-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 473-476
doi:10.5923/j.ajmms.20241402.63
Received: Jan. 6, 2024; Accepted: Jan. 23, 2024; Published: Feb. 22, 2024

Methods of Reconstructive Operations for Neurotrophic Ulcers in Spinal Patients
Matmuratov K. J., Khalikova O. M., Parmanov S. A.
Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The objective of this research was to examine the clinical progression of neurotrophic ulcers in the hip area of individuals with spinal conditions via the optimization of cosmetic surgical procedures. Materials and methods: This study analyzed the outcomes of inpatient treatment for 11 patients with neurotrophic ulcers of the hip. These patients had post-traumatic spinal cord lesions and had previously undergone unsuccessful conservative treatment. The analysis was conducted at the Pulmonary Surgery and Surgical Complications Division of Diabetes at the Multidisciplinary Clinic of the Tashkent Medical Academy between 2020 and 2023. Results: The specially selected patients had reconstructive and plastic surgery. Concurrent diseases, patient constitution, and wound defect extent were studied. The data analysis indicated that all patients had a complication-free recovery after surgery, and their wounds healed without any excessive strain. Conclusion: The selection of a surgical approach tailored to each individual patient with neurotrophic ulcers in the buttocks and cranial areas is crucial for achieving a positive surgical outcome in the immediate postoperative period.
Keywords: Neurotrophic ulcers, Spinal patients, Cosmetic surgical procedures
Cite this paper: Matmuratov K. J., Khalikova O. M., Parmanov S. A., Methods of Reconstructive Operations for Neurotrophic Ulcers in Spinal Patients, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 473-476. doi: 10.5923/j.ajmms.20241402.63.
Article Outline
1. Actuality
- Major harm to the spinal cord in the majority of patients, ranging from 70% to 90%, is further worsened by the presence of lining. This lining is a result of serious problems in the nerve supply to the soft tissues, a significant deterioration in the functioning of the nerves, and a near-total lack of preventive measures for these difficulties. The presence of infection and other detrimental factors results in compromised immune function in individuals, which in turn contributes to the development of purulent wounds [3]. The primary factors leading to deaths in this group of individuals are leprosy and urinary tract infections [4]. Several recent investigations on individuals with spinal cord injuries have identified peritoneum as a neurotrophic disease. This highlights the absence of nerve supply in the damaged region, the reduced resilience of tissues, and their limited ability for restorative regeneration [2]. The lobe is characterized by a disruption of the skin's trophic and protective qualities, which occur as a result of tissue hypoxia, regardless of the underlying etiology. Prolapses often occur in regions where tissues experience significant and persistent pressure, particularly in the vicinity of the subcutaneous bone prominences. When a person is laying down, the parts of the body that suffer the most pressure (measured at 40-60 mm Hg/st) are the coccyx, buttocks, heels, and occiput. The findings from tests investigating the extent to which external influences compress objects indicate that subjecting tissues to a consistent pressure of 70 mm Hg over a duration of two hours induces irreversible alterations. Simultaneously, when the pressure is halted every 5 minutes, there are negligible alterations in the tissues that do not result in consequences. There is a significant body of literature by writers from both local and international origins that focuses on the management of leprosy. According to the majority of experts, conservative therapies are becoming acknowledged as unsustainable since they are lengthy and have little impact. Several studies on the surgical treatment of the spleen provide unclear information about the use of various plastic procedures to close spleen abnormalities in different regions [5].Contemporary literature places emphasis on the prevention of neurotrophic ulcers. This involves the development of risk scales and the establishment of regulations and guidelines for treatment. Nevertheless, the prevalence of neurotrophic ulcers among hospitalized patients remains substantial, ranging from 75% to 80% [6]. Prolegies are difficult to treat and often worsen or reoccur, leading to major limitations and delays in rehabilitation efforts, prolonged hospital stays, and an increased risk of septic complications.The aforementioned evidence highlights the necessity of selecting the most effective strategies for surgical and non-surgical interventions in patients with spinal cord injuries who have neurotrophic ulcers. It is crucial to consider the specific location of the neurotrophic ulcer, as this can directly impact the time required for wound healing and recovery. The objective of this research was to examine the clinical progression of neurotrophic ulcers in the hip area of individuals with spinal conditions via the optimization of cosmetic surgical procedures.
2. Materials and Methods of Research
- This study analyzed the outcomes of inpatient treatment for 11 patients with neurotrophic ulcers of the hip. These patients had post-traumatic spinal cord lesions and had previously undergone unsuccessful conservative treatment. The analysis was conducted at the Pulmonary Surgery and Surgical Complications Division of Diabetes at the Multidisciplinary Clinic of the Tashkent Medical Academy between 2020 and 2023. Upon admission to the clinic, all patients had a comprehensive clinical and instrumental X-ray examination in order to rule out the presence of osteomyelitis. Patients had infusion therapy in conjunction with antimicrobial treatment. There were five males, accounting for 62.5 percent of the total, and three females, accounting for 37.5 percent. The majority of individuals were between the age range of 20 to 40 years. The neurotropic ulcers varied in size from a few centimeters to 10-15 cm in diameter. They exhibited the characteristics of a long-lasting skin ulcer, with hard and uniform margins that were covered with granulations. Out of the total of 8 patients, 6 (75%) had the symptoms concentrated in the buttock area, while the remaining 2 (25%) had them in the cross region. Not all individuals had osteomyelitic lesions in the underlying bone. The majority of individuals had lower paraplegia without any signs of conductor-type sensitivity. The surgical procedure was carried out following preoperative measures, which involved administering appropriate antibiotics based on a bacteriological examination of the pelvic microflora and its susceptibility to antibiotics. Additionally, efforts were made to restore the body's electrolyte, water, and protein balance, as well as to detoxify and sanitize the pelvis through necrectomy, enzyme treatments, and antiseptic applications. The primary indicators of the surgeon's readiness were the existence of granulations across the whole surface, the lack of necrotic tissue, and indications of wound poisoning. To address significant gaps in the buttock region, cosmetic surgery was performed using a technique involving the displacement of skin and muscle. For tiny wounds, a surgical incision was made, followed by the subsequent healing of the wound surface by the surrounding tissues.
3. Results and Discussion
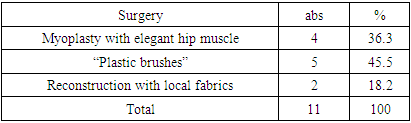
- The specially selected patients had reconstructive and plastic surgery. Concurrent diseases, patient constitution, and wound defect extent were studied.Due to the seriousness of the wound defect, half of the patients were provided with a prosthetic that resembled a mouth. A patient had a procedure in which the fistula was incised to its base and filled with plastic material using local tissues, thereby closing the deep fistula opening. When the defect was identified in the lower region of the buttock, namely around the hip and thigh crease, myoplasty was conducted using a delicate hip muscle. This was done to address the local tissue shortage and avoid the reoccurrence of trophic ulcers (table.1.).
|
4. Clinical Observation
- The patient's name is N.A., born in 1989, and has the identification number 13558/1964. In May 2020, he had a fall from a 6-meter height during construction, leading to a fracture in the body of the L1 vertebra and instant amputation of his legs. In August 2020, he had spinal surgery including the implantation of a metallic structure. In 2021, a surgical procedure was conducted to extract metallic constructs from the spinal column. No positive neurological signs were detected after these procedures. In July 2023, a medical illness manifested in the left buttock area. The individual had treatment at a hospital and continued to get care as an outpatient at their place of residence. Due to the incurable nature of a neurotrophic ulcer, he was admitted to the department of purulent surgery and surgical consequences of diabetes mellitus at the multidisciplinary clinic of the Tashkent Medical Academy. He had symptoms of asthenia, splenomegaly in the left gluteal region, immobility, and hypoesthesia in the lower extremities.
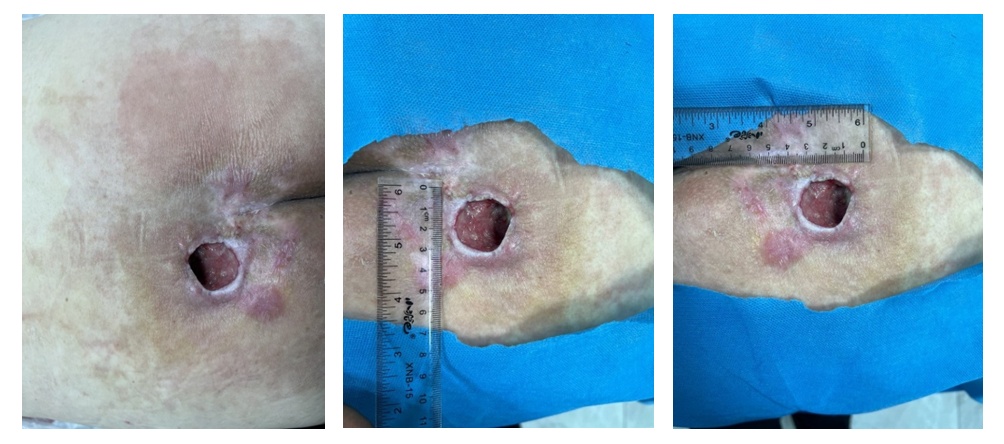 | Figure 1. Conditions of protrusion in the left buttock region at the time of admission |
 | Figure 2. Excision and plastics of neurotrophic ulcer |
 | Figure 3. Postoperative period – wound healing with primary tension |
5. Discussion
- Wound abnormalities that occur due to impaired neurotrophic function in soft tissues exhibit distinct characteristics throughout their progression. The primary factor is the quick intensification of the process and the development of internal shell or granular tissue, resulting in the prolonged progression of the wound process. Neurotrophic ulcers primarily occur in people with reduced sensitivity, and are characterized by the presence of an internal inflammatory roller. For such situations, it is necessary to use a personalized surgical method and adopt a cautious therapeutic approach. No instances of recurrence were seen in our patients for a duration of 3 months. The primary objective of the surgeon doing surgery on such patients is to avoid the occurrence of relapses. Regrettably, in the majority of instances, we see a reoccurrence of a neurotrophic ulcer in the surgically treated region. The causative element that contributed to this issue is crucial in attaining a successful surgical wounds in spinal patients and analyzing the unsatisfactory outcomes, we decided to carry out several reconstructive-plastic surgeries based on the specific location of the wound defect. From our perspective, this issue requires more investigation before definitive conclusions can be drawn.
6. Conclusions
- 1. The selection of a surgical approach tailored to each individual patient with neurotrophic ulcers in the buttocks and cranial areas is crucial for achieving a positive surgical outcome in the immediate postoperative period.2. Secondary reconstructive-plastic surgery is necessary to avoid the development of pus-filled problems and to enlarge the wound defect in patients with neurotrophic ulcers after spinal cord damage.3. Further contemporary research is needed to enhance the quality of life for individuals with post-traumatic spinal cord injuries by establishing criteria for predicting the occurrence of neurotrophic ulcers in the cranial and hip areas.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML