Shuxrat Shukurullaevich Isakov
Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Correspondence to: Shuxrat Shukurullaevich Isakov, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The results of treatment of purulent tracheobronchitis in patients operated on for emergency surgical diseases of the abdominal organs, complicated by peritonitis, using bronchoscopic photodynamic therapy, nebulized delivery of methylene blue (MB) at a concentration of 0.05%, followed by laser irradiation of this solution with a wavelength of 0 are presented .63 µm. A significant reduction or complete relief of clinical manifestations of purulent tracheobronchitis was noted.
Keywords:
Purulent tracheobronchitis, Endoscopic photodynamic therapy, Emergency abdominal surgery
Cite this paper: Shuxrat Shukurullaevich Isakov, Rationale for the Effectiveness of Bronchoscopic Photodynamic Sanation Using Methylene Blue for Purulent Tracheobronchitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 390-397. doi: 10.5923/j.ajmms.20241402.49.
1. Introduction
In recent years, the frequency of bronchopulmonary complications in patients undergoing surgery on the abdominal organs is, according to various authors, from 15 to 17.2% [1,2]. The frequency of bronchopulmonary complications that developed after laparotomies, including diffuse purulent tracheobronchitis, varies quite widely and ranges from 1.9% to 9.6% [4]. At the same time, mortality from bronchopulmonary complications in patients undergoing surgery on the abdominal organs remains quite high [5,6].Traditionally, for postoperative bronchopulmonary complications, bronchoscopic sanitation is performed using antibiotics, antiseptic solutions, as well as parenteral antibiotic therapy. However, the causative agents of purulent-inflammatory processes are mainly staphylococci and pneumococci, which in most cases are resistant to many antibacterial drugs [7,8].Antibacterial photodynamic therapy (ABPT) is a method of inactivating microbial cells using a photosensitizer and a source of laser or LED radiation with the appropriate wavelength [9]. It has been established that ABPT does not depend on the spectrum of sensitivity of pathogenic microorganisms to antibiotics; it has a detrimental effect on antibiotic-resistant strains of Staphylococcus aureus, pneumococcus, etc. The development of resistance of microorganisms to antibiotics to the action of PDT is unlikely, because photodynamic damage is caused by the cytotoxic effect of singlet oxygen and free radicals; Photosensitizers used in the clinic are non-toxic and do not have a mutagenic effect; the antimicrobial effect of PDT does not decrease with long-term treatment of chronic local infectious processes; The bactericidal effect of PDT is local in nature; it does not have a systemic detrimental effect on the saprophytic microflora of the body [10]. Dissatisfaction with the results of antibacterial drug therapy forces us to look for other ways of eradication, including physical local methods of influencing the local inflammatory process and the microflora of the bronchial tree. In this regard, the development of intra- and postoperative bronchoscopic sanitation for disorders of bronchial obstruction and lower respiratory tract infections, including tracheobronchitis, in patients with obstructive purulent-inflammatory complications of the tracheobronchial tree, tolerant to drug therapy in emergency abdominal surgery, is relevant.The purpose of the research. The purpose of the study is to improve the results of treatment of purulent tracheobronchitis by using bronchoscopic photodynamic therapy with methylene blue in patients undergoing surgery on the abdominal organs.
2. Research Materials and Methods
The study included 81 patients (there were 43 patients in the main group and 37 in the control group) who were treated in the surgical department of City Clinical Hospital No. 4 named after. I. Ergashev in the period from October 2019. to December 2023. In the main group, bronchoscopic sanitation of the bronchial tree was carried out with low-intensity laser radiation with a wavelength of 0.63-0.66 μm, using a 0.05% solution of methylene blue (MB) as a photosensitizer, and in the control group, sanitation was performed furatsilin solution 1:5000. We previously established the optimal doses and exposure time of laser irradiation, and the required concentrations of MB in in vitro experiments [3].The study groups were equal and comparable in terms of basic typological characteristics: gender, age, severity of clinical and endoscopic signs of purulent tracheobronchitis and the initial composition of the microflora of the bronchial tree, as well as diseases and the extent of the operation performed.The nature of the diseases of the abdominal organs for which emergency surgical interventions were performed is presented in Figure 1. It follows that in all cases the patients were operated on for local and widespread peritonitis caused by destructive appendicitis, perforated gastroduodenal ulcers, strangulated ventral hernias, destructive pancreatitis, etc. In 18 cases, the indication for emergency surgical intervention was acute small intestinal obstruction, in 9 cases - acute destructive pancreatitis.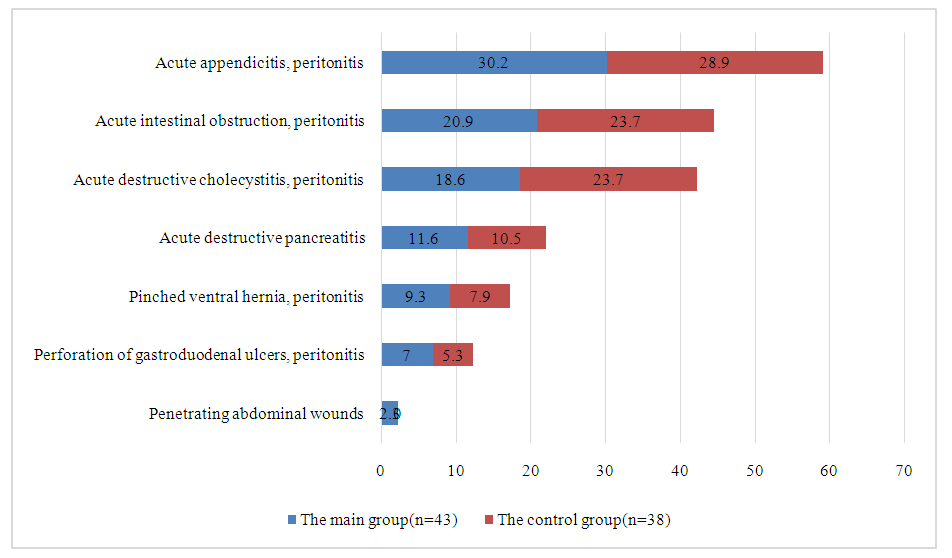 | Figure 1. The nature of acute surgical diseases of the abdominal organs |
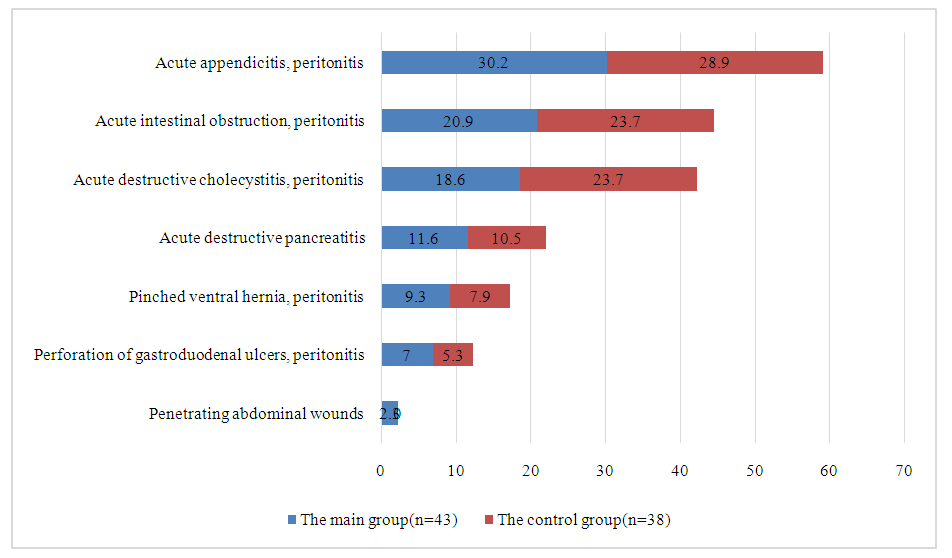
The nature and extent of surgical interventions performed are presented in Figure 2. As can be seen from Figure 2, traditional surgical interventions were used in all observations.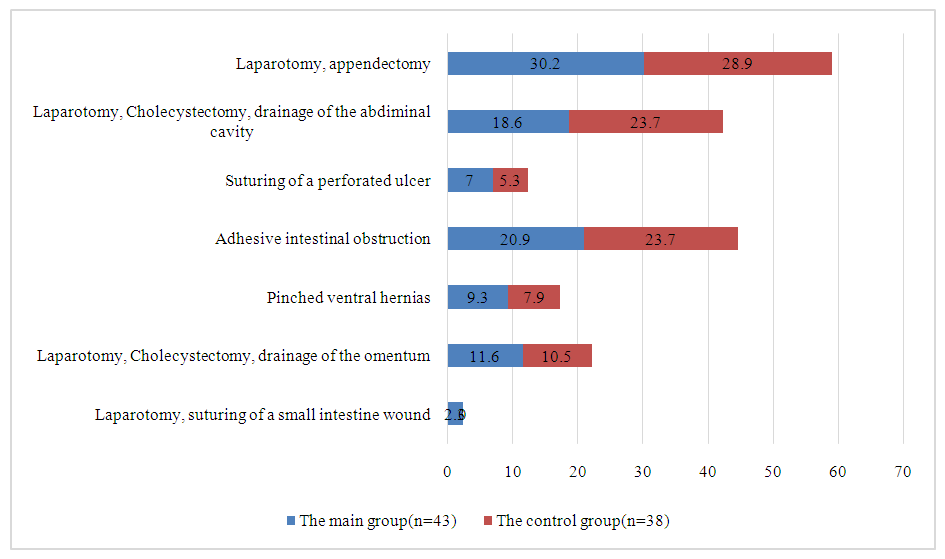 | Figure 2. The nature of surgical interventions performed in patients of the main and control groups |
In patients with acute surgical diseases of the abdominal organs, starting from 2-3 days after surgery, the risk of bronchopulmonary complications increases significantly. At the same time, postoperative bronchopulmonary complications in elderly and senile patients occur in 4 to 54% of cases. In this regard, the feasibility of developing preventive measures is beyond doubt.To assess the intensity of mucosal inflammation, we used the classification of Lemoine J. (1965); according to the author, the apparent intensity of inflammation can be of three degrees.When a diagnosis of bronchitis of II or III degree of inflammation intensity is established, sanitary bronchoscopy should be performed.All patients of the main (43) and control group (38) underwent fibrotracheobronchoscopy of the FTBS during the operation, and the following degree of damage to the tracheobronchial tree was established: in the main group, 8 patients were diagnosed with 1 degree of tracheobronchitis, and in 6 patients, 2 degrees in the main group - in 3, in the control - in 4. The third degree of damage in the main and control groups, respectively: 3 and 3 patients. In 29 (67.4%) patients in the main group and in 26 (68.4%) in the control group, no special changes in the tracheobronchial tree were detected intraoperatively.The photosensitizer MB at a concentration of 0.05% was delivered to the tracheobronchial tree by nebulizer inhalation. The photodynamic therapy procedure was performed 5 minutes after inhalation during bronchoscopy. Through a light guide passed through the biopsy channel of the fibrobronchoscope, irradiation of the orifices of the middle, upper lobe, and main bronchus on one side and then in the same sequence on the other side was sequentially carried out. The output power at the end of the light guide was 0.25 W, wavelength 675 nm, exposure 25-35 J/cm2.Sanitation is carried out by us in the intensive care unit, or on the operating table and in the postoperative period according to indications. After exposure for 1-3 minutes, sputum and pathological contents are collected from the lumen of the bronchial tree. The main goal of the procedure is to remove pathological contents and infected sputum from the lumen of the bronchial tree, while simultaneously influencing the pathological flora and altered mucosa of the bronchial tree in order to relieve inflammatory changes or prevent them. Before sanitation, we remove the contents of the bronchial tree through the instrumental channel of the bronchoscope. At the same time, collecting the contents of the bronchial tree into a sputum catcher - a “trap”, directly connected to the instrumental canal. With this procedure, as a rule, we manage to free all visible parts of the bronchial tree - subsegmental bronchi, i.e., from sputum and pathological contents. bronchi 5 - 6 generations.We used an LG-75 installation (helium-neon laser) with coherent red radiation delivered to the object of study through a fiber-optic light guide. The emission range is 640±20nm, which provides 100 mW of radiation and can be focused into a spot with a diameter of 1.5 to 5 cm depending on the distance to the object.A total of 147 samples of clinical material were examined, of which various types of microorganisms were isolated in 63 (43.0%) samples. Among the isolated strains, the most common were: Esherichia coli – 18.2%, Staphylococcus aureus – 10.7%, Acinetobacter spp. – 6.2%, Klebsiella pneumonia – 6%, Candida spp. – 10.7%, Pseudomonas aeruginosa – 7.4%. Staphylococcus aureus MR – 3.3%.
3. The Results and Their Discussion
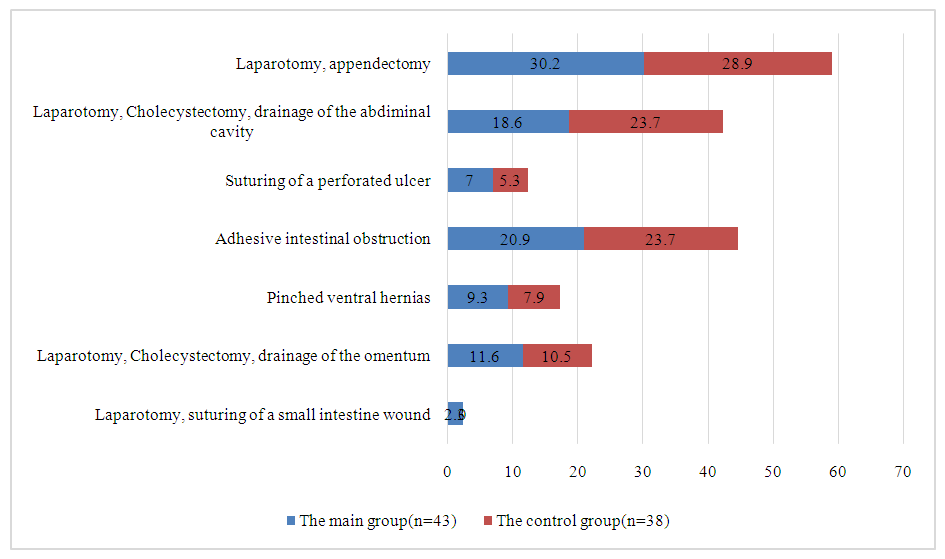
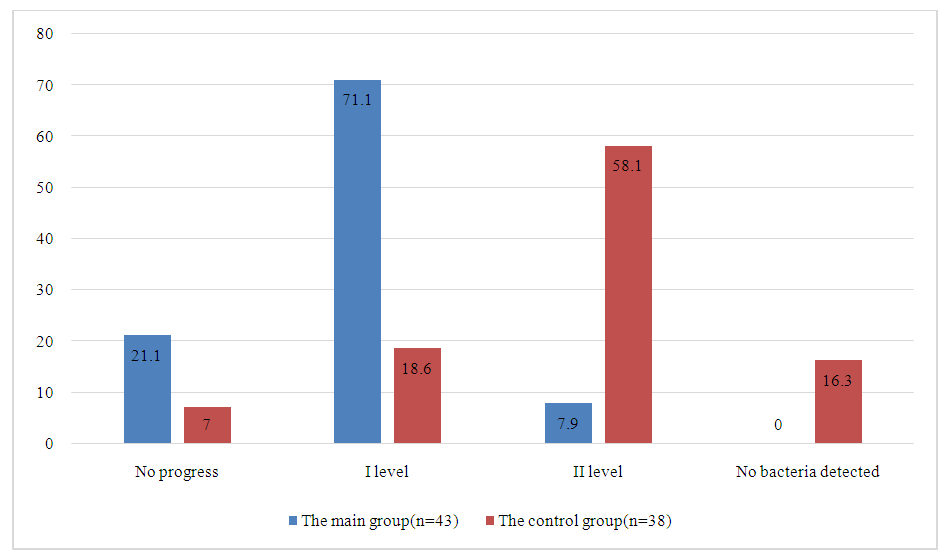
According to the degree of growth of the microflora of the contents of the bronchial tree, in the control group, patients were distributed as follows: I degree of growth of the microflora of the contents of the bronchi was detected in 7 patients (18.42%), II degree - in 9 patients (23.68%), III degree - in 9 patients (23.68%), grade IV - in 13 patients (34.21%).When examining the contents of the bronchial tree, in the group where sanitary bronchoscopy was performed using MB, the following were revealed: I degree of growth of the microflora of the contents of the bronchi was detected in 8 patients (18.6%), II degree - in 10 patients (23.25%), III grade - in 11 patients (25.58%), grade IV - in 14 patients (32.55%). The data is presented in Figure 3.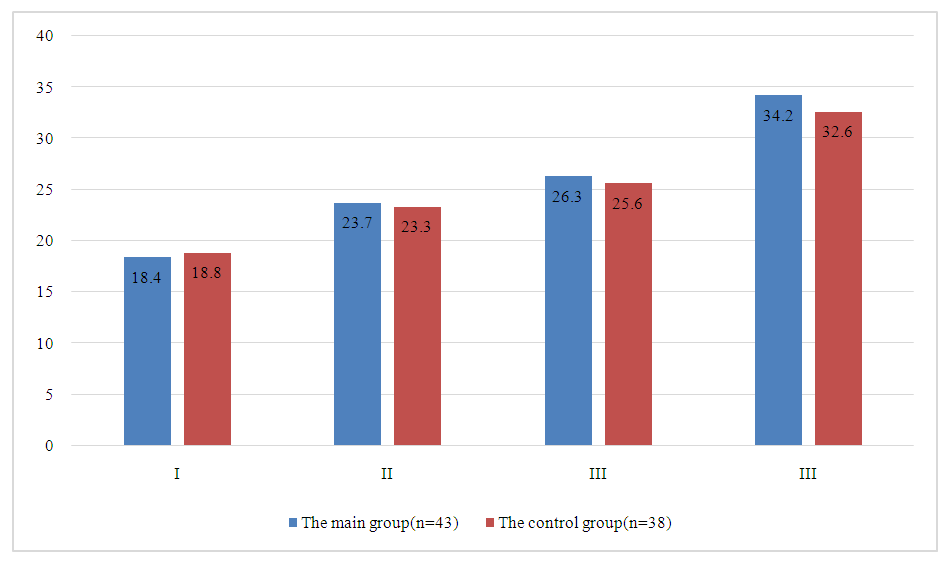 | Figure 3. Initial degree of growth of the microflora of the bronchial tree in patients with purulent tracheobronchitis |
Most of the patients in both the first and second groups had IV degree of microflora growth - 34.21% and 32.55%, respectively.When using a solution of furatsilin at a concentration of 1:5000 nm, as a rule, it was possible to reduce the degree of growth of the contents of the bronchial tree by the first degree. We obtained such results in 35 patients (73%). In 3 (6.2%) patients, the degree of microflora growth decreased by two degrees. In 10 patients (20.8%) the flora was without dynamics.The use of photodynamic sanitation allowed us, as a rule, to reduce the degree of growth of the contents of the bronchial tree by two degrees.We obtained such results in 25 patients of the main group (58.13%). In 8 (18.6%) patients there was a decrease in height by one degree. In 7 (16.27%) patients, no pathological flora was cultured after sanitation bronchoscopy with photodynamic sanitation with MS. In 3 patients (6.97%) there was growth of microflora without dynamics. The data is presented in Figure 4.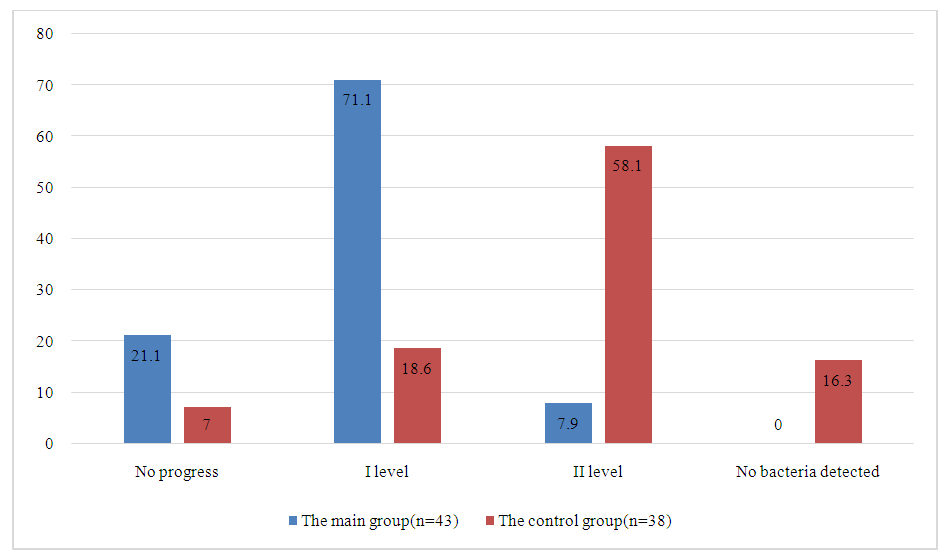 | Figure 4. Dynamics of changes in microbial contamination of the bronchial tree in the main and control groups of patients |
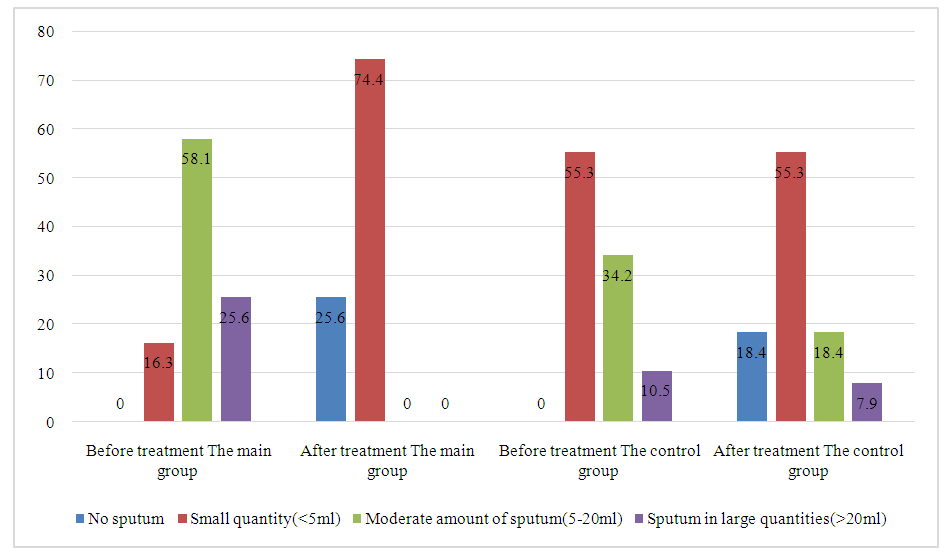
In the control group, after sanitary bronchoscopy with standard solutions, in 71.05% (27 patients) of cases, it was possible to reduce the degree of growth of the microflora of the bronchial tree to the first degree. In 3 (7.89%) patients there was a decrease in height by one degree. In 8 patients (21.05%) there was growth of microflora without dynamics.We studied the clinical aspects of the use of FBTS in the main and control groups of patients. In the intra- and postoperative period, sputum was detected in all patients during fiberoptic bronchoscopy (Figure 5).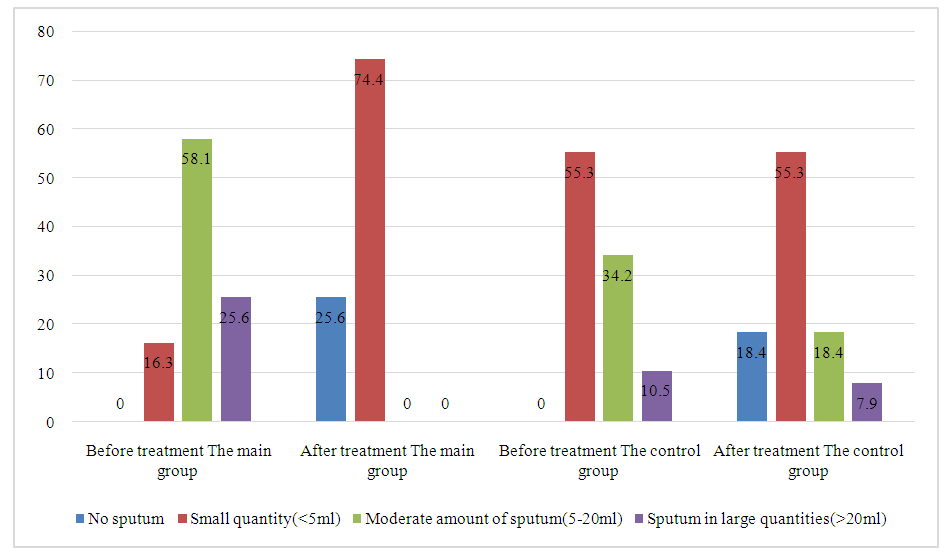 | Figure 5. Change in the amount of sputum during fibrobronchoscopy in patients before and after treatment (in ml) |
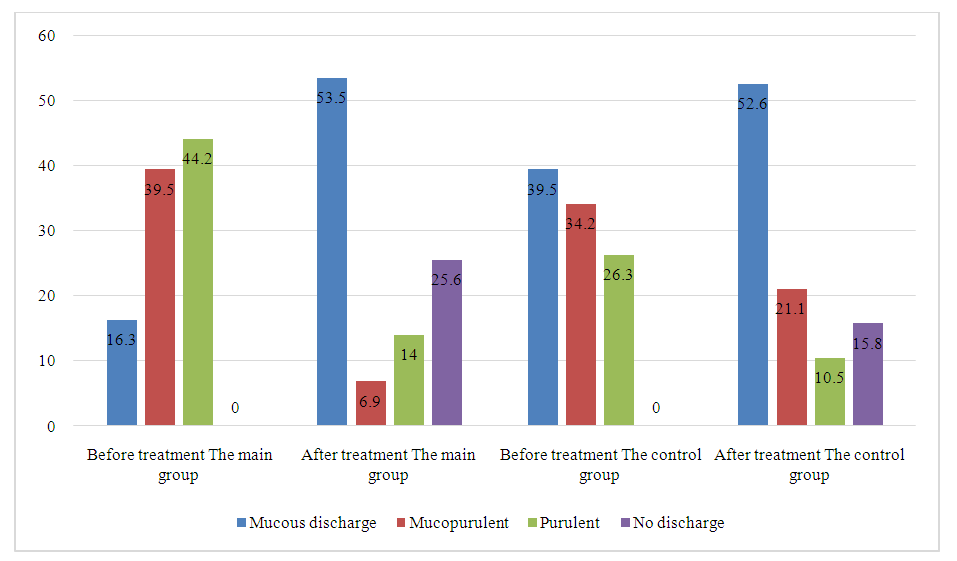
It should be noted that in the main group the number of patients with 5 ml or more of sputum in the bronchial tree was 39% higher than in the comparison group before treatment.After treatment in the main group, not a single patient had sputum in a volume of 5 ml or more. 74.4% of patients had up to 5 ml of sputum, and 25.6% of people had none at all. In the comparison group, after treatment, sputum remained in the bronchial tree in 81.6% of patients, including in a volume of 5-20 ml in 18.4%, more than 20 ml in 7.9%. Consequently, in the main group after treatment there were no patients with the amount of sputum in the bronchi of 5 ml or more, while in the comparison group it was observed in 18.4% of patients (p <0.001).Before treatment, the number of patients with mucous discharge in the bronchial tree in the main group was 23.2% (p <0.005) less than in the comparison group, and the number of patients with purulent discharge was 17.9% more. p <0.02, Fig. 6).After treatment in the main group, the number of patients with mucopurulent and purulent discharge in the bronchial tree decreased by 62.7% (p <0.001). The number of patients with mucous discharge increased by 36.2% (p <0.001); in another 25.6% of patients, the discharge in the bronchial tree completely disappeared (Fig. 6).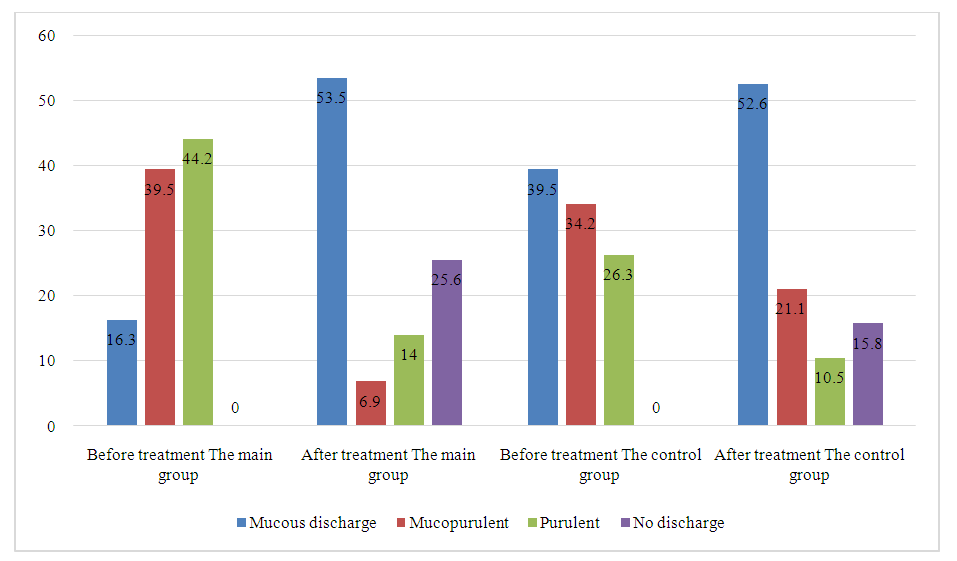 | Figure 6. The nature of sputum in the tracheobronchial tree in patients of the main and control groups before and after treatment |
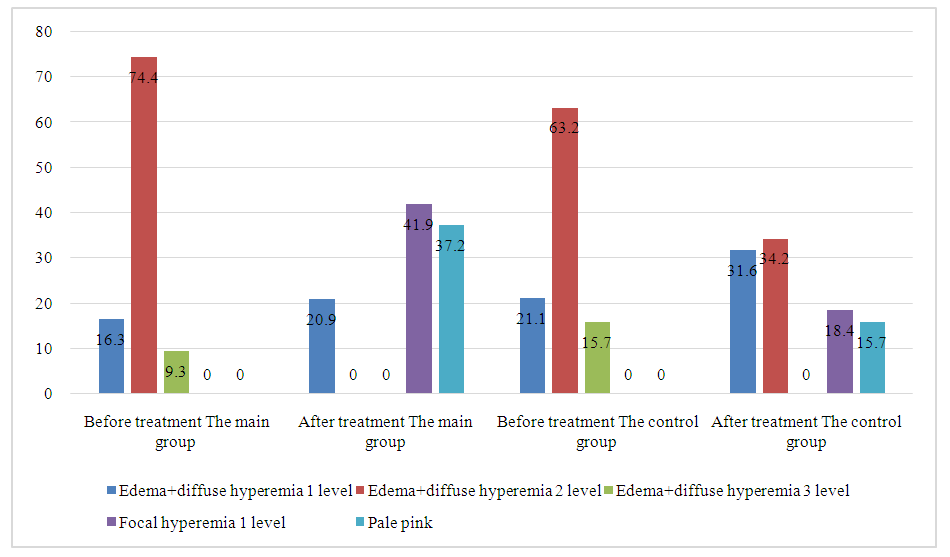
After treatment in the comparison group, the number of patients with purulent discharge in the bronchial tree decreased by 15.8% (p <0.05), and with mucous discharge increased by 11.0% (p <0.05). After treatment in the main group, the number of patients with mucopurulent discharge became smaller, on average by 14.2% (21.1-6.9=14.2%) (p <0.05) than in the comparison group, and the number of patients with the absence of contents in the bronchial tree is 9.8% more (p<0.05).Consequently, the number of patients with mucopurulent and purulent sputum in the main group after treatment decreased by approximately 62.8% (p <0.001), while in the comparison group these changes were not so significant and amounted to 28.9% (p <0.05).Before treatment, the indicators of the condition of the mucous membrane of the bronchial tree did not differ statistically significantly between the groups of patients (Fig. 7).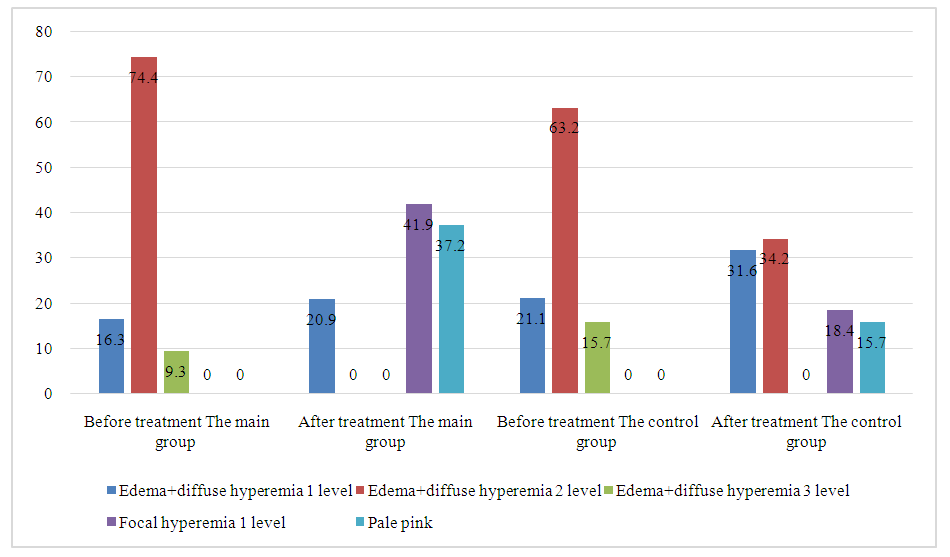 | Figure 7. Condition of the mucous membrane of the tracheobronchial tree in patients of the main and control groups |
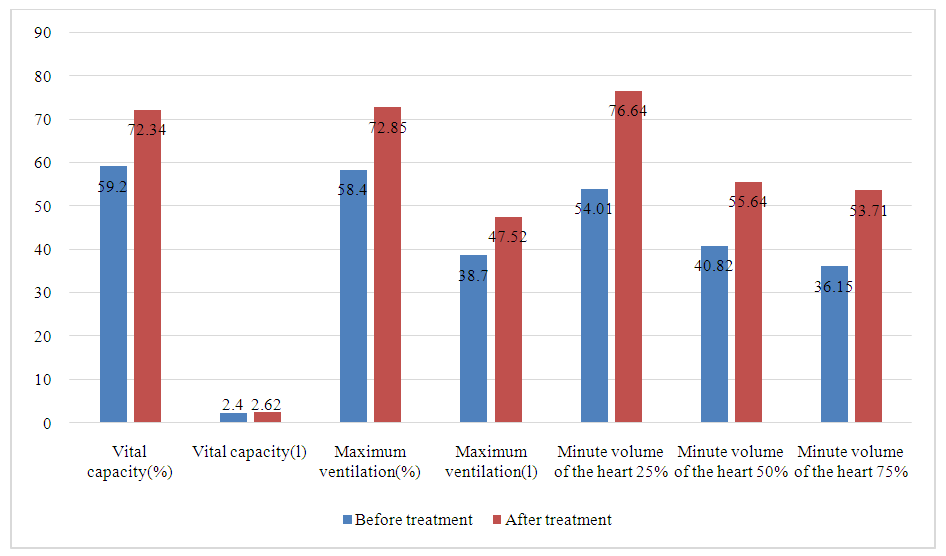
In the main group of patients after treatment, there were no patients with edema in combination with diffuse hyperemia of degrees 2 and 3; in 41.9% of patients, focal hyperemia of grade 1 began to be determined, and in 37.2% of patients, the bronchial mucosa became pale pink.In the comparison group after treatment, the number of patients with edema and diffuse hyperemia of grade 2 decreased from 63.2% to 34.2% (p <0.001), and there were no patients with edema and diffuse hyperemia of grade 3. In 18.4% of patients, focal hyperemia of the 1st degree was detected and in 15.7% of patients the bronchial mucosa was pale pink.Thus, with the same initial indicators of the nature of the mucous membrane of the bronchial tree, there is a sharp increase in the number of patients with normal bronchial mucosa in the main group, while in the comparison group there were fewer of them by 21.5% (p < 0.05). The number of patients with normal bronchial mucosa increased significantly. focal hyperemia (41.9%), while in the comparison group there were 23.5% fewer of them (p < 0.002). It is noteworthy that there were no more patients with edema and diffuse hyperemia of degree 2 in the main group after treatment, and in the comparison group there were 34.2% (p < 0.05).Nebulizer PDT with MBwas effective and was accompanied by a decrease in signs of endotoxemia (decrease in body temperature, leukocytosis, amount of purulent discharge from the tracheobronchial tree) and acute respiratory failure (increase in the oxygenation index, decrease in scores on the CPIS scale - Clinical Assessment of Pulmonary Infection Scale) for 2. 3±1.2 days from the start of treatment in the main group and for 5.2±1.5 days in the control group.Thus, the use of inhalation PDT with MB is effective and safe as an addition to systemic antibacterial therapy in the treatment of severe tracheobronchitis, including nosocomial pneumonia, caused by multidrug-resistant gram-negative pathogens.We examined indicators of external respiratory function (ERF) in all observed patients. ERF indicators also underwent positive dynamics, but less pronounced than other indicators. Figure 8 shows the dynamics of the main indicators of respiratory function in patients in the control group before and after treatment (n=38).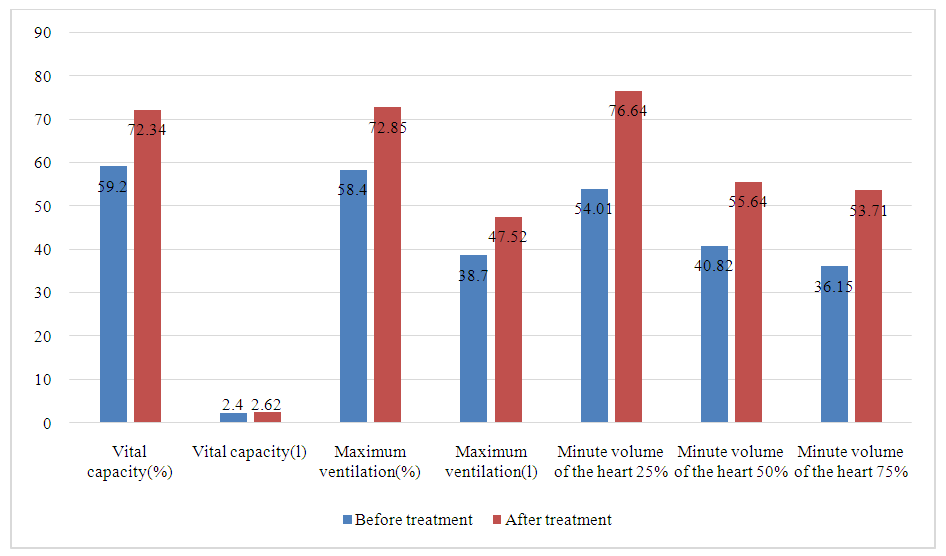 | Figure 8. Dynamics of the main indicators of respiratory function in patients of the main group before and after treatment (n=43) |
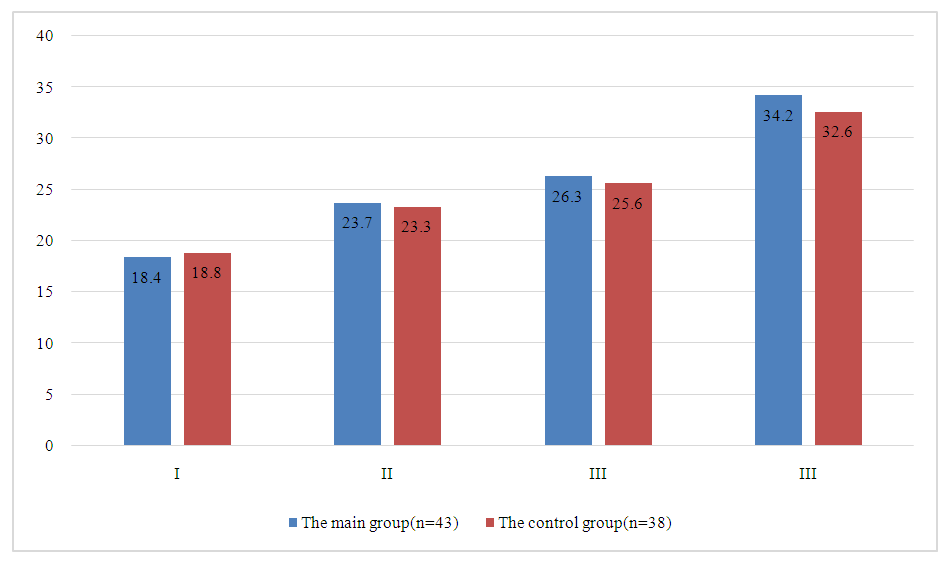
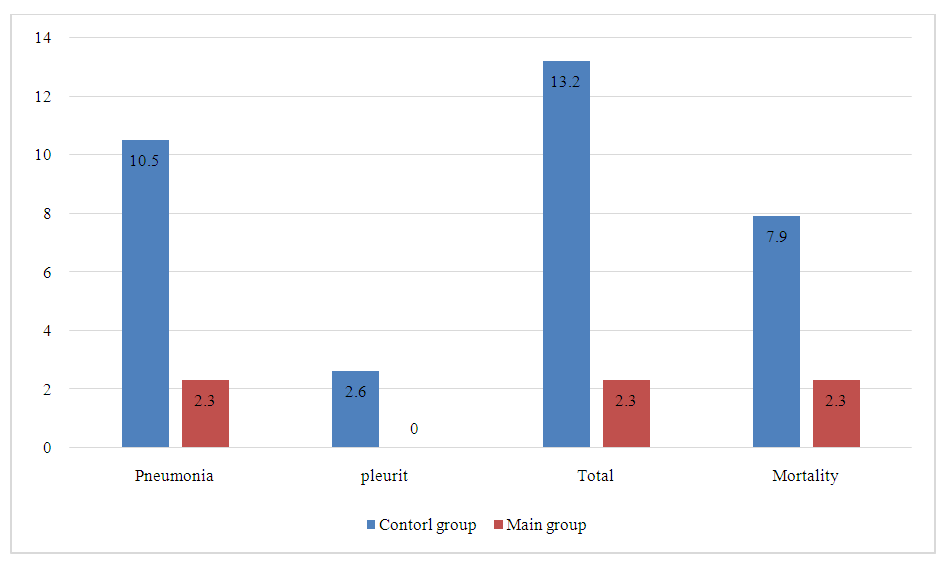
The effectiveness of the use of photodynamic bronchoscopic sanitation in the treatment of purulent-inflammatory diseases of the bronchi is evidenced by the following data. VC indicators (%) increased from 59.2±3.06 to 72.34+3.21, ERF (%) from 58.4±6.36 to 72.85±3.21. All this indicates an improvement in respiratory function, which is also confirmed by the dynamics of indicators characterizing both pulmonary ventilation and bronchial patency (Figure 8).Under the influence of the treatment carried out in patients of the main groups, along with an improvement in clinical data and respiratory function indicators, positive dynamics of endoscopic signs were observed.The nature of postoperative complications associated with the respiratory system in patients with lung diseases is presented in Figure 9.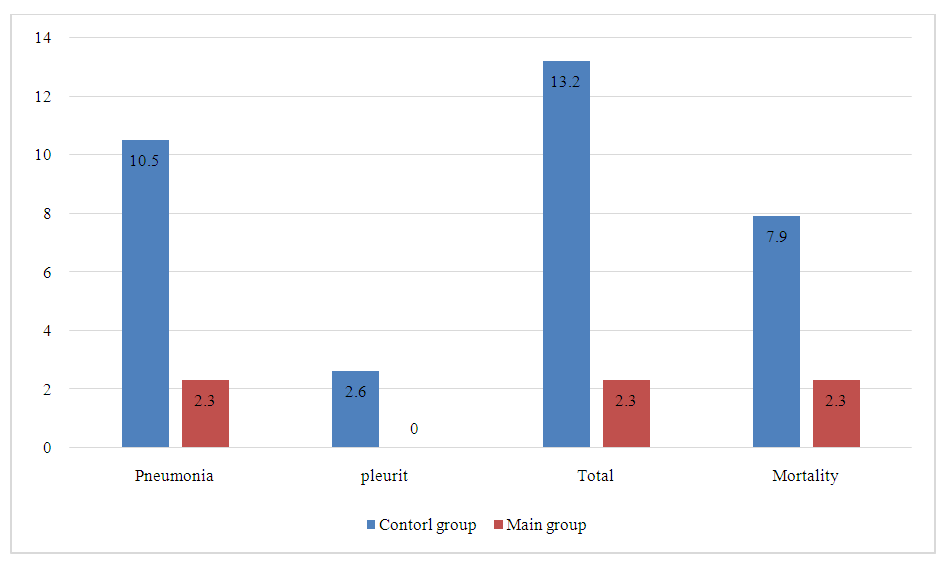 | Figure 9. Postoperative complications associated with the respiratory system |
From Figure 9 it follows that in the group with PD sanitation with MB solution, the occurrence of respiratory complications in the postoperative period was noted in 2.3±2.3%, while when using standard solutions the development of pneumonia was noted in 10.5±5.0% and pleurisy developed in 2.6±2.6% of cases.In the control group, three patients who were operated on for generalized peritonitis died. The causes of death in two were multiple organ failure, and in one, purulent tracheobronchitis and confluent bilateral pneumonia. In the main group, 1 patient died after being operated on for generalized peritonitis. The cause of death was multiple organ failure. From the side of the tracheobronchial tree, the phenomena of tracheobronchitis are 1-2 degrees.Carrying out PD sanitation bronchoscopy with MB gave good results after the first sanitation in 74.4%. Satisfactory results in 10 (23.25%) patients. In the main group there was 1 (2.3%) death. It should be noted that the immediate cause of death was ongoing widespread peritonitis; pathological studies did not reveal progression of pathology from the respiratory system.Our studies have shown that the use of sanitation bronchoscopy must begin during surgery and continue in the early stages after surgery, which prevents the development of postoperative complications from the respiratory system, the fight against which takes a lot of time and effort, and is accompanied by large material costs. Based on the above results, it has been proven that the use of photodynamic sanitation bronchoscopy with MB significantly enhances the therapeutic effect. The best therapeutic effect was achieved in the groups where sanitation was carried out using PD sanitation with MB. The use of MB solution does not require significant material costs, and a good therapeutic effect is achieved.
4. Conclusions
The most common causative agents of postoperative purulent tracheobronchitis in emergency abdominal surgery are pathogenic bacteria S. Aureus -10.7%, Staphylococcus aureus MR - 3.3%, Acinetobacter spp. - 6.2%, Esherichia coli - 18.2%, Klebsiella pneumonia - 6%, Pseudomonas aeruginosa -10.7% and Candida fungi -10.7%.The use of MB solution sensitized by laser radiation at a concentration of 0.05%, laser radiation exposure time of 3 minutes, energy density of 99 J/cm2 in patients with severe tracheobronchitis, operated on for acute surgical diseases of the abdominal organs, was found to be effective in sanitation bronchoscopy, respectively. 72, 22%. Moreover, the use of standard solutions was effective in 6.2% of patients in the control group.The developed method of nebulizer photodynamic antibacterial therapy of purulent tracheobronchitis using a 0.05% MB solution is effective and safe as an addition to systemic antibacterial therapy in the treatment of purulent tracheobronchitis.
References
| [1] | О проблемах лечения распространенного гнойного перитонита / А. М. Карсанов, С. С. Маскин, А. А. Хасиева [и др.] // Современная наука: актуальные проблемы теории и практики. Серия: Естественные и технические науки. – 2020. – № 8. – С. 168-172. |
| [2] | Савельев, В. В. Пятнадцатилетний опыт использования интегральной шкалы «Индекс брюшной полости» при установлении показаний к этапному хирургическому лечению распространенного перитонита / В. В. Савельев, М. М. Винокуров, В. В. Французская // Якутский медицинский журнал. – 2021. – №. 1. – С. 39-43. |
| [3] | Турсуметов А.А., Исаков Ш.Ш. Фотодинамическая терапия - инновационный метод борьбы с антибиотикорезистентными бактериями в хирургии// Евразийский Вестник Педиатрии. - 2022. -№ 2(13). -С. 33-39. |
| [4] | Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Vidal Melo MF. Postoperative Pulmonary Complications, Early Mortality, and Hospital Stay Following Noncardiothoracic Surgery: A Multicenter Study by the Perioperative Research Network Investigators. JAMA Surg. 2017 Feb 1; 152(2): 157-166. doi: 10.1001/jamasurg. 2016.4065. |
| [5] | Odor PM, Bampoe S, Gilhooly D, Creagh-Brown B, Moonesinghe SR. Perioperative interventions for prevention of postoperative pulmonary complications: systematic review and meta-analysis. BMJ. 2020 Mar 11; 368: m540. doi: 10.1136/bmj.m540. |
| [6] | Schultz MJ, Hemmes SN, Neto AS, et al. LAS VEGAS investigators Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS - an observational study in 29 countries. Eur J Anaesthesiol 2017; 34: 492-507. 10.1097/EJA.0000000000000646. |
| [7] | Kawasaki K, Yamamoto M, Suka Y, et al. Development and validation of a nomogram predicting postoperative pneumonia after major abdominal surgery. Surg Today. 2019; 49(9): 769-777. doi: 10.1007/s00595-019-01796-8. |
| [8] | Organisation for Economic Co-operation and Development (OECD) and European Centers for Disease Control and Prevention. Antimicrobial Resistance: Trackling the Burden in the European Union. OECD Publications; Paris, France: 2019. Briefing Note for EU/EEA Countries. |
| [9] | Cieplik F., Deng D., Crielaard W., Buchalla W., Hellwig E., Al-Ahmad A., Maisch T. Antimicrobial photodynamic therapy-What we know and what we don’t. Crit. Rev. Microbiol. 2018; 44: 571–589. doi: 10.1080/1040841X.2018.1467876. |
| [10] | Hamblin MR. Antimicrobial photodynamic inactivation: a bright new technique to kill resistant microbes. Curr Opin Microbiol. 2016 Oct; 33: 67-73. doi: 10.1016/j.mib.2016.06.008. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML