-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 382-385
doi:10.5923/j.ajmms.20241402.47
Received: Jan. 19, 2024; Accepted: Feb. 15, 2024; Published: Feb. 19, 2024

Features of the Course of Acute Coronary Syndrome with ST Elevation in Patients with Concomitant Coronavirus Infection COVID-19
Atamuratov B. R., Fozilov Kh. G., Abdullaeva S. Ya., Yuldashov B. A., Yuldashov A. A., Ermetova A. M.
Republican Specialized Scientific and Practical Medical Center of Cardiology of the Ministry of Health of the Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim. Study and comparison of the features of the course of acute coronary syndrome (ACS) with ST elevation in patients who have had COVID-19 infection. Materials and methods. A study was carried out on 114 patients with ACS with ST segment elevation who were admitted to the Russian National Medical Research Center from January 2021 to February 2022 (during the COVID-19 pandemic). The patients were divided into 2 groups. The first group included patients who had COVID-19, and the second group without a history of COVID-19. Results. COVID-19 infection has a negative impact on the course of acute coronary syndrome with ST elevation. Transformation of ACS with ST elevation into myocardial infarction with Q wave was observed significantly more often in patients who had COVID 19 than in patients without a history of COVID 19.
Keywords: ACS with ST segment elevation, COVID-19
Cite this paper: Atamuratov B. R., Fozilov Kh. G., Abdullaeva S. Ya., Yuldashov B. A., Yuldashov A. A., Ermetova A. M., Features of the Course of Acute Coronary Syndrome with ST Elevation in Patients with Concomitant Coronavirus Infection COVID-19, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 382-385. doi: 10.5923/j.ajmms.20241402.47.
1. Relevance
- Due to the fact that coronavirus infection has a significant impact on the decompensation of existing chronic diseases, specific damage to the cardiovascular system, patients with coronary artery disease and COVID-19 are identified as a special risk group [1].New cases of heart failure, myocardial infarction, acute cerebrovascular accident among patients after a coronavirus infection develop 3 times more often than in patients in the population who have not had COVID-19 [2,3]. Katsoularis I., et.al., having studied data from the Swedish registry, showed that COVID-19 is a risk factor for the development of myocardial infarction and stroke, which in the future may become a clinical and social problem [4]. Huang S. et al. (2020) recorded that six months after suffering from COVID-19, almost a third of patients reported chest pain, shortness of breath or palpitations [5,6]. At the same time, complaints from the cardiovascular and respiratory systems can develop even against the background of low-symptomatic and asymptomatic COVID-19, and not only after severe and moderate course of the disease [7].Purpose of the study: To study and compare the characteristics of the course of acute coronary syndrome (ACS) with ST elevation in patients who have had COVID-19 infection.
2. Materials and Methods
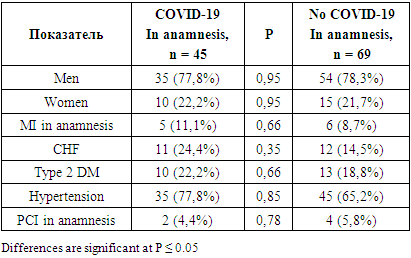
- A single-center prospective study conducted at the Republican Specialized Scientific and Practical Medical Center of Cardiology (RSNPMCC). The study included all ST-segment elevation ACS patients admitted from January 2021 to February 2022 (during the COVID-19 pandemic). These patients were compared with a group of patients who did not have COVID-19 infection and were hospitalized for ACS during a similar period of time. A total of 114 patients were included in the study. In all patients, the presence in the blood of IgG antibodies to the causative agent of coronavirus infection COVID-19 was determined in a laboratory, which indicates whether the person has already had coronavirus infection or not. The patients were divided into 2 groups: the first group included 45 patients diagnosed with COVID-19, and the second group included 69 patients who had not had COVID-19, among them 78.3% were men (54), and 21 women .7% (15). The following indicators were assessed in all patients: the time of pain before coronary angiography, the onset of coronary artery disease/coronary artery disease in the anamnesis, the incidence of cardiogenic shock, the presence of ST-segment elevation myocardial infarction, the combination of heart attack and diabetes mellitus, as well as the number of deaths during hospitalization. Statistical analysis was performed using STATISTICA 12 software.
3. Results
- The two groups were comparable on basic demographic and clinical parameters. The mean age in the groups was: 63.4 ± 9.0 years in the COVID-19 group and 60.2 ± 11.7 years in the control group, p = 0.11. The ratio of men to women did not differ significantly between the groups: 77.8% of men in the group with a history of COVID-19 and 78.3% in the second group (p = 0.78). In both groups, men significantly prevailed: 77.8% to 22.2% in the first group and 78.3% to 21.7%, p = 0.00001 (Table 1).
|
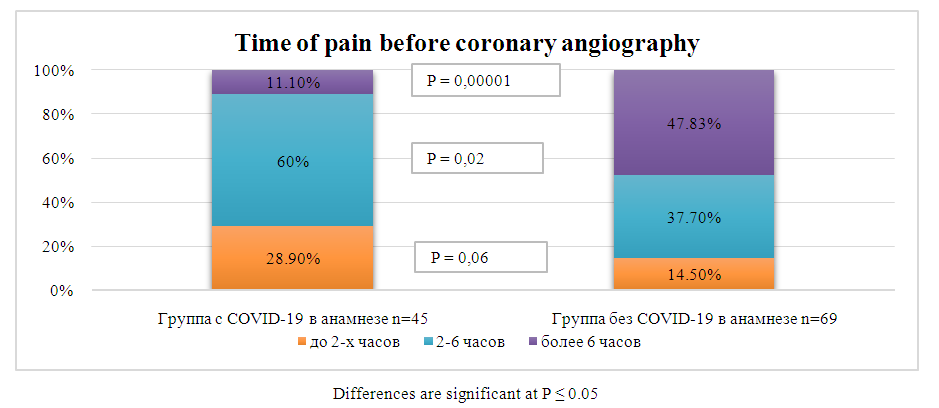 | Figure 1. Time of pain before coronary angiography in groups |
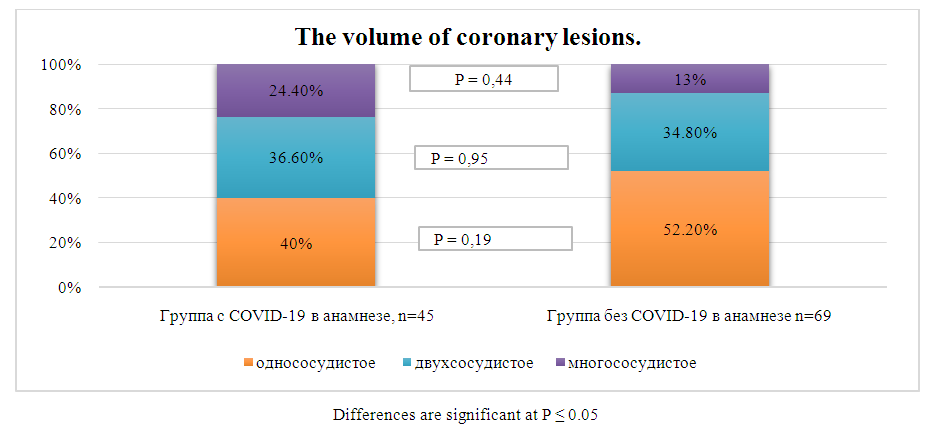 | Figure 2. Volume of coronary lesions in groups |
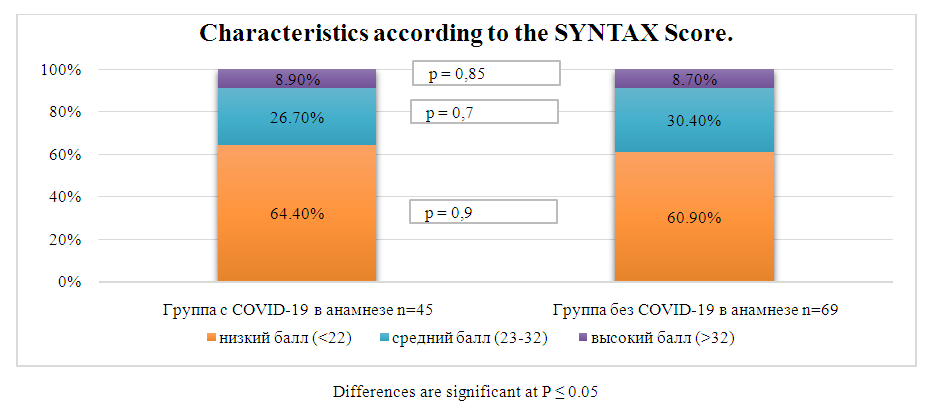 | Figure 3. Characteristics according to the SYNTAX Score in groups |
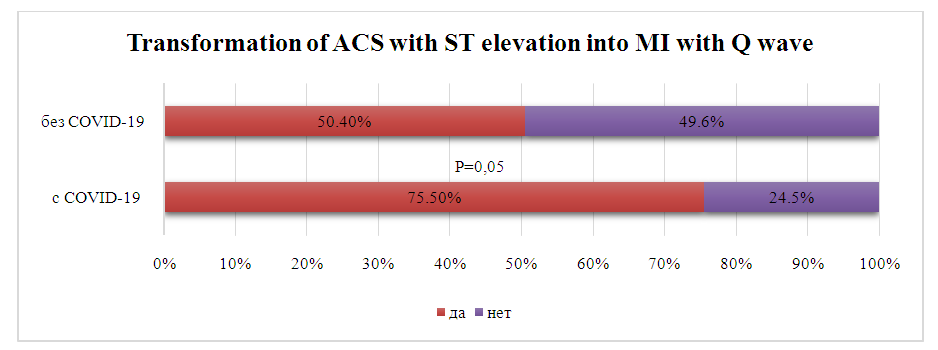 | Figure 4. Transformation of ACS with ST elevation into MI with Q wave, in groups |
4. Discussion
- Pathology of the cardiovascular system is often found in patients who have had coronavirus infection, regardless of the severity of the disease. Cardiovascular diseases are observed both in patients who have had a severe course of COVID-19, and in patients undergoing outpatient treatment, and even in people with no obvious symptoms of coronavirus infection. Endothelial dysfunction, hemodynamic disorders, microvascular inflammation, disturbances in the hemostatic system and an increased risk of thrombosis can lead to the development of ischemic disease, including ACS [2,8]. For early diagnosed chronic ischemic heart disease. COVID-19 can be a cause of plaque rupture increasing. The mechanism of this phenomenon is associated with a sharp increase in the level of interleukin-6. This pro-inflammatory cytokine is a trigger for atherosclerotic plaque instability, one of the main factors of atherothrombosis. [7,9] Rupture of an atherosclerotic plaque can lead to myocardial infarction, which significantly increases the risk of death. According to some authors, mortality from acute myocardial infarction in COVID-19 is 40% [10]. The data obtained by the authors also demonstrate that COVID-19 infection has a negative impact on the course of acute coronary syndrome with ST elevation. Transformation of ACS with ST elevation into myocardial infarction with Q wave was observed significantly more often in patients who had COVID 19 than in patients without a history of COVID 19: 75.5% to 59.4%, p<0.05. There was a tendency towards a higher incidence of cardiogenic shock, 4.4% to 1.45%, among those who had not recovered from the disease; the percentage of deaths during hospitalization in patients who had recovered from COVID 19 was also, although unreliably, higher compared to those who had not recovered from the disease - 4.4% to 1.45%. With regard to the volume and severity of damage to the vascular bed, no significant differences were found between the groups.
5. Conclusions
- 1. With regard to the volume and severity of damage to the vascular bed, no significant differences were found between the groups.2. The transformation of ACS with ST elevation into myocardial infarction with Q wave occurs significantly more often in patients who have had COVID 19.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML