-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 4(2): 352-355
doi:10.5923/j.ajmms.20241402.41
Received: Jan. 10, 2024; Accepted: Feb. 7, 2024; Published: Feb. 12, 2024

The Impact of Laser Treatment on Glaucoma
A. F. Yusupov1, M. X. Karimova1, Sh. A. Jamalova2, N. O. Umarova3
1Doctor of Medical Sciences, Professor, Republican Specialized Scientific Practical Medical Center of Microsurgery of the Eye, Uzbekistan
2Doctor of Medical Sciences, Associate Professor, Republican Specialized Scientific Practical Medical Center of Microsurgery of the Eye, Uzbekistan
3PhD Post-Graduate Course Student, Republican Specialized Scientific Practical Medical Center of Microsurgery of the Eye, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective. to evaluate the effectiveness of treating primary open-angle glaucoma (POAG) using micropulse laser trabecuplasty (MLT) with a laser device at a wavelength of 577 nm for 360° exposure. Methods: the examination included 54 patients with unstabilized POAG divided into two groups. The 1st group 21 patients underwent SLT, and the 2nd group 33 patients underwent MLT. The MLT group was further divided into 2 subgroups: 14 patients underwent MLT with a power of 1000 mW, duty cycle of 10%; and 19 patients underwent MLT with a power of 1000 mW, duty cycle of 15%. Results: the mean pretreatment IOP values were similar in the SLT and MLT groups, but one hour after laser trabeculoplasty in the SLT group, 5 patients (24%) experienced a pressure increase greater than 3 mmHg. At the 6-month follow-up, the SLT and MLT groups with a duty cycle of 15% exhibited similar success, with a reduction in IOP values of more than 20% from the baseline, at 71% and 78%, respectively. The results were similar in terms of OCT and perimeter. Conclusion: аor the treatment of POAG, MLT emerges as a novel method that operates without causing thermal damage to the pigment cells of the trabecular meshwork. Importantly, the group of patients undergoing MLT reported no discomfort during and after treatment, and there were no spikes in IOP following the laser procedure compared to the group receiving SLT.
Keywords: Open-angle glaucoma, Micropulse laser trabeculoplsty, Intraocular pressure
Cite this paper: A. F. Yusupov, M. X. Karimova, Sh. A. Jamalova, N. O. Umarova, The Impact of Laser Treatment on Glaucoma, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 352-355. doi: 10.5923/j.ajmms.20241402.41.
1. Introduction
- When selecting treatment for unstabilized glaucoma, the primary focus is on stabilizing the process, achievable primarily through laser treatment methods [9]. Laser trabeculoplasty, utilizing an argon laser, demonstrated significant success in stabilizing the process. However, in the long term, it presented some complications, leading Latina and Park to develop selective laser trabeculoplasty (SLT) in 1995 [6,7]. With SLT, laser exposure is exclusive to the pigmented cells of the trabecular meshwork. SLT has achieved comparable success to argon laser trabeculoplasty (ALT) and has demonstrated long-term intraocular pressure (IOP) stabilization, proving its therapeutic efficacy in numerous prospective and randomized studies [3,5,7,8,10].Ingvoldstad and colleagues reported a randomized trial of micropulse laser trabeculoplasty (MPL) for glaucoma at the 2005 annual meeting of the Association for Research in Vision and Ophthalmology [4]. The study aimed to achieve a reduction in IOP similar to ALT without thermal damage, a hypothesis confirmed by histological examination of the trabecular region of the anterior chamber angle [3,12]. Subsequently, many authors conducted studies examining the effect of MLT on IOP [1,2,4,11]. However, to this day, there is no definitive postulate for the treatment of glaucoma with MLT, and there are no large randomized studies proving the therapeutic effect of MLT.Purpose of the study: to evaluate the effectiveness of treating primary open-angle glaucoma (POAG) using MLT with a laser device at a wavelength of 577 nm for 360° exposure.
2. Material and Methods
- The examination included 54 patients (62 eyes) with unstabilized POAG divided into two groups. The 1st group (21 patients (26 eyes)) underwent SLT, and the 2nd group (33 patients (36 eyes)) underwent MLT. The MLT group was further divided into 2 subgroups: 14 patients (15 eyes) underwent MLT with a power of 1000 mW, duty cycle of 10%; and 19 patients (21 eyes) underwent MLT with a power of 1000 mW, duty cycle of 15%. The age of the patients ranged from 40 to 78 years. The average age of patients was: SLT group – 62 years; MLT with a duty cycle of 15% - 56; with a duty cycle of 10% - 61. There were 32 women and 22 men. Most patients had stage II primary open-angle glaucoma - 63%, with 37% having stage I primary open-angle glaucoma. Patients had no previous history of antiglaucomatous surgeries or laser procedures. The examination considered the conservative treatment received before and after laser treatment. The combination of antihypertensive drops received by patients was calculated as 2 separate antihypertensive agents.In the MLT patient group, the procedure was performed using an Easyret unit (Quantel Medical, France) with a wavelength of 577 nm on a 360° micropulse unit with a power of 1000 mW, a duty cycle of 10% and 15%, duration 300 ms, and a spot size of 300 μm per area of pigmented trabecular meshwork.In a group of patients who underwent selective laser trabeculoplasty, the procedure was performed using an Nd:YAG laser system Q-LAS (A.R.C. Laser, Germany) at 360° with a wavelength of 532 nm at double frequency. The SLT energy was titrated from 1.0-2.0 mJ per pigmented area of the trabecular meshwork until the formation of a gas bubble was achieved; the spot size was 400 μm, and the duration was 3 ns.After laser treatment, patients were prescribed topical non-steroidal anti-inflammatory eye drops for 10 days to reduce the inflammatory response. At each visit, the anterior segment was examined, best-corrected visual acuity was determined, and IOP was measured. IOP measurements were carried out an hour after the laser procedure, also on the 10th day, after 1, 3, and 6 months. IfIOP values were unstable or there were changes in the visual field, laser treatment was considered unsuccessful. After the procedure, laser trabeculoplasty was deemed successful when the IOP was reduced by more than 20%.
3. Results
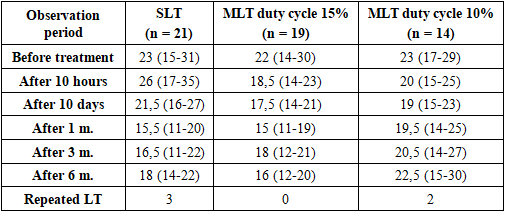
- The mean pretreatment IOP values (Table 1) were similar in the SLT and MLT groups, but one hour after laser trabeculoplasty in the SLT group, 5 patients (24%) experienced a pressure increase greater than 3 mmHg. Conversely, in the MLT group (in both subgroups), an hour later, there was a decrease in IOP. None of the groups exhibited inflammation of the anterior chamber of the eye when examined at 10 days and during subsequent follow-ups. The treatment proceeded without complications in 100% of cases: no thermal pain, unpleasant laser flashes, or peripheral anterior synechiae. Visual acuity remained unchanged in all eyes.
|
 | Figure 1. The indicators of mean deviation of light sensitivity in perimetry |
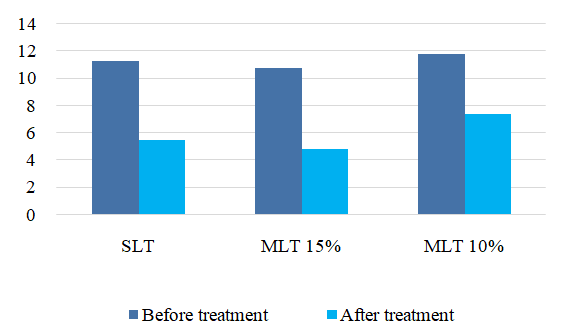
 | Figure 2. The number of medications used before and after treatment |
4. Discussion
- The concept behind a pulsed laser delivery system is to minimize thermal energy, thus reducing physiological damage to ocular tissue. SLT and MLT differ in their mechanisms of action. SLT targets intracellular melanin and activates macrophages [3], selectively damaging pigmented cells in the trabecular meshwork, which may lead to postoperative inflammation and IOP surges. MLT, conversely, thermally affects trabecular cells without destroying them, providing a cooling period between pulses, thereby preventing tissue destruction.The aim of MLT is to stimulate a biological response in the trabecular meshwork while minimizing tissue damage (10-15% duty cycle), as opposed to delivering a continuous laser wave (100% duty cycle) into the trabecula.In the results of our studies, the maximum reduction in IOP was achieved on day 1, and the most significant reduction effect at 6 months was observed in the groups with SLT and MLT with a duty cycle of 15%.From our studies, MLT with a duty cycle of 15% exposure to 360° resulted in a treatment success rate of 72%, comparable to the findings of Fea and colleagues [2]. Their study, using MLT with a wavelength of 810 nm, showed a 75% reduction in IOP, with more than a 20% reduction in 60% of treated patients. In our study, this success rate was achieved using a 577 nm MLT laser with a 360° irradiation area and a 15% duty cycle.Chudoba and colleagues [1] conducted an MLT study in 2014 using a 577 nm setup, targeting the inferior region of the trabecular meshwork. Their study noted a reduction in IOP of 1.7 mmHg compared to baseline, and in non-laser-treated fellow eyes treated with antihypertensive drops, a decrease in IOP of 1.8 mmHg was observed. In 2015, Lee and colleagues reported a 72.9% success rate following MLT using a 577 nm laser with 360° treatment, achieving a 20% reduction in IOP values one month after laser treatment.A noteworthy aspect of our study is the post-laser observation, during which it was found that the group of patients after MLT experienced significantly less pain, and there were no jumps in intraocular pressure, unlike in 24% of cases with SLT.The study had its limitations, as patients undergoing laser treatment were concurrently receiving antihypertensive drops, potentially affecting the results of IOP reduction.However, it is noteworthy that laser treatment is often offered to glaucoma patients who have previously undergone antihypertensive treatment with drops.Our study results demonstrate that laser trabeculoplasty using SLT and MLT exhibits similar efficacy and safety, especially when MLT employs a power of 1000 mW and a duty cycle of 15%. Conversely, using MLT with a 10% duty cycle showed no significant reduction in IOP during the 6-month follow-up period, indicating low efficiency with these laser settings.
5. Conclusions
- For the treatment of primary open-angle glaucoma (POAG), MLT emerges as a novel method that operates without causing thermal damage to the pigment cells of the trabecular meshwork. However, to achieve optimal treatment effects, the impact power must be set at 1000 mW, and the duty cycle should be 15%. This was evidenced by a substantial decrease in IOP over a 6-month observation period. Importantly, the group of patients undergoing MLT reported no discomfort during and after treatment, and there were no spikes in IOP following the laser procedure compared to the group receiving SLT.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML