam, Shetu Nazmul Huda, Mahfuzer Rahman D. Reconstruction of bone loss of diaphyseal tibial bones using GA Ilizarov technique // Genius of Orthopedics. 2015. No. 2. |
| [20] | Tibial Lengthening Using a Fixator-Assisted Lengthening Plate: A New Technique. Tosun HB, Agir I, Gumustas S, Serbest S, Uludag A, Celik S. Trauma Mon. 2016 Mar 30; 21(5): e25340. doi:10.5812/traumamon.25340. eCollection 2016 Nov. PMID: 28184364. |
| [21] | Radiomorphological Manifestations of Femoral and Tibial Cortical Bones at Different Stages of Limb Lengthening. Diachkova GV, Novikov KI, Diachkov KA, Rohilla R, Wadhwani J. Indian J Orthop. 2019 Jul-Aug; 53(4): 567-573. doi: 10.4103/ortho. IJOrtho_443_18. PMID: 31303674. |
| [22] | Acute Shortening and Re-Lengthening (ASRL) in Infected Non-union of Tibia - Advantages Revisited. Baruah RK, Baruah JP, Shyam-Sunder S. Malays Orthop J. 2020 Jul; 14(2): 47-56. doi: 10.5704/MOJ.2007.012. PMID: 32983377. |
| [23] | Circular external fixation in tibial nonunions. García-Cimbrelo E, Martí-González JC. Clin Orthop Relat Res. 2004 Feb; (419): 65-70. PMID: 15021133. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML