-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 416-422
doi:10.5923/j.ajmms.20241402.53
Received: Jan. 25, 2024; Accepted: Feb. 17, 2024; Published: Feb. 22, 2024

Laparoscopic Pyelolithotomy: The Optimal Drainage Method
M. M. Bakhadyrkhanov1, G. T. Mukhtarov1, F. A. Akilov2, B. A. Ayubov1, D. A. Nazarov1, F. R. Nosirov1, Kh. Z. Nuriddinov1, Khojanyazov Sh. R.1
1Republican Specialized Scientific and Practical Medical Center of Urology
2Tashkent Medical Academy, Department of Urology, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to improve the treatment results of patients by improving the urinary tract drainage methods during laparoscopic surgery. Introduction. Percutaneous renal drainage is effective for most, if not all, obstructions, including intrarenal, ureteropelvic or ureteral obstructions. An alternative to percutaneous drainage is drainage through a ureteral catheter or a retrograde stent. The choice of antegrade or retrograde drainage of the upper urinary tract collecting system depends on the indication, health status and anatomy of the patient, as well as the preferences of both the patient and the physician. Using percutaneous renal access, surgical removal of upper urinary tract stones, urothelial tumors, obstructions, and calyceal diverticula can be performed. Material and methods. 45 patients who underwent laparoscopic pyelolithotomy at the Republican Specialized Scientific and Practical Medical Center of Urology in the period from 2012 to 2022 were selected for the study. The mean age of the patients was 34.2 ± 13.3 years (M±δ). There were 30 (66.7%) males and 15 (33.3%) females among them. In 26 (57.8%) patients, the surgery was performed on the left side, and in the remaining 19 (42.2%) ones - on the right. Results. To assess the efficiency and safety of upper urinary tract drainage, the duration of surgical intervention; the amount of intraoperative blood loss; the frequency of intra- and postoperative complications; the frequency of additional interventions; the severity of pain syndrome; the duration of the patient's stay in the hospital; the length of the incision; assessment of the patient's quality of life using an adapted Wisconsin questionnaire (WISQOL) were comparatively analyzed. During the study, the duration of surgical intervention was analyzed to assess the impact of nephrostomy drainage period during laparoscopic pyelolithotomy, as well as the time to relieve intraoperative complications associated with the drainage method. Conclusion. The developed technique for installing nephrostomy drainage during laparoscopic pyelolithotomy allows to install drainage on upper urinary tracts during the surgery itself, without involving additional specialists and equipment. This technique is not only safe for use in patients, but also reduces the duration of surgery and the frequency of postoperative complications, allows patients to get rid of drains at an earlier date and contributes to a rapid improvement of the life quality.
Keywords: Laparoscopic pyelolithotomy, Therapeutic percutaneous nephrostomy, Drainage, Urinary tract, Ureteral catheter
Cite this paper: M. M. Bakhadyrkhanov, G. T. Mukhtarov, F. A. Akilov, B. A. Ayubov, D. A. Nazarov, F. R. Nosirov, Kh. Z. Nuriddinov, Khojanyazov Sh. R., Laparoscopic Pyelolithotomy: The Optimal Drainage Method, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 416-422. doi: 10.5923/j.ajmms.20241402.53.
1. Introduction
- Using a new technique of combining upper urinary tract (UUT) drainage and ureteral intubation during laparoscopic pyelolithotomy, it is possible to drain effectively the UUT, maintain autonomy of ureteral intubation and remove all drainage through a single puncture on the patient’s body.Hillier repeatedly aspirated a young boy's hydronephrotic kidney to relieve symptoms for 4 years until his death at age 8 at Great Ormond Street Children's Hospital in London in 1865, [1-2]. It was the first description of percutaneous nephrostomy in the literature. Subsequently, there were several reports of diagnostic percutaneous renal aspiration, but it was not until Goodwin, Casey, and Wool in 1955 described percutaneous trocar nephrostomy for temporary drainage of hydronephrosis in 16 patients that therapeutic percutaneous nephrostomy was rediscovered [3]. Even then, the usefulness of percutaneous access to the upper urinary tract collecting system was limited by the drainage of obstruction [4-11], until Fernström and Johansson (1976) described percutaneous removal of kidney stones, called percutaneous nephrolithotripsy [12]. After it, percutaneous access to the upper urinary tract became the main diagnostic and therapeutic method. Percutaneous renal drainage is effective for most, if not all, obstructions, including intrarenal, ureteropelvic, or ureteral ones. Although lower urinary tract obstruction is best treated with bladder drainage using a urethral catheter, secondary supravesical obstruction can be relieved by placement of a percutaneous nephrostomy tube if other measures did not provide adequate drainage [13-14,10]. An alternative to percutaneous drainage is drainage through a ureteral catheter or a retrograde stent. The choice of antegrade or retrograde drainage of the upper urinary tract collecting system depends on the indication, health status and anatomy of the patient, as well as the preferences of both the patient and the physician [14].As a rule, the retrograde route of drainage is preferable to the antegrade one [15]. However, in upper collecting tract obstruction complicated by infection, drainage is an emergency, and in many such cases percutaneous rather than retrograde drainage is superior [16]. Percutaneous nephrostomy tubes and retrograde ureteral stents are generally equivalent in their ability to relieve fever in patients with upper urinary tract obstruction and acute urinary tract infection [17-18], but in a particular patient, circumstances may dictate a preference for one approach over another. Retrograde ureteral stent placement requires regional or general anesthesia, whereas a percutaneous nephrostomy tube can be placed under a local anesthesia. Because the percutaneous approach has a higher initial success rate than the retrograde approach, in cases where the collecting system is dilated, it may be preferable in patients requiring rapid intervention. Conversely, untreated coagulopathy is a contraindication to percutaneous access, but ureteral stents can be safely placed in patients taking anticoagulants. In rare cases, percutaneous renal access is needed solely for diagnostic purposes, for example, for the Whitacker test, which is an invasive but very accurate test for differentiating obstructive hydronephrosis from non-obstructive one [19]. Percutaneous renal access can be performed to facilitate the instillation of chemotherapeutic agents for urothelial lesions of the upper urinary tract or agents for chemolysis of kidney stones, including the administration of antifungal drugs for renal bezoars.Using percutaneous renal access, it is possible to perform surgical removal of upper urinary tract stones, urothelial tumors, obstructions, and calyceal diverticula [20]. The use of percutaneous drainage of the upper urinary tract after various surgical interventions is widespread. However, based on the situation after surgery, the surgeon must decide which drainage means to use [21].
2. Material and Methods
- 45 patients who underwent laparoscopic pyelolithotomy at the Republican Specialized Scientific and Practical Medical Center of Urology in the period from 2012 to 2022 were selected for the study. The mean age of the patients was 34.2 ± 13.3 years (M±δ). There were 30 (66.7%) males and 15 (33.3%) females among them. In 26 (57.8%) patients, the surgery was performed on the left side, and in the remaining 19 (42.2%) ones - on the right. During the preparation for laparoscopic surgery, all patients were performed general and biochemical blood tests, tests to determine the Rh factor, HIV infection, syphilis, hepatitis B and C and blood group, the prothrombin index, Lee-White blood clotting time and the Duke bleeding time test. Blood serum urea and creatinine levels were used to determine the functional state of the kidney. Reference values for normal urea levels were considered to be 2.8-7.2 mmol/l, and for creatinine in men - 70-115 µmol/l, for women - 44-80 µmol/l.Laparoscopic surgeries were performed using endovideosurgical equipment and instruments from KARL STORZ (Germany), an electrosurgery device ARC 400 (BOWA Medical, Germany) and an ultrasonic scalpel Hormonic Scalpel Gen04 (Ethicon, USA). An Ethicon ultrasonic scalpel was used for each patient. The handle of the ultrasound scalpel was connected to the Hormonic Scalpel Gen04 generator. Urinary tract ultrasound was performed on ultrasound devices "Affinity 50G" (Philips, Netherlands) and "Sonix SP" (Ultrasonix, Canada).A special electronic patient examination card was developed to identify significant clinical, laboratory and instrumental parameters. It contained passport information, objective data, complaints, comorbidities, data of laboratory and instrumental methods of investigation, methods of surgical treatment and their results, as well as other significant features. The whole card was realized as an electronic database on a personal computer (Excel 2019 Mac). The quantitative features were coded binary (Yes, No), and gradations were introduced for qualitative signs. The necessary data arrays for the study were formed by filtering the initial information matrix according to the given conditions. Methods of graphical analysis (box histograms, quantile plots) and mathematical methods (Shapiro-Wilk criterion, Kolmogorov-Smirnov criteria) were used to test the distribution of the trait for normality. Analysis of variance (ANOVA) was used to compare characteristics of three or more normally distributed groups. the Mann-Whitney U test was used for statistical analysis and comparison of groups with a non-parametric (non-normal) distribution. The Kruskal-Wallis test was used to compare characteristics of three or more groups with a non-parametric (non-normal) distribution. The hypothesis about the distribution law of the studied value was tested using the Pearson goodness-of-fit test or Chi-square. The level of statistically significant results was considered p < 0.05. Statistical data processing was carried out using StatPlus and IBM SPSS Statistics programs. The aim of the study was to improve the treatment results of patients by improving the urinary tract drainage methods during laparoscopic surgery.
3. Results
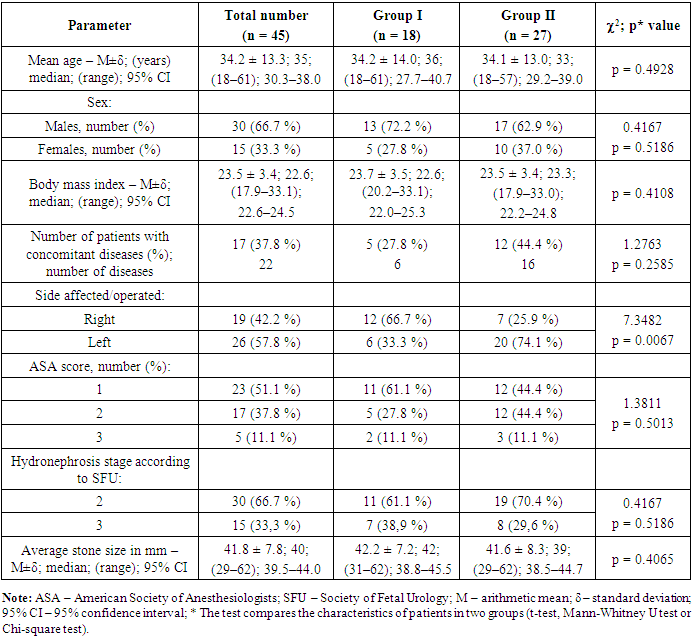
- 19 (42.2%) patients had an active urinary tract infection (UTI) before surgery, 18 (40%) of them had a nephrostomy tube installed before surgery for urine diversion and treatment of UTI. Surgery was performed after the active UTI had resolved. All 45 patients were divided into 2 groups: • Group I consisted of 18 patients who had a nephrostomy tube installed before the main operation;• 27 patients in Group II had a nephrostomy tube installed during laparoscopic pyelolithotomy using the developed technique for installing drainage in the UUT. The initial characteristics of patients in the 2 groups did not differ significantly (Table 1).
|
 | Figure 1. Boxplot of intraoperative blood loss in both groups of patients performed laparoscopic pyelolithotomy (p < 0.001) |
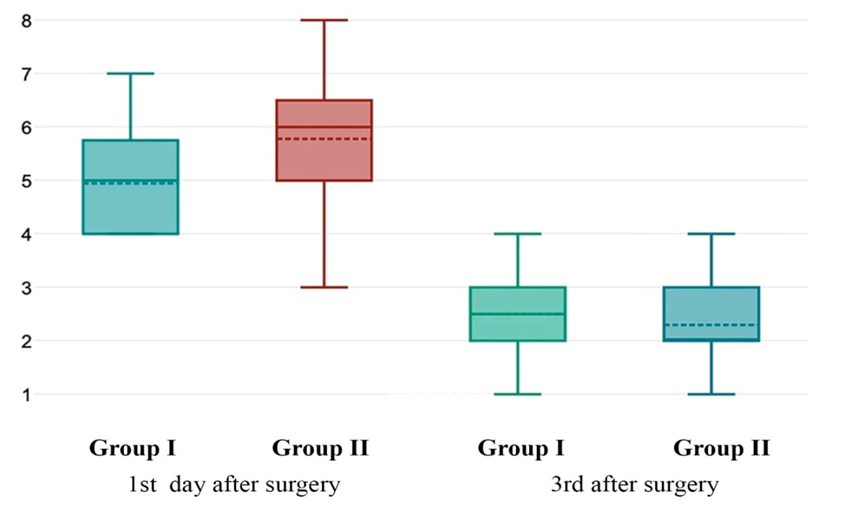 | Figure 2. Boxplot of postoperative pain assessment using a visual analogue scale on days 1 and 3 after surgery comparing the two groups (p < 0.001 and p = 0.22) |
|
4. Discussion
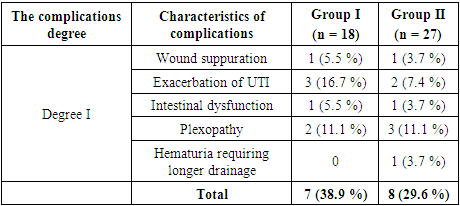
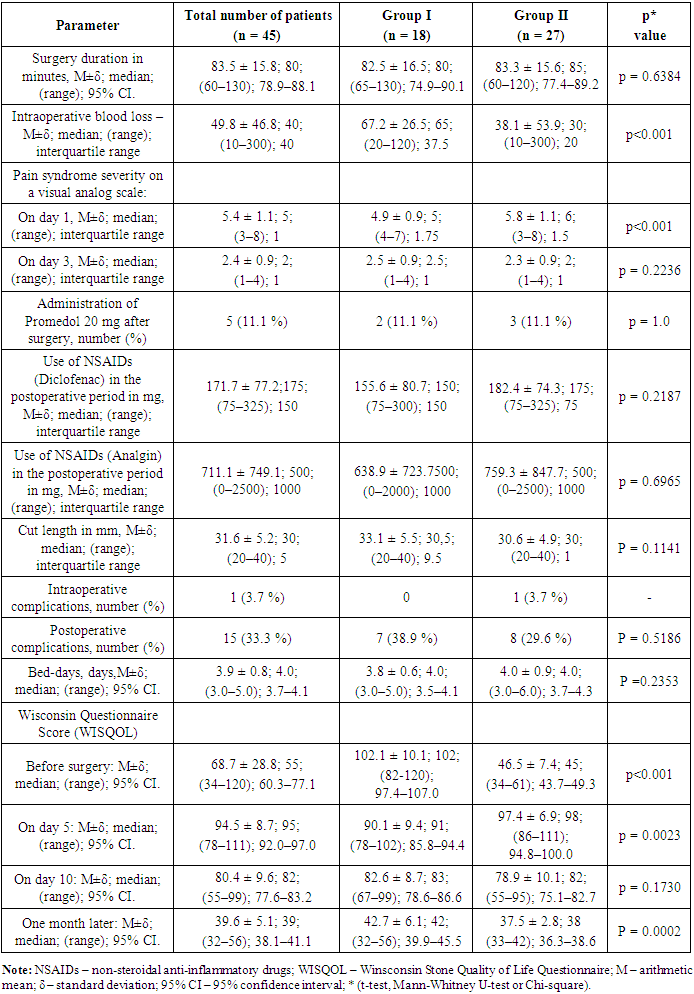
- Summarizing the observational data, we can conclude that the new method of installing nephrostomy drainage does not affect the duration of the surgery, the severity of pain and the amount of painkillers, there was no difference in intra- and postoperative complications and in the length of hospital treatment, etc. All data is shown in Table 3.
|
5. Conclusions
- The developed technique for installing nephrostomy drainage during laparoscopic pyelolithotomy allows you to install drainage on the UUT during the surgery itself, without involving additional specialists and equipment. This technique is not only safe for use in patients, but also reduces the duration of the operation and the incidence of postoperative complications, allows patients to be relieved of drainage at an earlier stage and helps to quickly improve the life quality. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML