-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 4(2): 300-302
doi:10.5923/j.ajmms.20241402.29
Received: Jan. 15, 2024; Accepted: Feb. 6, 2024; Published: Feb. 8, 2024

The Role of Intraoperative Monitoring of Visual Evoked Potentials in Patients with Tumors of the Chiasma-Sellar Region
Akmaljon Mukhamedov1, Uygun Altybaev1, Gayrat Kariev2, Rano Ismailova3
1Department of Oncology, Republican Specialized Scientific Practical Medical Center for Neurosurgery, Tashkent, Uzbekistan
2Director of the Republican Specialized Scientific Practical Medical Center for Neurosurgery, Tashkent, Uzbekistan
3Department of Spinal Neurosurgery, Republican Specialized Scientific Practical Medical Center for Neurosurgery, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

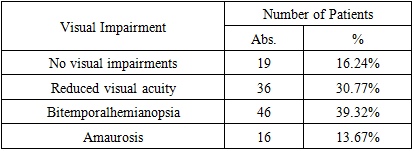
The microsurgical removal of tumors within the chiasm-sellar region is a crucial intervention to minimize recurrences and enhance the long-term quality of life for affected individuals. This study explores the efficacy of microsurgical procedures in conjunction with intraoperative monitoring of visual evoked potentials for assessing and preserving the functional integrity of the visual pathway structures during tumor removal. Methods: A retrospective analysis was conducted on 117 patients who underwent microsurgical interventions for chiasm-sellar region tumors at the Republican Scientific-Practical Medical Center of Neurosurgery from 2014 to 2021. Surgical procedures, primarily involving transcranial approaches, were performed with meticulous intraoperative monitoring of visual evoked potentials. Results: In the early postoperative period, an investigation into visual functions revealed notable outcomes. Among the 117 patients, 85 experienced an improvement in their visual functions, 25 patients maintained their preoperative levels, and 7 patients demonstrated a decline in vision. These findings underscore the positive impact of the surgical interventions on visual outcomes for the majority of patients. Conclusion: Microsurgical removal, coupled with intraoperative monitoring of visual evoked potentials, emerged as a promising strategy for achieving favorable long-term outcomes. This approach not only contributed to reduced recurrences but also facilitated a stable improvement in the quality of life for patients. The use of intraoperative monitoring was deemed objective and highly informative, preventing and minimizing visual complications associated with surgical interventions.
Keywords: Pituitary gland adenoma, Meningioma, Craniopharyngioma, Chiasm glioma, Tumors of the chiasma-sellar region, Intraoperative monitoring
Cite this paper: Akmaljon Mukhamedov, Uygun Altybaev, Gayrat Kariev, Rano Ismailova, The Role of Intraoperative Monitoring of Visual Evoked Potentials in Patients with Tumors of the Chiasma-Sellar Region, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 300-302. doi: 10.5923/j.ajmms.20241402.29.
1. Introduction
- The prompt diagnosis and treatment of tumors within the chiasmatic-sellar region of the brain represent a contemporary challenge in the fields of neurosurgery and neurology. Neoplasms in the chiasmal-sellar region (CS) are notable among intracranial tumors, constituting 15-18% of cases [1] [3] [4]. Predominantly, benign tumors of the pituitary gland are the most frequent within the sellaturcica region [1] [2], with the majority measuring less than 10-15 mm and remaining confined to the sellaturcica [5]. In these instances, clinical manifestations primarily result from the hormonal activity of the tumor.However, when tumors exceed these dimensions, clinical symptoms emerge due to the compression of adjacent structures [6]. These symptoms include headaches, impaired visual function, reduced secretion of tropic hormones from the adenohypophysis, and hyperprolactinemia. Deciding on the appropriate treatment approach requires assessing the tumor's hormonal activity and topographic and anatomical characteristics [7].The clinical nuances of CS region tumors, the selection of surgical strategies, and the prognosis of the disease hinge on factors such as tumor localization, size, growth characteristics, histological nature, and the degree of associated hydrocephalus. A thorough analysis of comprehensive examination results, encompassing CT and MRI scans, in conjunction with clinical data, is crucial for determining the optimal treatment plan and achieving enduring positive outcomes.Employing visual function monitoring during tumor removal allows for the timely identification of excessive irritation to the visual pathway, enabling the implementation of appropriate measures [8]. Consequently, this approach contributes to vision preservation and preventing irreversible damage to the visual system.The paramount objective of our research is to investigate the role of intraoperative monitoring of visual evoked potentials in patients with tumors located in the chiasm-sellar region. Understanding the impact of this monitoring technique in the context of chiasm-sellar tumors is crucial for advancing our knowledge in neurosurgery and optimizing patient care. This study aims to contribute valuable insights into the significance of visual evoked potential monitoring during surgical interventions in this patient population.
2. Materials and Methods
- A total of 117 patients with tumors in the chiasm-sellar region (CSR) were admitted for inpatient treatment at the Republican Scientific-Practical Medical Center of Neurosurgery from 2014 to 2021. Surgical interventions were performed on all patients utilizing transcranial approaches, with intraoperative monitoring of visual evoked potentials.Comprehensive preoperative and postoperative neurological examinations, cranial radiography, computed tomography (CT), magnetic resonance imaging (MRI), echoencephaloscopy, electroencephalography, visual evoked potentials, and other neurophysiological assessments were conducted for all patients. Diagnostic procedures were carried out in accordance with established standards for brain tumor evaluation.The Karnofsky Performance Status scale assessed the neuro-oncological patients' overall condition, evaluated upon admission and discharge. Neurological status was assessed upon admission, in the early postoperative period, and at discharge. In addition to the Karnofsky scale assessment, the level of consciousness was evaluated using the classic classification of consciousness disorders. The severity of global and focal neurological symptoms was also assessed.Histological analysis of the tumor was performed for all patients who underwent radical surgery to determine the nature of the neoplasm. This comprehensive approach aimed to provide a thorough understanding of the patient's neurological and oncological status before, during, and after surgical interventions, enhancing the overall outcomes assessment.
3. Results and Discussion
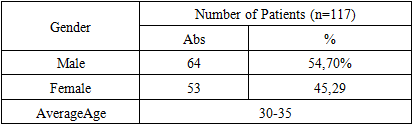
- The study included a diverse age range of patients, spanning from 6 to 60 years, with an average age of 30-35 years. The male-to-female ratio was 1.2:1, and there was no statistically significant correlation between age and gender (Table 1).
|
|
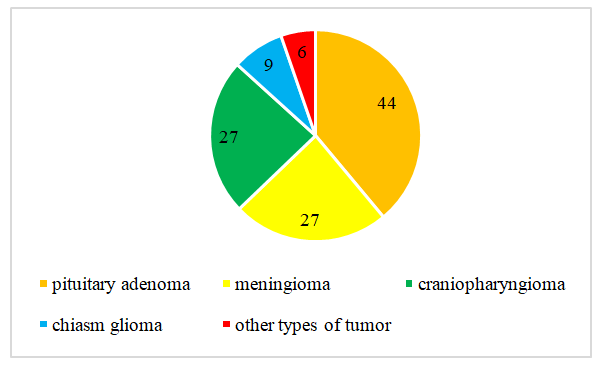 | Figure 1. Distribution of Tumor Types |
4. Conclusions
- Microsurgical removal of tumors in the chiasm-sellar region results in fewer recurrences and contributes to a sustained improvement in the quality of life for patients in the long term.Intraoperative monitoring of visual evoked potentials is considered an objective and highly informative method for assessing the functional status of the visual pathway structures during removing tumors in the chiasm-sellar region.The intraoperative monitoring of visual evoked potentials prevents and reduces the incidence of visual complications during surgical interventions. This technique proves instrumental in preserving visual function and minimizing adverse outcomes associated with the surgical removal of tumors in the chiasm-sellar region.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML