-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 423-427
doi:10.5923/j.ajmms.20241402.54
Received: Jan. 29, 2024; Accepted: Feb. 20, 2024; Published: Feb. 22, 2024

Changes in Cerebral Hemodynamic Parameters During Respiratory Support in Patients with Combined Severe Traumatic Brain Injury
A. L. Rosstalnaya1, H. H. Dadaev2, A. U. Takhirov2, D. R. Makhsudov2
1Center for the Development of Professional Qualification of Medical Workers
2Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

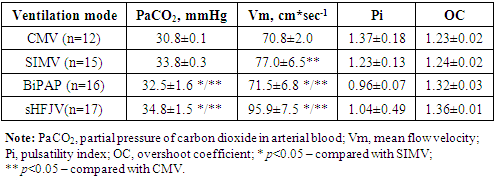
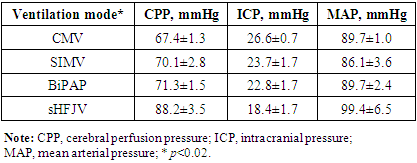
The aim of this research was to study and analyze the effects of mechanical ventilation and some modes of supportive ventilation on central hemodynamics and intracranial pressure, and to make comparative analysis with high-frequency jet ventilation in patients with combined severe traumatic brain injury. Introduction. Today traumatic brain injury has tendency to rapid increase, particularly in the last decade, which is due to industry development. The improvement of efficacy of treatment of the patients with combined severe traumatic brain injury is one of the important areas in modern neurological intensive care. Material and methods. The research was carried out in neurological intensive care unit of Republican Research Center of Emergency Medicine in 60 patients with combined STBI. Mean age of the patients was 32±5. In admission, the condition of the patients was assessed as severe, and level of consciousness was 7±3 according to Glasgow Coma Scale. Results. The effect of sHFJV on cerebral hemodynamics was compared with other modes of mechanical ventilation. This comparison showed that in this mode ventilation cerebral perfusion pressure (CPP) was quite higher (88.2±3,5 mmHg) than that in modes such as CMV, SIMV, BiPAP (67.4±1.3, 70.1±2.8, 71.3±1.5, respectively). In addition intracranial pressure (ICP) was much lower in sHFJV (18,4±1,7 mmHg) as compared with other modes (CMV, SIMV, BiPAP; 26.6±0.7, 23.7±1.7, 22.8±1.7, respectively). Conclusion. In comparative analysis of supportive modes of mechanical ventilation, they significantly influence on intracranial pressure and functions of cardiovascular system, but do not have negative effect on cerebral perfusion pressure. All these prove the advantage and advisability of the use of supportive ventilation modes combination with high-frequency ventilation in the complex of respiratory support and intensive care of patients with combined severe traumatic brain injury.
Keywords: Traumatic brain injury, Supportive modes of mechanical ventilation, Cerebral hemodynamics, Respiratory support
Cite this paper: A. L. Rosstalnaya, H. H. Dadaev, A. U. Takhirov, D. R. Makhsudov, Changes in Cerebral Hemodynamic Parameters During Respiratory Support in Patients with Combined Severe Traumatic Brain Injury, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 423-427. doi: 10.5923/j.ajmms.20241402.54.
Article Outline
1. Introduction
- Today traumatic brain injury has tendency to rapid increase, particularly in the last decade, which is due to industry development. The improvement of efficacy of treatment of the patients with combined severe traumatic brain injury (STBI) is one of the important areas in modern neurological intensive care. Currently, the problem of treating combined severe traumatic brain injury (TBI) is a topical issue in modern medicine and is of great socio-economic importance. The main contingent of victims is persons of working age (from 20 to 50 years). In the structure of mortality, 30-50% of all types of injuries are due to TBI. The overall mortality rate for TBI, including mild and moderate TBI, is 5-10%. In severe forms of TBI with the presence of intracranial hematomas and foci of brain contusion, mortality increases to 41-85%. In 20-25% of cases, TBI is combined with damage to other organs and systems: the musculoskeletal system, organs of the thoracic and abdominal cavities, the spine and spinal cord. Mortality among victims with combined TBI with extremely severe injuries and massive blood loss can reach 90-100% (V.V. Lebedev, V.V. Krylov (2000); V.A. Sokolov (2001); M.R. Bullock (2000). According to the data of the Institute of Health of the Ministry of Health of the Republic of Uzbekistan, the number of mechanical injuries per 100 thousand population is more than 3000, in some regions of the country this figure is even higher. As for the occurrence of severe traumatic brain injury, this figure exceeds 592 cases per year per 100,000 population [2], with combined traumatic brain injuries accounting for 40-45% of all traumatic brain injuries.Worldwide, traumatic brain injury is still one of the leading causes of disability in the population. The number of injured persons with permanent disability as a result of traumatic brain injury reaches 25-30%. In this regard, traumatic brain injury ranks first in terms of total medical, social and economic damage among all types of injuries.The basis of intensive care in neurosurgery is the prevention and treatment of secondary cerebral ischemic attacks [7, 8,9]. To prevent, external respiratory support that is adequate of the demand of the brain has significant role. Inadequate minute ventilation often causes hypoxia while hyperventilation may also be harmful due to hypocarbia and cerebral vasospasm [1]. Modern mechanical ventilators allow performing effective supportive ventilation while keeping spontaneous rhythm of patient. But we should not forget that in trauma and diseases of central nervous system, principles of respiratory support developed for general intensive care in various primary injuries of the lungs, cannot be totally used in neurological intensive care [12,15].In the world of science there are many researches on problems of mechanical ventilation in lung injuries, and researches on respiratory support in patients of neurological intensive care are rather limited [10,13]. Scientific works on cerebrovascular effects of mechanical ventilation are rare and they do not describe the problem from all quarters. We should emphasize that application of mandatory modes in this contingent of patients with intact cough reflex leads to asynchrony of the patient with mechanical ventilator. Increase in intrathoracic pressure results in reduction in venous return to the heart and rise in pressure in venous system including in cranium which in turn causes the increased intracranial pressure [11,14,18]. So, today the question about the relation between ventilation and cerebral blood flow becomes topical.Studying conventional modes of mechanical ventilation in last decades showed unfavorable effects on some vital functional of organism, particularly on central hemodynamics, pulmonary and peripheral circulation [2,3]. In the light of these factors and for solution of some other problems of effective treatment of combined STBI, high-frequency ventilators are developed and being used. Special features of these ventilators are much lower transpulmonary pressure and pressure in airways. In addition, negative pressure in pleural cavity is kept during inspiration and spontaneous breathings. Depression of hemodynamics and activation of antidiuretic hormone, i.e. decrease in stress reactions is not observed. And there is no need in the use of respiratory depressants for adaption of the patient to the ventilator, and in the airtightness of breathing circle to keep adequate gas exchange [1,6,16,17,18].The aim of this research was to study and analyze the effects of mechanical ventilation and some modes of supportive ventilation on central hemodynamics and intracranial pressure, and to make comparative analysis with high-frequency jet ventilation in patients with combined severe traumatic brain injury (STBI).
2. Materials and Methods
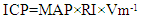
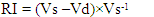
- Institutional Ethics Committee approved our research and the use of oral consent in our research, as most of the admitted patients were in severe condition and their relatives wanted to begin treatment instantly, so only oral consent was taken from relatives of the patients and this consent was documented in medical history of the patients. The research was carried out in neurological intensive care unit of Republican Research Center of Emergency Medicine in 60 patients with combined STBI. Mean age of the patients was 32±5. In admission, the condition of the patients was assessed as severe, and level of consciousness was 7±3 according to Glasgow Coma Scale. Intracranial pressure in admission was more than 15 mmHg. All patients had chest frame disruption in the form of 4±2 rib fracture without displacement and pleuropulmonary complications. All patients were operated for removal of subdural and/or intracerebral hematoma or hygroma. Conventional intensive care with mechanical ventilation was performed to all patients. Mortality coefficient was 32.7% (18 patients).Indication for mechanical ventilation was not only development of respiratory failure, but also progression on neurological disorders. Clinical-neurological examination and control of laboratory findings (common blood count, arterial blood gases, arteriovenous oxygen gradient (avDO2) and hemoglobin saturation in jugular vein (SjO2)) were performed. We examine gases of capillary, arterial and venous blood for our research. Blood sample of jugular vein was taken from internal jugular vein in 1st, 3rd and 5th days. Parameters of blood gases were studied not less than 4 times in a day during the whole period of mechanical ventilation. Blood gases analysis was carried out by blood gas analyzer “Analyze Blood Gas” (USA). Arteriovenous oxygen gradient was calculated using the data of pulse oximeter and hemoglobin saturation in jugular vein blood, and comparing with results of arterial blood gases analysis. In postoperative period mechanical ventilation in all patients was done with ventilators Savina, Evita 2+ (Draeger®, Germany), Hamilton-C6 (Hamilton Medical AG, Switzerland) while standard intensive care was continued. High-frequency ventilation was done with ventilator MB 200 “ZISLINE” (Yekaterinburg, Russia). Initially we applied СMV (Conventional Mechanical Ventilation) mode, which was then individually changed into BiPAP (Biphasic Positive Airway Pressure), SIMV (Synchronized Intermittent Mandatory Ventilation), sHFJV (High-frequency Jet Ventilation).Parameters of the modes were: 1. СMV – 12 patients with the following parameters: TV – 7-8 ml*kg-1, Ti – 33%, PEEP – 5-7 cmH2O, FiO2 – 0.3-0.4;2. SIMV – 15 patients with the following parameters: TV – 5-6 ml*kg-1, f – 20-22 per minute, Ti – 33%, PS – 15 cmH2O, FiO2 – 0.3-0.4;3. BiPAP – 16 patients with the following parameters: TV – 5-6 ml*kg-1, f – 20-22 per minute, Ti – 33%, PS – 15 cmH2O, FiO2 – 0.3-0.4;4. sHFJV – 17 patients with the following parameters: TV – 17-18 l*min, f – 100-120 per minute, Ti – 33%, FiO2 – 0.21-0.3.Adequacy of mechanical ventilation was assessed by SpO2 – 96-99% and PaCO2 – 34.7-35.2 mmHg.Simultaneously cerebral hemodynamics in all patients was examined by the method of transcranial Doppler ultrasound using the portable device “Mindray” (MT-1010, China) with monitoring program. Two transducers with the frequency of 2 MHz were used for diagnostic examination and monitoring. The following parameters were registered: mean flow velocity (Vm, cm*sec-1), pulsatility index (Pi) that shows hydrodynamic resistance of pial-capillary vessels of brain and overshoot coefficient (OC) that characterize the ability of pial-capillary system to regulate blood flow of brain [3,4,5].In patients with disturbed vascular autoregulation due to cerebrovascular disease, but without the signs of vasoconstriction and hemodynamically significant stenosis, the value of intracranial pressure (ICP) was calculated as follows [10,11]:
 | (1) |
 | (2) |
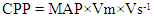 | (3) |
|
3. Statistics
- The software we used for statistical analysis was STATISTICA 10, StatSoft, Inc. 2011. p value was calculated by Pearson’s chi-squared test.
4. Results and Discussion
- Arterial blood gases were examined by the Astrup method in blood gas analyzer ABL. All patients had hematocrit within normal ranges (0.40-0.44).To reveal the features of cerebral circulation we compared the parameters characterizing cerebral circulation during high-frequency ventilation versus conventional mechanical ventilation (Table 1). Analysis of materials indicates that all modes of ventilation were performed with modern (near to normal) hyperventilation. The value of PaCO2 significantly differed of the normal ranges and did not differ between the modes. Therefore, there are grounds to confirm that changes in the parameters of cerebral circulation basically depend on the mode of ventilation. The most substantial shifts in the parameters of cerebral circulation were seen during conventional mechanical ventilation. These patients had significant increase in peripheral resistance and decrease in dilation reserve in comparison with the patients on spontaneous breathing. Presence of spontaneous breathing during supportive ventilation reduced negative effects of volume-controlled mechanical ventilation. Patients in whom this mode of ventilation was used had tendency to low peripheral resistance (overshoot coefficient).In high-frequency ventilation we observed distinctive dynamics of the parameters of cerebral circulation. General picture of cerebral circulation in sHFJV was similar to that in BiPAP and SIMV. Parameters that characterize autoregulation of cerebral circulation (Pi and OC) in BiPAP, SIMV and sHFJV did not substantially differ. The difference was only in the value of peripheral resistance in sHFJV, which was near to normal while in BiPAP and SIMV it was increased. In CMV mode, such conditions develop that cerebral circulation becomes unprotected from various changes in systemic hemodynamics due to absence of autoregulation and its little effect on systemic hemodynamics. As we know there is relation between central perfusion pressure and Pi, and this indicates that in the absence of autonomy, cerebral circulation completely receives vascular reactions of systemic hemodynamics, which is especially dangerous in systemic hypertension. Therefore, this mode of mechanical ventilation is rarely applied in patients with cerebral insufficiency. There may be exceptions when we are obliged to apply this mode. These conditions are those in which spontaneous breathing is disturbed (apnea, convulsive syndrome, etc.).The main distinction of cerebral hemodynamics in high-frequency ventilation from other modes of ventilation was in considerable increase in mean flow velocity (Vm). Increase in this parameter was basically associated with high cerebral perfusion pressure.Parameters of cerebral hemodynamics in Table 2 indicate that in all modes of ventilation besides sHFJV cerebral hypoperfusion developed (normal ranges of CPP – 80-100 mmHg). Incidentally, CPP was in normal ranges, which may be associated with the absence of depression of systemic hemodynamics and much lower ICP in high-frequency ventilation. It is worth to emphasize that characteristics of cerebral perfusion in HFJV did not depend on the severity of consciousness disturbance since the condition of the patients in sHFJV was significantly worse than those on spontaneous breathing or supportive ventilation, and did not differ from those who were on volume-controlled ventilation (according to Glasgow Coma Scale). The fact that attracts attention is that ICP is much lower in high-frequency ventilation. This phenomenon is quite important; because it allows us to be convinced, that high-frequency ventilation is one of the factors preventing the progression of cerebral hypertension in comatose conditions.
|
5. Conclusions
- Application of sHFJV as respiratory support in combined STBI makes favorable conditions for central hemodynamics and cerebral perfusion is considered as optimal mode of respiratory support in complex care of comatose conditions. Absence of cerebral perfusion depression and integrity of autoregulation of cerebral circulation attest that during this mode of ventilation all processes of cerebral perfusion are adequately supplied. Hence, high-frequency ventilation is more physiological and safer for patients with combined STBI.
ACKNOWLEDGEMENTS
- We are grateful to Dr. Mahkamov K.E. for his counsel to and support of the Neurosurgical ICU and his insightful comments on the manuscript. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML