-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 471-472
doi:10.5923/j.ajmms.20241402.62
Received: Feb. 6, 2024; Accepted: Feb. 21, 2024; Published: Feb. 22, 2024

The Correlation of Laboratory Parameters in Patients with Hypothyroidism and Chronic Migraine
Kambarova D. N.1, Usmanova D. D.2
1Andijan State Medical Institute, Uzbekistan
2Tashkent Pediatric Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Migraine is a neurovascular disorder characterized by persistent headache of moderate or severe intensity, unilateral localization and throbbing pain lasting from hours to days, often combined with nausea, vomiting, photophobia, phonophobia and increasing with physical exertion.
Keywords: Hypothyroidism, Migraine, Diagnosis, Thyroid hormones
Cite this paper: Kambarova D. N., Usmanova D. D., The Correlation of Laboratory Parameters in Patients with Hypothyroidism and Chronic Migraine, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 471-472. doi: 10.5923/j.ajmms.20241402.62.
Article Outline
1. Relevance
- Research is being conducted around the world aimed at identifying the causes of headaches, their early diagnosis and achieving a highly effective approach to treatment tactics. In this regard, identifying the causes, risk factors for migraine, factors for the development and prevention of complications of the disease, eliminating neuropsychological, neurovegetative maladjustment, identifying biochemical disorders when the disease occurs, as well as improving treatment and prevention methods are recognized as an urgent problem. [1,6,9,12]. Migraine is commonly found in comorbidity with various diseases such as epilepsy, myocardial infarction, stroke, fibromyalgia, bronchial asthma and depression [2,7,10,11]. Recently, literature sources have appeared indicating that migraine can be a powerful risk factor for the development of both overt and subclinical hypothyroidism.Hypothyroidism, defined as the clinical condition of moderately elevated serum TSH levels (up to 10 mcg/l subclinical hypothyroidism and more than 10 mcg/L manifest hypothyroidism) at normal or reduced levels of FT4 and FT3, is a much more common and asymptomatic disease than overt hypothyroidism [1,4,9]. It is diagnosed in 1-10% of the adult population. It shows a higher prevalence among women and the elderly [2,3,5,8]. Hypothyroidism, characterized by changes in cardiovascular and neuromuscular functions and lipid metabolism, may be the first phase or the beginning of a progressive painful condition, as well as migraines [8,12].Objective: to determine the significance of thyroid hormones in the development and diagnosis of chronic migraine.
2. Research Materials and Methods
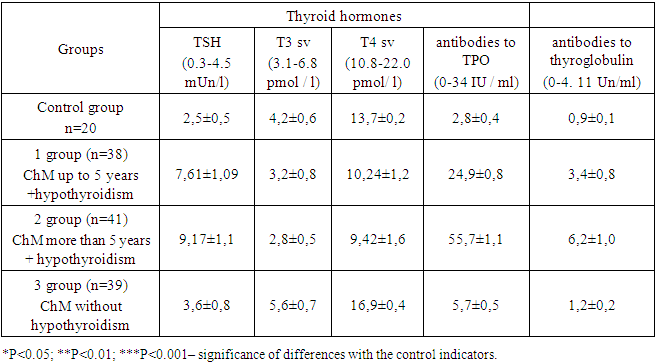
- 118 patients with chronic migraine (ChM) were included in the study. The diagnosis of migraine was made according to the International Classification of Headaches (ICHD-III).The patients were divided into 3 groups. Group 1 consisted of 38 patients with ChM with headache duration up to 5 years and hypothyroidism. Group 2 included 41 patients with ChM with headache duration of more than 5 years and hypothyroidism. Group 3 consisted of 39 patients with HM without hypothyroidism. A control group was also created, which included 20 practically healthy individuals. Some patients applied to the polyclinic for outpatient treatment. Some patients were treated in the departments of neurology and endocrinology of the clinic of the Andijan State Medical Institute from 2022-2023. The concentration of TSH in blood plasma, free T3 and T4 was determined by enzyme immunoassay on an analyzer of the company "Oxis" (USA) using test systems of the company "Diagnostic Systems" (Nizhny Novgorod).
3. The Results of the Study
- In the control group, thyroid hormone levels were as follows: TSH 2.5±0.5 mED/l, T3 free - 4.2±0.6 pmol/L, T4 free - 13.7±0.2 pmol/L, antibodies to TPO 2.8±0.4 IU/ml, antibodies to thyroglobulin 0.9±0.1 Units /ml.In group 1 patients with ChM under 5 years of age and hypothyroidism, the indicators were equal: TSH 7.61±1.09 mED/L, T3 free - 3.2±0.8 pmol/L, T4 free - 10.24±1.2 pmol/L, antibodies to TPO 24.9±0.8 IU/ml, antibodies to thyroglobulin 3.4±0.8 Units/ml.In patients of group 2 with HM for more than 5 years and hypothyroidism, the indicators were equal: TSH 9.17±1.1 mED/l, T3 free - 2.8±0.5 pmol/L, T4 free - 9.42±1.6 pmol/L, antibodies to TPO 55.7±1.1 IU/ml, antibodies to thyroglobulin 6.2±1.0 U/ml. In patients of group 3 with HM without hypothyroidism, the indicators were consistent: TSH 3.6±0.8 mED/l, T3 free - 5.6±0.7 pmol/L, T4 free - 16.9±0.4 pmol/L, antibodies to TPO 5.7±0.5 IU/ml, antibodies to thyroglobulin 1.2±0.2 Units /ml.Analyzing the results obtained (Table 1) it can be concluded that all patients of group 1 had subclinical hypothyroidism, while 9 (22%) patients of group 2 had manifest hypothyroidism, and 32 (78%) patients of group 2 had subclinical hypothyroidism. There were no deviations from the norm in patients of group 3, i.e. all thyroid hormones were within the reference values.
|
4. Conclusions
- Chronic migraine has an adverse effect on thyroid function. The revealed manifest and subclinical hypothyroidism in patients confirms this fact. Pathogenetically, thyroid-stimulating hormone begins to increase due to the occurrence of neurohumoral changes observed in migraines.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML