-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 4(2): 303-305
doi:10.5923/j.ajmms.20241402.30
Received: Jan. 12, 2024; Accepted: Feb. 6, 2024; Published: Feb. 8, 2024

Comparison of Methods of Intraoperative Hemostasis in Traumatic Intracranial Hemorrhages
Avazbek R. Mamadaliev1, Kobil T. Khudayberdiev2, Bakhodir N. Davlatov2, Abbosbek B. Mamadaliev2
1Andijan branch of the Republican Scientific Center for Emergency Medical Care, Andijan, Uzbekistan
2Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Severe traumatic brain injury is the leading cause of death among people under 45 years of age. For the most part, this is due to a compressive mechanism (mainly intracranial hematoma), leading to edema and swelling of the brain,as a result of acute cerebral insufficiency. The aim of this study was to compare and identify the advantages and disadvantages of various topical hemostatic agents. To do this, we studied the data of 184 patients with intracranial hemorrhages of various depths and localizations. Intraoperative and immediate results of hemostasis and postoperative complications were evaluated and _ the advantages and disadvantages of the techniques were identified.
Keywords: Traumatic brain injury, Intracranial hematoma, Intraoperative hemostasis, Hemostatic collagen sponge, Hemostatic powder
Cite this paper: Avazbek R. Mamadaliev, Kobil T. Khudayberdiev, Bakhodir N. Davlatov, Abbosbek B. Mamadaliev, Comparison of Methods of Intraoperative Hemostasis in Traumatic Intracranial Hemorrhages, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 303-305. doi: 10.5923/j.ajmms.20241402.30.
Article Outline
1. Introduction
- Surgical removal of intracranial hematomas is one of the main treatment options for traumatic brain injury. In modern neurosurgery, one of the unsolved problems remains the problem of achieving hemostasis after the main stage of the operation [2,3]. This is explained by the fact that it is undesirable to carry out excessive coagulation, clipping or ligation of blood vessels in the area of brain tissue, as well as to use local hemostatic agents, which retain their structure for a long time and often provoke the development of a local inflammatory process [1,4].The purpose of the study is to conduct a comparative analysis of methods of intraoperative hemostasis based on clinical data.
2. Material and Research Methods
- The study material included data from 184 patients with traumatic intracranial hemorrhage. The patients were hospitalized immediately after the injury or were admitted via air ambulance to the neurosurgery department of the Andijan branch of the Republican Scientific Center for Emergency Medical Care. The age of the study patients ranged from 18 to 85 years, according to the WHO age classification (WHO, 2017). The average age was 43.8±10.6 years. Among those studied 162 (88%) patients were men, 22 (12%) were women. The main group (96 patients) consisted of patients who, during surgery, underwent intraoperative hemostasis using Hemoben powder; patients in the comparison group (88 patients) received a collagen hemostatic sponge.
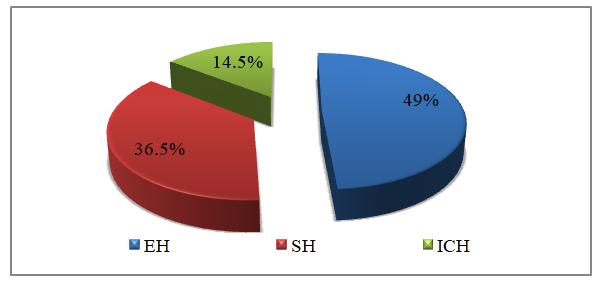 | Figure 1. Distribution of patients in the comparison group by type of intracranial hematoma |
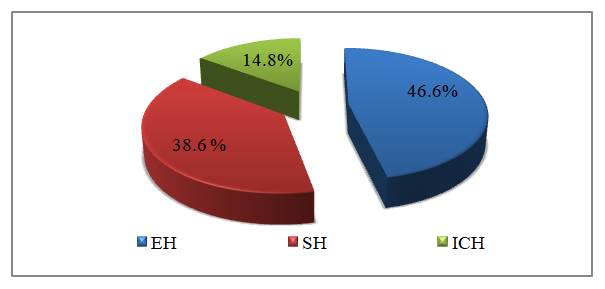 | Figure 2. Distribution of patients in the main group by type of intracranial hematoma |
3. Results and Its Discussion
- The intensity of bleeding was assessed using the Lewis KM et al. (2017), where 0 points – no bleeding, 1 point – diapedetic hemorrhage, 2 – extensive bleeding.After the main stage of the operation, in patients in the comparison group this indicator was 0 points (no bleeding) in only 8.3% of patients, in the main group 6.8%.
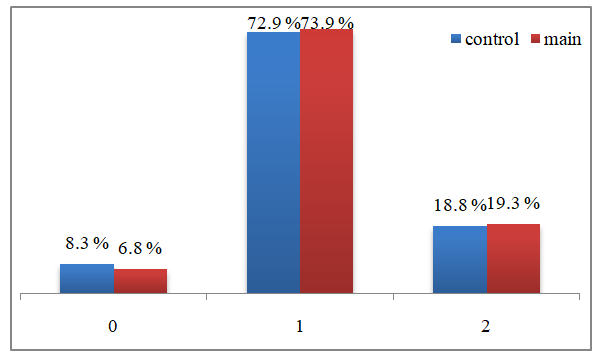 | Figure 3. Assessment of bleeding intensity according to the Lewis KM et scale al. (2017) after completing the main stage of the operation |
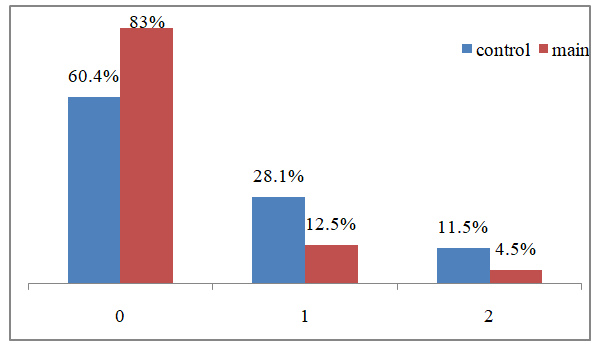 | Figure 4. Assessment of bleeding intensity after the first stage of local hemostasis |
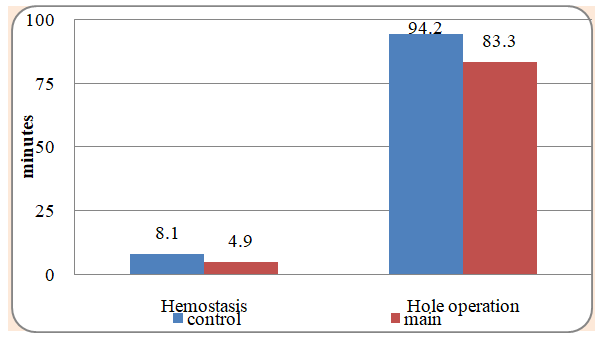 | Figure 5. Duration of the hemostasis stage and the entire operation (min: M±δ) |
4. Conclusions
- The use of the domestic drug Chemoben during operations on patients with traumatic intracranial hemorrhages, already at the first application according to the proposed method on the wound surface of brain tissue, made it possible to significantly reduce the intensity of parenchymal bleeding with an increase in the frequency of achieving one-stage absolute hemostasis (0 points on the Lewis KM et al.) from 60.4% to 83.0% (χ2 = 11.395; df =2; p=0.004).Also, the new method made it possible to reduce the number of hemostatic stages from 1.5±0.7 to 1.2±0.4 (t =3.74; p <0.05), reduce the need for the use of additional means for hemostasis (electrocoagulation, hemostatic sponge, temporary compression with a gauze pad with hot saline solution) from 39.6 to 17.0% (χ2 = 15.717; df = 3; p = 0.002), duration of the entire hemostasis stage from 8.1 ± 4.9 to 4.9±1.9 minutes (t =5.83; p <0.05) and reduce the volume of blood loss at the hemostasis stage from 70.2±16.6 to 54.4±15.1 ml (t =6, 77; p <0.05).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML