-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 428-431
doi:10.5923/j.ajmms.20241402.55
Received: Feb. 2, 2024; Accepted: Feb. 20, 2024; Published: Feb. 22, 2024

An Interdisciplinary Approach to the Correction of Neurological Disorders in Children with Defects and Deformities of the Lower Jaw
Yakubova Z. A., Yakubov R. K., Madjidova Y. N.
Tashkent Pediatric Medical Institute, Tashkent State Dental Institute, Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents the results of a comprehensive examination of 76 children with jaw deformities, after injuries and inflammatory and destructive processes in the temporomandibular joint. Diseases of internal organs were identified: gastrointestinal tract, as well as the central and autonomic nervous system (ANS), more often hypersympathicotonic variant. The authors consider the identified changes as the causes of functional disorders of internal organs, hemostasis and microcirculation, justifying the need to include diseases of internal organs and systems in the complex treatment, as well as correction of the functional state of the ANS.
Keywords: Autonomic nervous system, Osteomyelitis, Somatoform disorders of the ANS, Osteoarthritis, Minimal brain dysfunction, Temporo-mandibular joint
Cite this paper: Yakubova Z. A., Yakubov R. K., Madjidova Y. N., An Interdisciplinary Approach to the Correction of Neurological Disorders in Children with Defects and Deformities of the Lower Jaw, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 428-431. doi: 10.5923/j.ajmms.20241402.55.
Article Outline
1. Introduction
- The central task of modern medicine is to determine the role and place of altered reactivity in pathogenesisо- and sanogenesis. The reactivity of the nervous system (neuroreactivity) acts as part of the overall reactivity of the body. It is characterized by variability and individual characteristics, including hereditary ones, and depends on a complex of continuously occurring and continuously changing reflex and metabolic processes, phyloо-and ontogenetic features of the body, often altered by sensitization, intoxication, and diseases [1]. Identification of small developmental anomalies (Badalyan L. O., 1984, Khodos Kh.S., 1985), which objectify disneiroontogenesis, is of great importance in diagnostics [2]. The term "reactivity" is closely related to the concept of "adaptation", the essence of which is most fully reflected in the definition of V. P. Kaznacheyev (1973): "Adaptation (adaptation) is the process of maintaining the functional state of the homeostatic systems of the body as a whole, ensuring its preservation, development, efficiency, maximum life expectancy in inadequate environmental conditions [1]. To explain the mechanisms of- pathogenesis and sanogenesis, N. P. Bekhtereva etal. (1978) studied the presence of not only rigid, but also flexible links in the brain system. According to the theory of a stable pathological process, quantitative changes first occur in systems that provide a stable pathological state. One stable state passes into another through the destabilization phase. The formation of a primary stable pathological condition is also associated with a violation of homeostasis, its destabilization [3]. In maintaining brain homeostasis at the proper level, an important role belongs to the reactivity and adaptability of the vascular system of the brain (Schmidt E. V., 1975; Mchedlishvili G. I., 1977; Kavtaradze V. G., 197; Vereshchagin N. V., 1980; Gusev E. I., 1983, 1991; Moskalenko Yu. E., Khilko V. A., 1984, 1991) [4]. Changes in the reactivity of the nervous system under the influence of exogenous and endogenous risk factors lead to a decrease in the adaptive capabilities of the nervous system and the occurrence of neurological disorders. Elucidation of the patterns of adaptivity and disadaptivity is an important link in the pathophysiological mechanisms of nervous pathology. The modern scientific theory of human adaptation allows us to move from the knowledge of adaptive processes to their management (Kaznacheyev V. P., 1987, 1991) [5]. Risk factors often act as a dynamic process, where during the development of the disease, risk factors change and pathogenetic processes change. The close а relationship of the vegetative and соcardiovascular systems with the pathogenesis of connective tissue dysplasia makes it important to study the in children with а jaw deformities caused а by TMJ, а pathology and associated with connective tissue dysplasia (DMST). In the literature sources, we did not find information about the state of the autonomic nervous system, their connection with the pathology of internal organs and systems in children with а jaw deformities caused by TMJ pathology.Objective: To study the state of the autonomic nervous system and hemodynamics of brachiocephalic vessels in children with jaw deformities caused by TMJ pathology. Research objectives: 1. Analyze the general condition of children with jaw deformities, caused by TMJ pathology. 2. Using the method of cardiointervalography to assess the functional state of the vegetative nervous system in patients during preoperative preparation.3. Study the functional state of brain hemodynamics based on the results of dopplerography of brachiocephalic vessels.
2. Materials and Methods
- In total, 87 children were examined in the clinics of pediatric surgical dentistry of the Tashkent State Dental Institute, the Department of Neurology, Pediatric Neurology and Medical Genetics of the Tashkent Pediatric Medical Institute, together with the staff of the Tashkent City Children's Medical Consultation and Diagnostic Center. Including 76 (87.4%) children with jaw deformities caused by TMJ pathology (post – traumatic secondary deforming osteoarthritis, 46(60.5%) children, 30(39.4%) - after a destructive form of chronic osteomyelitis of the lower region) - were included in the main group. The majority of patients-41(54%) - were girls. By age, the patients were divided into 3 age groups: group I aged 3-6 years – 10 patients, group II 7-11 years - 26, group III 12-15 years – 36. All of them needed а to be treated operatively in order to eliminate deformation and limit opening of mouth. The control group consisted of 11 tactically healthy children without TMJ pathology.The complex examination of а patients consisted of а basic methods of clinical-laboratorial examination, sting analysis, anamnesis, traditional clinical-laboratory and functional methods (blood, urine, feces, ultrasound of the liver, gallbladder, electrocardiography) and other studies with the participation of a pediatrician, gastroenterologist, neuropathologist, endocrinologist, nephrologist, genetic and other specialists in medical services. The following methods were included in the complex exam: - Dopplerography of brachiocephalic vessels, electroencephalography (EEG), rheoencephalography (REG) cardiointervalography (CIG), with a clino-ortostatic test according to the method of R. M. Baevsky.
3. Research Results and Discussion
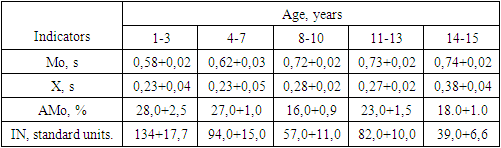
- In the course of a comprehensive interdisciplinary examinationу, 76 (100%) patients had complaints of rapid fatigue, 73(96.05%) – headaches, 42(55.3%) - difficulty in nasal breathing, shortness of breath, sweating-48(63.1%), memory loss-51(67.1%) marbling of the skin 71(93.4%), restless sleep-72 (94.7%), lower back pain-63(82.9%), abdominal pain-50(65.8%), feeling of pain or heaviness in the right hypochondrium -44(57.9%), constipation alternating with diarrhea -46(60.5%), nausea-20(26.3%).The results of the conducted studies showed that out of the 76 children examined, 27(35.5,%) had cholecystitis, 61(80.2%) had biliary dyskinesia, 30(39.4%) had biliary tract abnormalities, 49(64.4%) had functional bowel disorders, and 41 (54%) – chronic colitis, dysbacteritis - in 59(77.6%), in 12(15.7%) - chronic enteritis, in 4(5.2%) -chronic hepatitis, and in 23 (30.2%) patients – chronic gastritis. The pathogenetic factor of these disorders was dysmetabolic syndrome, which in turn was complicated by dysmetabolic nephropathy with oxaluria and crystalluria, signs of mineral metabolism disorders occurred in 76 patients (100%). Studies of the nervous system against the background of chronic intoxication and hypoxia (94,7 revealed signs of somatoform disorders of the autonomic nervous system in 72 (94.7%) patients, asthenic-neurotic syndrome in 54(7.5%), minimal brain dysfunctions in 76 (100%) [8].The results of KIG with the calculation of the stress index in 51 children (46 of them with post-traumatic secondary deforming osteoarthritis, 30 after the destructive form of chronic osteomilitis of the lower region) allowed us to assess the aggressive reactivity (Diagram 2) and adaptive capabilities of the child's body. Normal reactivity and adaptive capabilities were observed only in 7 patients. According to the results of the examination, the prevalence of hypersympathicotonic reactions was found more often at the age of 11-15 years. When examining such patients, asthenic body type, moderate pallor of the skin, moist fingertips were observed, children did not tolerate heat well, almost always felt cold in the hands and feet. Feelings of fear, irritability, and emotional lability were also noted, which is consistent with the literature data [1,7].
|
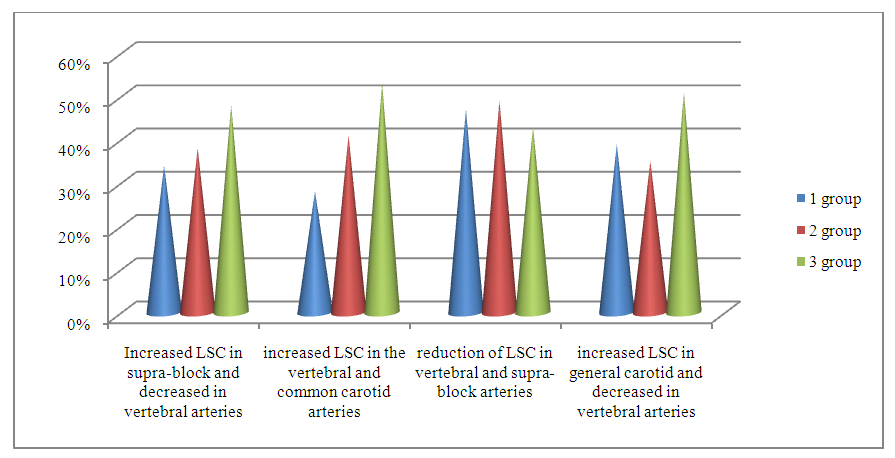 | Chart 1. Results of brachiocephalic vessel Doppler imaging (n=51) |
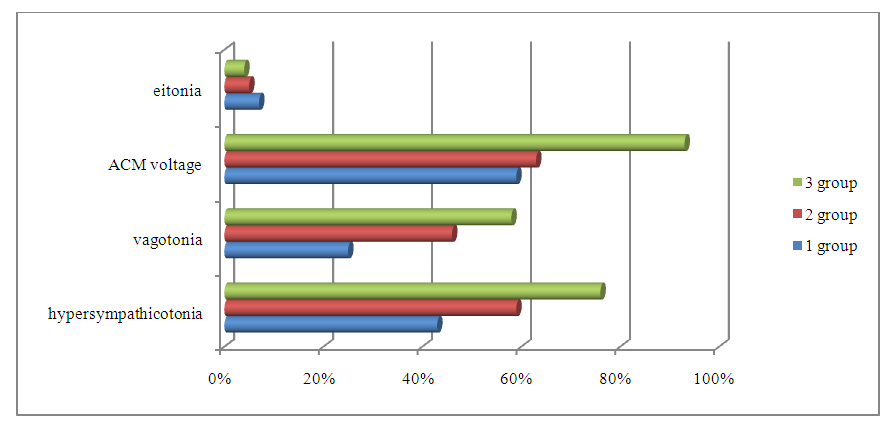 | Chart 2. Assessment of vegetative reactivity by the IN2/IN1 index in COP (n=51) |
4. Conclusions
- 1. An interdisciplinary approach to the study of the health status of children with jaw deformities allowed us to identifythe same type of pathological processes in the internal organs with a predominant lesion of the gastrointestinal tract, nervous system, kidneys, respiratory organs, etc. 2. Cardiointervalography with a clino-ortostatic test makes it possible to determine latent autonomic dysfunction in patients, which plays an important role in the regulation of adaptive-compensatory processes, and to explain local and general disorders in patients with jaw deformitiescaused by TMJ pathologyassociated with connective tissue dysplasia.3. Children with jaw deformities caused by TMJ pathology in complex rehabilitation require an interdisciplinary approach to correction of diseases of internal organs and systems, as well as correction of the functional state of the ANS and CNS in the pre - and postoperative period.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML