-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 4(2): 347-351
doi:10.5923/j.ajmms.20241402.40
Received: Jan. 19, 2024; Accepted: Feb. 8, 2024; Published: Feb. 12, 2024

Diagnostic Approach to COVID-19-Associated Myocarditis in Pregnant Women
Anvar A. Tukhtabaev1, Ahmad Kh. Karimov2, Gulchehra M. Tukhtabaeva1
1PhD, Republican Specialized Scientific and Practical Medical Center for Mother and Child, Tashkent, Uzbekistan
2Doctor of Medical Sciences, Professor, Department of Obstetrics and Gynecology in Family Medicine, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

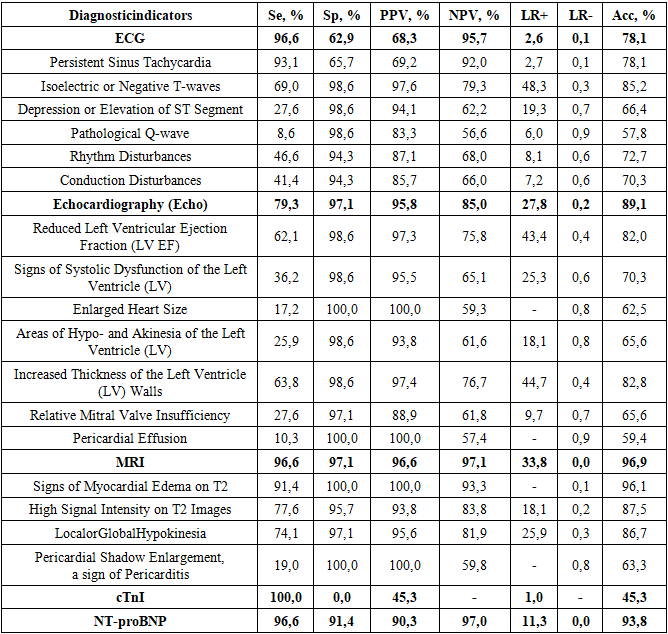
Objective: The aim is to formulate an optimal diagnostic search algorithm for myocarditis associated with COVID-19 in pregnant women. Methods: The research was conducted as an observational, prospective, cross-sectional study, involving a comprehensive examination of patients with the active participation of a cardiologist. Various diagnostic methods were assessed using parameters such as sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+), negative likelihood ratio (LR-), and diagnostic accuracy (Acc, %). Results: The study findings provide an assessment of the effectiveness of different features and parameters on MRI for detecting myocarditis in pregnant women. Notably, indicators like myocardial edema on T2 and high signal intensity on T2 images exhibit high sensitivity and accuracy, whereas pericardial shadow enlargement shows lower sensitivity but higher specificity. Verification of the diagnosis facilitated the computation of specific indicators reflecting the effectiveness of diagnostic methods for COVID-19-associated myocarditis in pregnant women. The results and established diagnostic criteria led to the proposal of a specialized Diagnostic Search and Diagnosis Verification Algorithm. Conclusion: The developed diagnostic search algorithm for confirming the diagnosis of COVID-19-associated myocarditis in pregnant women is based on the evaluation of the diagnostic effectiveness of various clinical, instrumental, and laboratory methods. This algorithm emphasizes the identification of the most informative signs of myocardial involvement, considering limitations associated with pregnancy.
Keywords: COVID-19, Pregnancy, Myocarditis, Diagnostic approach
Cite this paper: Anvar A. Tukhtabaev, Ahmad Kh. Karimov, Gulchehra M. Tukhtabaeva, Diagnostic Approach to COVID-19-Associated Myocarditis in Pregnant Women, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 347-351. doi: 10.5923/j.ajmms.20241402.40.
1. Introduction
- In the context of cardiovascular pathology associated with coronavirus infection in pregnant women, one of the understudied aspects is myocarditis [1]. There are very few publications [1,2,3] in the literature dedicated to this issue. Clinical observations of patients have shown that a significant number of cases have been recorded where clinical and laboratory symptoms of acute myocarditis were frequently noted against the backdrop of COVID-19 in pregnant women.Myocarditis is a significant cause of sudden cardiac death in young individuals, accounting for up to 12% of cases, according to the results of pathological studies [4]. Timely identification of myocarditis can influence the choice of tactics and treatment methods for patients and the prognosis of the disease. One of the controversial aspects in the management of patients with myocarditis currently is the question of diagnostic criteria [2,5].Overall, the issue of diagnosing and differentially diagnosing myocarditis was relevant and not entirely resolved even before the onset of the pandemic. Literature data indicate that the sensitivity of an electrocardiogram for diagnosing myocarditis is quite low (47%). Echocardiography is primarily useful for ruling out other causes of heart failure, as there are no specific signs of acute myocarditis [6]. Cardiac magnetic resonance imaging (MRI) is currently used as a diagnostic method when there is suspicion of myocarditis; however, it should be noted that MRI is most effective when using modes with special contrast enhancement, which poses significant challenges for pregnant women [7,8]. Laboratory biomarkers of cardiac damage are elevated in a small number of patients with acute myocarditis but can help confirm the diagnosis. Troponin I has high specificity (89%) but limited sensitivity (34%) in diagnosing myocarditis [9,10,11,12]. Histological examination with biopsy material collection also does not guarantee confirmation of the diagnosis, even in cases where the technical feasibility of this procedure exists and there are no contraindications [4].In light of the above, there is interest in research to develop optimal approaches to confirm the diagnosis in cases of suspected myocarditis associated with coronavirus infection.Research Objective. To develop an optimal diagnostic search algorithm for COVID-19-associated myocarditis in pregnant women.
2. Materials and Methods
- The work was conducted from 2020 to 2022. Clinical material was collected at the Republican Specialized Scientific and Practical Medical Center of Obstetrics and Gynecology under the Ministry of Health of the Republic of Uzbekistan, the 1st Republican Multidisciplinary Infectious Diseases Hospital, and temporary COVID centers in the city of Tashkent, which operated during the coronavirus infection pandemic.Inclusion criteria for patients in the main group:- pregnancy in the first to third trimesters of gestation;- availability of data on COVID-19 during pregnancy, confirmed by corresponding laboratory tests (PCR and ELISA);- presence of clinical, instrumental (echocardiography, MRI), or laboratory signs of myocarditis, the development of which has a chronological and presumptive cause-and-effect relationship with COVID-19.Exclusion criteria for patients in the main group:presence of chronic cardiovascular diseases in pregnant women's medical history (congenital and acquired heart defects, rheumatism, systemic diseases, etc.).The age of women in the overall sample ranged from 18 to 40 years, with an average age of 26.6±4.1 years. The majority of women (36.4%) were in the age group below 20 years.The study was conducted as an observational prospective cross-sectional investigation. Patient examination was comprehensive and involved the participation of a cardiologist. The diagnostic minimum for all pregnant women included, in addition to general clinical examinations, performing ECG, echocardiography, cardiac MRI (Lake Louise criteria), and special blood biochemical analyses to assess the levels of troponin I (cTnI) and N-terminal pro-B-type natriuretic peptide (NT-proBNP).Each diagnostic method was evaluated based on several parameters, including sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+), negative likelihood ratio (LR-), and diagnostic accuracy (Acc, %).The research materials underwent statistical analysis using parametric and non-parametric methods. Accumulation, correction, systematization of the initial information, and visualization of the obtained results were carried out using Microsoft Office Excel 2016 electronic tables.
3. Results and Discussion
- Table 1 presents the results of assessing the effectiveness of various diagnostic methods for COVID-19-associated myocarditis in pregnant women. The analysis of key indicators for each method showed that the ECG has high sensitivity (Se) - 96.6%, moderate specificity (Sp) - 62.9%, moderate positive and negative predictive values (PPV and NPV) - 68.3% and 95.7% respectively, as well as moderate positive (LR+) and negative (LR-) likelihood ratios - 2.6 and 0.1 respectively. The overall accuracy (Acc) was 78.1%.
|
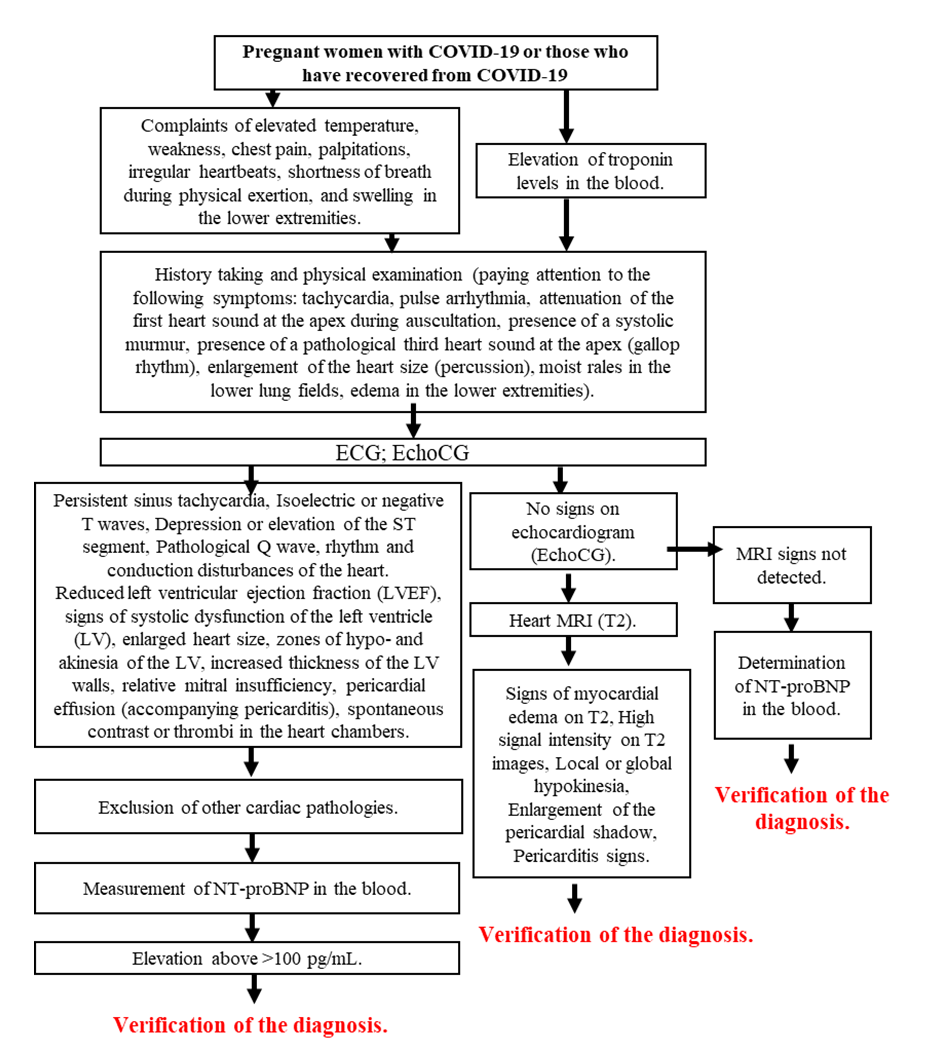 | Figure 1. Diagnostic search and verification algorithm for COVID-19-associated myocarditis in pregnant women |
4. Conclusions
- Thus, based on the evaluation of the diagnostic effectiveness of various clinical, instrumental, and laboratory methods, a diagnostic search algorithm was developed to confirm the diagnosis of COVID-19-associated myocarditis in pregnant women. This algorithm is based on identifying the most informative signs of myocardial involvement, taking into account limitations associated with pregnancy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML