-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 441-449
doi:10.5923/j.ajmms.20241402.57
Received: Feb. 7, 2024; Accepted: Feb. 19, 2024; Published: Feb. 22, 2024

Clinical and Immunological Justification of the Choice of Methods for the Prevention of Purulent-Septic Complications of Liver Echinococcosis
Safarov Sunnat Sattorovich, Khamdamov Bakhtiyor Zarifovich, Abdurakhmanov Mamur Mustafayevich, Khamdamov Alisherjon Bakhtiyorovich
Bukhara Medical Institute named after Abu Ali Ibn Sina, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The literature and own data on modern methods of surgical treatment and clinically and immunologically sound methods of choosing the prevention of purulent-septic complications in patients with echinococcosis of the liver, corresponding to the principles of evidence-based medicine, are summarized. Along with this, new algorithms of therapeutic and diagnostic tactics for non- and complicated forms of hydatidous echinococcosis of the liver are described in detail.
Keywords: Echinococcosis, Liver, Immunity
Cite this paper: Safarov Sunnat Sattorovich, Khamdamov Bakhtiyor Zarifovich, Abdurakhmanov Mamur Mustafayevich, Khamdamov Alisherjon Bakhtiyorovich, Clinical and Immunological Justification of the Choice of Methods for the Prevention of Purulent-Septic Complications of Liver Echinococcosis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 441-449. doi: 10.5923/j.ajmms.20241402.57.
1. Introduction
- Advances in the use of antibacterial drugs could not affect the eradication of purulent-septic complications [1,3,5,13,14]. And in recent years, such complications have not tended to decrease [2,4,6,15,16,17]. At the same time, in the general structure of mortality in surgical hospitals, purulent-septic complications remain the leading ones [7,9,18,19,20,21].The development of purulent-septic complications of echinococcosis and echinococcectomy lead to a significant increase in the duration of treatment, an increase in the incidence of disability and mortality, which on average varies between 7.2-10.8% [8,10,12,22,23,24,25]. In this regard, the prognosis and prevention of complications in surgery for echinococcosis of the lungs and liver is still far from being solved and relevant.It is known that echinococcus, developing in the human body, which acts as an intermediate host, significantly affects the restructuring of the immune system [11,26,27,28]. The mechanism of these changes has not been sufficiently studied to date. Many studies of the relative immune response of the body to the invasion of echinococcus are multidirectional, sometimes even contradictory to each other. There is an opinion that, once in the body, echinococcus stimulates the host's immune system. This is manifested by the development of a number of cellular and humoral reactions. Along with this, there is information about the suppression of immunity. Proponents of this theory argue that the suppression of the host's defense mechanisms against both their own antigens (homologous immunosuppression) and the antigens of other agents infecting organisms (heterologous immunosuppression).There is no data in the literature on the effect of initial changes in the immunological status of patients with echinococcosis on the frequency and severity of purulent-septic complications and the dynamics of changes in immunological parameters in the postoperative period.Postoperative purulent-septic complications in surgery of echinococcosis of the liver are extremely severe, existing methods and methods of prevention are ineffective [29,30,31,32]. Evaluation of existing and development of new methods for predicting the development of possible purulent-septic complications, which is important for the effective and rational rehabilitation of patients with echinococcosis, could significantly improve the results of treatment of patients with echinococcosis of human internal organs. All of the above has determined the main direction of this work.The purpose of the study. Improvement of methods for the prevention of purulent-septic complications of echinococcosis.
2. Materials and Methods
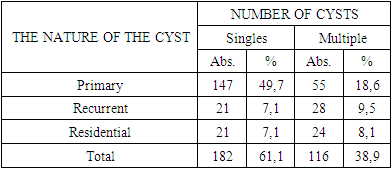
- The main group included 296 patients with liver echinococcosis who were treated and examined at the Bukhara Regional Multidisciplinary Medical Center from 2016 to 2022. The distribution of patients by age revealed the predominance of patients in the age range from 41 to 60 years (69.5%), that is, during the period of active labor activity. At the same time, the range of age variance of patients in the main group, compared with the control group, decreased both towards young and elderly age. A separate comparative analysis showed that among male patients, patients in the age category from 41 to 50 years (37.8%) prevailed, followed in descending order by patients in the age range from 51 to 60 years (21.0%) and from 61 to 70 years (17.6%). At the same time, among female patients, the prevalence in the age range was also from 51 years to 60 years (46.3%). In comparison with patients of the control group, it can be noted that the prevalence in the main group of the number of patients was only in the age range from 41 to 50 years (1.1 times), from 61 to 70 years (2.1 times) and over the age of 71 years (1.4 times). Lower values in the number of patients in the main group, compared with the control group, were noted by us in the age categories younger than 20 years (3.5 times less), in the range from 21 to 30 years (2.2 times) and in the range from 31 to 40 years (1.6 times). Thus, a comparative analysis of the distribution of patients with hydatidous echinococcosis of the liver in the main group of patients showed an excess of the older contingent with the same gender values. A comparative assessment of the distribution of patients by the nature of the disease and the number of cysts showed (Table 1) that patients with a residual solitary echinococcal cyst (1.9 times), with multiple residual echinococcal cyst (1.6 times) and with a solitary recurrent cyst (1.2 times) prevailed in the main group of patients.
|
3. Results and Their Discussion
- In patients with primary hydatidous echinococcosis of the liver in the preoperative period, a compensated degree of immunological suppressiveness was diagnosed in 51.0% of cases (103 patients). Of these, patients with single echinococcal liver cysts were in priority (5.1% more). To a lesser extent, 62 patients (30.7%) were diagnosed with a subcompensated degree of immunological suppressiveness. Its distribution was also in favor of patients with a single echinococcal cyst of the liver (more by 4.7%). In 35 (17.3%) patients with primary hydatidous echinococcosis of the liver, a decompensated degree of immunological suppression was diagnosed in the preoperative period. At the same time, it was detected to a greater extent among patients with primary multiple hydatidous echinococcosis of the liver (11.2% more cases). It remains unclear whether there are any violations in immunological suppressiveness among 2 patients with primary single hydatidous echinococcosis of the liver. This was probably due to the small size of the cyst, which did not reach 5 cm. Thus, the degree of immunological suppressiveness among patients of the main group with primary hydatidous echinococcosis of the liver showed the predominance of a compensated degree of immunological suppressiveness. Along with this, other degrees were noted in this cohort of patients, which may have been due to the presence of purulent-septic complications, which were characterized by a severe course against the background of immunological suppression of the body. Nevertheless, in the majority of patients with primary both single and multiple hydatidous echinococcosis of the liver, transient disorders in the immune system were prevalent. In the main group, 45 cases with residual echinococcal liver cyst were diagnosed. Patients with multiple echinococcosis of the liver prevailed (by 6.6% more). An assessment of the degree of immunological suppression among patients with residual echinococcal liver cyst showed that in more than half of the cases (55.6%), decompensation was diagnosed in the studied parameters. Almost 2 times of these patients were among cases with multiple liver cysts (1.55 times more).In 42.2% of cases, patients were diagnosed with a subcompensated degree of immunological suppression, which prevailed among patients with single echinococcal liver cysts. In another 1 (2.2%) patient with a residual echinococcal cyst of the liver, the degree of immunological suppression was at the compensation level. Such a case was diagnosed among patients with a single hydatidous echinococcal cyst of the liver. Thus, in patients with residual liver echinococcosis, the decompensated level of immunological suppressiveness becomes a priority, which exceeds the subcompensated level by almost 2 times among patients with multiple liver echinococcosis. Against this background, the subcompensated variant of immunological suppressiveness is superior in patients with single hydatidous echinococcal liver cysts.A recurrence of hydatidous echinococcosis of the liver was diagnosed in 49 patients of the main group. The distribution of patients depending on the degree of immunological suppression revealed, in contrast to previous cases of the study, clear distinctive sides. However unusual it may be, there were more patients with multiple echinococcal liver cysts than with single ones. The majority of patients (89.9%) had decompensated immunological suppressiveness, which was leading among both patients with single and patients with multiple liver echinococcosis. Moreover, in the latter case, there were more such patients by only 7.2% of the case. Only in 5 (10.2%) cases, a subcompensated form of immunological suppressiveness was diagnosed among patients with a recurrent form of liver echinococcosis. Moreover, it was almost identical both among patients with single and multiple echinococcal liver cysts. We have not identified patients with a recurrent form of hydatidous echinococcosis of the liver with a compensated degree of immunological suppressiveness. Thus, in patients with recurrent hydatidous echinococcosis of the liver, the decompensated degree of immunological suppression is a priority, which, as shown by statistical analysis, was at a priority level. Against this background, it should be noted the absence of a compensated form of immunological suppressiveness, which occurred in previous subgroups of patients (with primary and residual forms). Apparently, this is due to the peculiarities of the manifestation of purulent-septic complications of liver echinococcosis and this analysis attracted our attention. In 51.0% of patients, hydatidous echinococcosis of the liver was complicated. Among the complicated forms of liver echinococcosis, cases with banal cyst suppuration (60.3%) and cyst suppuration with a breakthrough into the intrahepatic bile ducts with the development of cholangitis and jaundice (31.1%) prevailed. A complication in the form of suppuration of an echinococcal cyst with a breakthrough into the pleural cavity in 7 (4.6%) patients led to the development of pleural empyema. A similar nature of the lesion, but without pleural complications, led to a cyst breakthrough into the bronchial tree with the development of purulent endobronchitis was noted by us in 1 (0.7%) patient. In 6 (3.3%) patients, the complication of an echinococcal cyst was in the form of its breakthrough into the free abdominal cavity with the development of peritonitis. Along with the analysis of complications similar to the control group of patients, we also conducted an analysis of the distribution of the degree of immunological suppression among patients with complicated and uncomplicated forms of hydatidous echinococcosis of the liver. A preliminary summary analysis showed that patients in the main group had the same proportion of patients with compensated and decompensated degrees of immunological suppressiveness (35.1%, respectively; 104 patients each). Only in 29.1% (86 patients) of cases in patients of the main group was a subcompensated degree of immunological suppressiveness diagnosed. Among patients with a complicated form of liver echinococcosis, the decompensated degree of immunological suppressiveness (58.9%) was preferred, whereas among patients with an uncomplicated form of the disease, only 10.3% (15 patients) turned out to be such. The same imbalance was noted among patients with subcompensated immunological suppression. A subcompensated form of the degree of immunological suppression was noted among 41.1% (62 patients) of patients with a complicated form of the disease, whereas in the subgroup of patients where there was no complication of liver echinococcosis, only 16.6% (24 patients) turned out to be such. Among patients with a complicated form of liver echinococcosis, we did not detect any other changes in the degree of immunological suppressiveness, whereas among patients with an uncomplicated form of the disease, 104 (71.7%) patients with compensated and 2 patients (1.4%) with a normal level of immunological suppressiveness of the body were identified. The peculiarities of therapeutic measures in patients with a complicated form of liver echinococcosis is an approach to the choice of surgical intervention, which differs both in technical issues of solving the problem and in the timing of surgical interventions. As for the uncomplicated forms of hydatidous echinococcosis of the liver, surgical interventions in such patients should be completed without the possibility of developing purulent-septic complications, relapses and residual cysts in various periods after surgery. Therefore, before proceeding to the development of a therapeutic and diagnostic algorithm, we resorted to another comparative analysis of the distribution of patients with uncomplicated liver echinococcosis (145 patients) and the degree of immunological suppressiveness.The approach to the separation of patients with uncomplicated form of hydatidous echinococcosis of the liver was based on WHO criteria from 2010. All these criteria were described by us in the second chapter of the dissertation, and they were based on ultrasound data.In general, among those with an uncomplicated form of hydatidous echinococcosis of the liver, patients with hydatidous echinococcal cyst in the CL and CE-4 stages were the most. At the same time, if in the first case (31 patients; 21.4%), they were characterized by the presence of ultrasonic signs of a single-chamber cystic formation, usually spherical or oval in shape, with unclear homogeneous anechoic contents limited by a hyperechoic rim without visible walls, then in the second case (35 patients; 24.1%) - heterogeneous-hypoechoic or dysgomogenously-degenerative contents and the absence of daughter cysts. In patients with CL, it was hydatidous echinococcosis of the liver, referred to simply as "cystic formation". In these patients, in 93.5% of cases (29 patients), the degree of immunological suppression was compensated. The remaining 6.5% of patients (2 cases) were diagnosed with a subcompensated degree of immunological suppressiveness. At the same time, only compensated forms of immunological suppression were diagnosed in patients with sonographic signs of hydatidous echinococcosis of the liver CE-4. Ultrasound examination revealed the presence of a cyst with daughter cysts in 29 patients with hydatidous echinococcosis of the liver. At the same time, the contents were anechoic with simultaneous detachment of the inner cyst shell. The cyst shell gave out the sign of a "water lily". At the same time, in 18 patients of this subgroup, the single-chamber cyst contained daughter cysts that had an anechoic image in the form of a complex mass due to the presence of periodic echogenic sites. All these patients were identified by us in a subgroup with ultrasound signs of hydatidous echinococcosis of the liver CE-3. The lion's share of patients (96.6%) had a compensated degree of immunological suppressiveness and 1 patient (3.4%) had a subcompensated degree. Such a high level of patients with compensated immunological suppressiveness was due to the transitional or intermediate period of death of the parasite, both maternal and daughter cysts. However, these cysts still contained viable protoscolexes.Patients with ultrasound signs CE-1 and CE-2 were in the same proportion (24 patients in each subgroup). In both the first and second cases, hydatidous echinococcosis of the liver was characterized by the presence of an active, living parasite. However, in the first case, patients revealed a single-chamber cystic formation of spherical or oval shape with homogeneous anechoic contents with clearly visualized cyst walls. In contrast to these signs, patients with CE-2 revealed multicameral cysts with multiple septa, in which daughter cysts completely filled the maternal cyst. Half of the patients (12 cases) with CE-1 signs of ultrasound pattern were patients with a subcompensated degree of immunological suppressiveness. A compensated degree of immunological suppressiveness was diagnosed in 11 (45.8%) patients with CE-1 signs of ultrasound pattern. Another 1 (4.2%) patient was diagnosed with a decompensated degree of immunological suppressiveness. In contrast to this subgroup of patients, patients with CE-2 ultrasound picture of hydatidous echinococcosis of the liver in 58.3% of cases were diagnosed with a decompensated degree of immunological suppression, in 9 patients (37.5%) – subcompensated and in 1 (4.2%) patient - compensated. Thus, a comparative analysis of the distribution of patients with an uncomplicated form of hydatidous echinococcosis of the liver according to the morphofunctional signs of the cyst and the degree of immunological suppression revealed a natural relationship between the phase and form of development of the pathological process and the severity of disorders in the immunological response of the body.The absence of any sign of immunological suppressiveness was diagnosed by us only among patients with CE-1, which was due to the presence of immunological competence, which made it possible not only to achieve the death of the parasite and stop the growth of the cyst, but also to create conditions for the abortive course of the entire pathological process, which led to calcification of hydatidous echinococcosis of the liver. A compensated degree of immunological suppressiveness was diagnosed, as already indicated in the previous paragraph of this chapter of the dissertation, in 104 patients with an uncomplicated form of hydatidous echinococcosis of the liver. At the same time, in 33.7% of cases (35 patients) these were patients with CE-4, in 27.9% of cases (29 patients) – patients with CL, in 26.9% of cases (28 patients) – patients with CE-3, in 10.6% of cases (11 patients) – patients with CE-1 and 1% (1 patient) – with CE-2. Thus, a compensated degree of immunological suppressiveness was typical for patients with developing and dead hydatidous echinococcosis of the liver. A subcompensated degree of immunological suppression in 50% of cases (12 patients) was characteristic of hydatidous echinococcosis of the liver with ultrasound signs of CE-1, in 37.5% of cases (9 patients) – for patients with CE-2, in 8.3% of cases (2 patients) - for patients with CL, and in 4.2% of cases (1 patient) – for patients with CE-3. Thus, a subcompensated degree of immunological suppressiveness was typical for patients with a live active parasite of hydatidous echinococcal cyst of the liver.The decompensated degree of immunological suppressiveness was diagnosed by us mainly (93.3%) among patients with ultrasound signs of hydatidous echinococcosis of the liver CE-2. Only 1 patient (6.7%) with ultrasound signs of hydatidous echinococcosis of the liver CE-1 showed a decompensated degree of immunological suppression. Thus, the decompensated degree of immunological suppressiveness was typical for patients with a live active multicameral parasite of hydatidous echinococcal cyst of the liver.In general, it should be noted that, as our comparative analysis has shown, the formation and development of hydatidous echinococcosis of the liver is based on the degree of manifestation of immunological suppressiveness. On the other hand, as already mentioned above, the development of immunological competence ends with the death of the parasite with the cessation of the development of echinococcosis and calcification of the cyst, which can be perceived as an adequate immunological response of the body. In this regard, preventive measures in patients with hydatidous echinococcosis of the liver should be aimed primarily at influencing immunological suppressiveness, transferring this violation of the system to the level of immunological competence. It seems to us that the solution of this issue should be reflected at all stages of providing medical and diagnostic care to the patient. The analysis of the distribution of the degree of immunological suppression in patients with a complicated form of hydatidous echinococcosis of the liver was carried out by separating patients depending on the presence of septic manifestations of the disease or identifying patients with the threat of sepsis.As already described above, 151 patients of the main group with hydatidous echinococcosis of the liver were diagnosed with a complication of the disease. We would like to remind you that among the complications in 60.3% of cases (91 patients), suppuration of hydatidous echinococcal cyst of the liver was noted, in 31.1% of cases (47 patients) – suppuration of hydatidous echinococcal cyst of the liver with a breakthrough into the intrahepatic bile ducts, with the development of cholangitis and jaundice, in 4.6% of cases (7 patients) – suppuration of hydatidous echinococcosis of the liver, with a breakthrough into the pleural cavity, followed by the development of pleural empyema. In 1 patient (0.7%), suppuration of an echinococcal cyst of the liver was diagnosed, with a breakthrough into the pleural cavity and further into the bronchial tree, with the development of purulent endobronchitis. Another 5 patients (3.3%) were admitted to the clinic with a complication of hydatidous echinococcosis of the liver in the form of its perforation into the abdominal cavity. Thus, all complications of hydatidous echinococcosis of the liver in patients of the main group can be divided both depending on the localization of the process and in the involvement of other organs and systems of the body, as well as emptying the focus of the pathological process due to the destructive destruction of the cyst. Intrahepatic complications of hydatidous echinococcosis of the liver were noted by us in 91.4% of cases (138 patients), which indicates the leadership of such variants of the manifestation of severe forms of this disease. In contrast, cases with a breakthrough of an echinococcal cyst were noted in 39.7% of cases (in 60 patients). This indicates the priority of purulent-inflammatory complications of hydatidous echinococcosis of the liver, which, as our experimental studies have shown, develop due to changes in the immunological response. Based on this, it is important, in our opinion, to know how much there is a comparative relationship between the development of purulent-septic complications of hydatidous echinococcosis of the liver and its clinical manifestations. The clinical manifestations of purulent-septic complications of hydatidous echinococcosis of the liver were based on signs of the syndrome of systemic inflammatory reactions, the manifestation of which is taken into account when assessing the severity of the inflammatory process. A comparative assessment of the distribution of the number of signs of systemic inflammatory response syndrome among patients with various types of purulent-inflammatory complications of hydatidous echinococcosis of the liver revealed that in 91 patients with cyst suppuration, the most (61.5%) was noted only on one sign of the syndrome. In second place (24.2%) were patients with two clinical and laboratory signs of systemic inflammatory response syndrome. At the same time, in 13 patients (14.3%), we did not notice signs of a systemic inflammatory reaction syndrome among patients with hydatidous echinococcosis of the liver, complicated by cyst suppuration. We did not identify patients with three and four signs of systemic inflammatory reaction syndrome in hydatidous echinococcosis of the liver, complicated by suppuration. In 47 patients (31.1%) with a complication of hydatidous echinococcosis of the liver in the form of cyst suppuration with a breakthrough into the intrahepatic bile ducts, with the development of cholangitis and jaundice, two (55.3%) and three (40.4%) clinical and laboratory signs of systemic inflammatory response syndrome were mainly noted. Only 2 (4.3%) patients showed only one of the four signs of systemic inflammatory response syndrome. More closely approximated to the clinical picture of the septic manifestation of the complicated form of hydatidous echinococcosis of the liver were noted by us in 7 (4.6%) patients with cyst suppuration, with its breakthrough into the pleural cavity followed by the development of pleural empyema. At the same time, in 57.1% of cases, three, and in 42.9% of cases, four clinical and laboratory signs of systemic inflammatory response syndrome were registered in patients. In 1 (0.7%) patient with suppuration of hydatidous echinococcosis of the liver, complicated by a breakthrough into the pleural cavity and further into the bronchial tree with the development of purulent endobronchitis, only 2 clinical and laboratory signs of systemic inflammatory reaction syndrome were diagnosed. At the same time, in 5 (3.3%) patients with perforation of the echinococcal cyst of the liver into the abdominal cavity, four clinical and laboratory signs of systemic inflammatory response syndrome were noted, which served as the main manifestation of the shock state. A comparison within the frequency of clinical and laboratory signs of systemic inflammatory response syndrome revealed that the absence of symptoms was only among patients with banal suppuration of hydatidous echinococcosis of the liver. Among patients with one clinical and laboratory symptom, systemic inflammatory response syndrome in 96.6% of cases (56 patients) were patients with banal suppuration of hydatidous echinococcosis of the liver and only in 3.4% of cases in patients with suppuration of echinococcal cyst of the liver, complicated with its breakthrough into the intrahepatic bile ducts with the development of cholangitis and jaundice.A more dispersive distribution was observed among patients with two clinical and laboratory signs. They were mainly observed (in 53.1% of cases) among patients with suppuration of an echinococcal cyst of the liver, complicated by its breakthrough into the intrahepatic bile ducts with the development of cholangitis and jaundice and in 44.9% of patients with banal suppuration of hydatidous echinococcosis of the liver. In 2% of cases, such a number of systemic inflammatory response syndrome was noted by us among patients with suppuration of an echinococcal cyst of the liver, with a breakthrough into the pleural cavity, into the bronchial tree with the development of purulent endobronchitis. Three clinical and laboratory signs of systemic inflammatory response syndrome were noted in the main (82.6% of cases) in patients with suppuration of an echinococcal cyst of the liver, complicated by its breakthrough into the intrahepatic bile ducts with the development of cholangitis and jaundice, in 17.4% of cases (4 patients) with suppuration of an echinococcal cyst with a breakthrough into the pleural cavity, followed by the development of pleural empyema. According to four clinical and laboratory signs of systemic inflammatory response syndrome, we noted among 62.5% of patients with perforation of the echinococcal cyst of the liver into the abdominal cavity, with the development of peritonitis and in 37.5% of cases among patients with suppuration of the echinococcal cyst of the liver, with its breakthrough into the pleural cavity, with the development of pleural empyema. Thus, as shown by our studies on the comparative analysis of clinical and laboratory manifestations of purulent-septic complications of hydatidous echinococcosis of the liver, we can note the scarcity of their manifestations, which often did not meet the criteria for the diagnosis of sepsis. This, in turn, indicates the low diagnostic significance of clinical and laboratory signs of systemic inflammatory response syndrome in an objective assessment of the severity of the patient's condition. On the other hand, the reason for such changes may be due to the immunological disorders we have identified, in particular suppressivity, which determine the body's response against the background of bacterial infection. This hypothesis can be confirmed by conducting a comparative analysis of clinical and laboratory manifestations of systemic inflammatory response syndrome and the degree of immunological suppressiveness in patients with hydatidous echinococcosis of the liver complicated by purulent septic process. I would like to remind you that among patients with a complicated form of hydatidous echinococcosis of the liver, we did not identify normal and compensated values of immunological suppressiveness. In most cases (58.94%), we detected decompensated and to a lesser extent (41.06%) – subcompensated degrees of immunological suppressiveness. Among 62 patients with a subcompensated degree of immunological suppressiveness, patients with two (38.71%) and three (33.87%) clinical and laboratory signs of systemic inflammatory response syndrome were more likely. In 13.11% of patients with a subcompensated degree of immunological suppressiveness, 4 clinical and laboratory signs of systemic inflammatory response syndrome to a complicated form of hydatidous echinococcosis of the liver were identified. Patients with a compensated degree of immunological suppressiveness were least represented among patients with one (8.06%) and without symptoms of systemic inflammatory response syndrome (6.45%) of the complicated form of hydatidous echinococcosis of the liver.The decompensated degree of immunological suppressiveness in more than half of the cases (59.55%) was represented by patients with one sign of systemic inflammatory response syndrome. The remaining percentages were distributed in descending order among patients with two (28.09%) and three (2.25%) clinical and radiological signs of systemic inflammatory response syndrome to purulent-inflammatory complications of hydatidous echinococcosis of the liver. It should be noted that in 9 patients (10.11%) with a decompensated degree of immunological suppressiveness, there were no clinical and radiological signs of a syndrome of systemic inflammatory reaction to purulent-inflammatory complications of hydatidous echinococcosis of the liver. When comparing the frequency of registration of the degree of immunological suppressiveness in patients with various clinical and laboratory signs of the manifestation of the syndrome of systemic inflammatory response to the purulent-inflammatory complication of hydatidous echinococcosis of the liver, we also revealed a certain pattern. A subcompensated degree of immunological suppressiveness was diagnosed in all cases among patients with four clinical and radiological signs of systemic inflammatory reaction syndrome. And in patients with three clinical and radiological signs of systemic inflammatory response syndrome, subcompensated immunological suppressiveness was noted in 91.3% of patients (21 patients), and in 2 patients (8.7%) – decompensated. The decompensated degree of immunological suppression increases among patients with two clinical and radiological signs of systemic inflammatory response syndrome, reaching up to 51.02% (25 patients). The remaining 48.98% of patients with two clinical and laboratory signs of systemic inflammatory reaction syndrome were diagnosed with a subcompensated degree of immunological suppressiveness. In patients with one or no clinical and laboratory signs of systemic inflammatory reaction syndrome, patients with a decompensated degree of immunological suppression were prioritized (91.38% and 69.23%, respectively. A compensated degree of immunological suppression in patients with one clinical and laboratory sign was diagnosed in 8.62% of patients (5 patients) with a complicated form of hydatidous echinococcosis of the liver, and without symptoms of systemic inflammatory response syndrome - in 30.77% (4 patients).Summing up the results of comparative analyses of changes in the degree of immunological suppression and clinical and laboratory signs of various forms of hydatidous echinococcosis of the liver, we would like to note that in this disease, the presence of a certain form of purulent-septic complication and especially its manifestations, in the form of signs of a systemic inflammatory reaction syndrome, cannot be taken as the basis for an objective assessment of the patient's condition. We can draw such a conclusion based on the above data, where patients with a decompensated degree of immunological suppression do not have a pronounced clinical picture of inflammation and generalization of the process, whereas in the third chapter of the dissertation we attempted to identify these changes using laboratory indicators of markers of generalization of infection.This statement, in our opinion, is due to early immune suppression, which led to the development of hydatidous echinococcosis of the liver, since its development, and even more so its manifestation, as shown by our experimental data, requires restraint of the immune response system, which proceeded according to the Th2 cell type. And even with the development of cytokinemia, the clinical picture of the purulent-inflammatory process does not reflect the whole essence of the immunological manifestations of the disease. Only the transition to the Th1 cellular type of the body's response leads to a transition to a competent type of immunological response, which contributed to the death of the parasite and its daughter cysts, followed by the development of calcification of the destruction site. It is the translation of the body's immunological response to the Th1 cellular type of response that should be the priority for correcting the disorders that occur. Accordingly, the use of preventive measures to correct immunological suppressiveness will contribute to improving the results of treatment of patients with hydatidous form of liver echinococcosis. Through experimental studies, we have proved that immunoglobulins, in particular G, play a key role in the body's immunological response, which, when exposed to echinococcosis membrane antigens, trigger the body's response according to a certain type of cellular-humoral mechanism. At the same time, in the presence of purulent-septic complications, in conditions where the focus of destruction persists, all measures aimed at detoxification and correction of identified immune disorders can be considered nullified due to their low effectiveness. In this regard, in the main group of patients, the algorithm of tactics of therapeutic and diagnostic measures was based on the first stage in the differentiation of patients divided into subgroups with a complicated course of hydatidous echinococcosis of the liver and without complications. In cases where the patient has a complicated form of hydatidous echinococcosis of the liver, measures were taken aimed at differentiating its type and nature of damage to organs and body systems with full verification of the final diagnosis. The main focus was on reducing the duration of the preoperative period and performing surgical intervention as soon as possible after the patient's preparation. Immediately in the postoperative period, the degree of immunological suppression was assessed, which determined our further tactics of therapeutic measures. With a compensated degree of immunological suppressiveness, no special correction of the immune system was required. Conventional therapy was carried out, including antibacterial, detoxification and restorative treatment. Along with this, targeted antiparasitic chemotherapy was started.In case of subcompensated immunological suppressiveness in the early postoperative period, measures were also carried out, including antibacterial, detoxification and restorative therapy. However, along with this, correction of immunological suppressiveness was required by conducting targeted immunomodulation (thymomimetics, antibody formation and phagocytosis stimulants). When a compensated degree of immunological suppressiveness was achieved, targeted antiparasitic chemotherapy was started. With a decompensated degree of immunological suppression, second-level detoxification therapy was performed in the early postoperative period, which included plasmapheresis, hemosorption, and infusion of detoxifying solutions. Metabolic and antioxidant drugs were also prescribed. In order to correct immunological suppressiveness, in the early postoperative period, substitution immunotherapy (immunoglobulins, interferon alpha, thymomimetics, Roncoleukin) was started. This approach to therapeutic measures was carried out until the level of subcompensated or compensated degree of immunological suppressiveness was reached, against which targeted antiparasitic chemotherapy was started. In patients with an uncomplicated form of hydatidous echinococcosis of the liver, the stage of development of a parasitic cyst was diagnosed at the first stage in comparison with the degree of immunological suppression of the body. All measures, including immunomodulation and substitution immunotherapy, were carried out according to the same scheme as in the case of a complicated form of hydatidous echinococcosis of the liver. However, unlike the complicated variant of the course of the disease, with uncomplicated surgical intervention was performed only when the level of compensated immunological suppressiveness was reached, which is achieved by carrying out the above-described therapeutic and diagnostic algorithm. After targeted antiparasitic chemotherapy, repeated diagnosis of the degree of immunological suppressiveness was carried out for 30 days.
4. Conclusions
- 1. In patients with a complicated form of hydatidous echinococcosis of the liver, the main emphasis is on reducing the duration of the preoperative period. In the postoperative period, the degree of immunological suppression is assessed, which determines the further tactics of therapeutic measures. In patients with an uncomplicated form of hydatidous echinococcosis of the liver, at the first stage, it is necessary to diagnose the phase of development of a parasitic cyst in comparison with the degree of immunological suppression of the body. However, unlike the complicated variant of the course of the disease, with an uncomplicated one, surgical intervention is performed only when the level of compensated immunological suppressiveness is reached.2. The application of the developed clinical and immunological methods for predicting and preventing purulent-septic complications of liver echinococcosis has reduced their incidence from 28.2% to 10.1%. Compared with the control group of patients, an increase in the number of patients with good and satisfactory treatment results was achieved by 7.2% overall, and the number of patients with unsatisfactory treatment results and mortality was reduced by 1.8 and 3 times, respectively.3. The application of the methods developed by us for predicting and preventing purulent-septic complications of hydatidous echinococcosis of the liver, based on the identification of the degree of immunological suppression and the use of targeted methods for its correction, significantly improved the results of treatment in the long-term period by 2.1 times and improved the quality of life of patients with good results by the end of the study to 99.7%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML