Karshiev Ziyadulla Khazratovich1, Ibadullaev Bekzod Bakhramovich2
1Samarkand State Medical University, Samarkand, Uzbekistan
2Urgench Branch of Tashkent Medical Academy, Urgench, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article discusses the study of the structure of adaptation disorders using effective psycho-diagnostic methods in the diagnosis of adaptation disorders in patients with bronchial asthma and the use of effective medical and psychological methods in therapeutic processes and treatment effectiveness.
Keywords:
Adaption, Anxiety, Bronchial asthma, Frustration, Psychotherapy
Cite this paper: Karshiev Ziyadulla Khazratovich, Ibadullaev Bekzod Bakhramovich, Characteristics of the Structure of Adaptation Disorders in Patients with Bronchial Asthma and Its Psychocorrection, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 272-277. doi: 10.5923/j.ajmms.20241402.23.
1. Introduction
Today, the number of chronic diseases in our region is increasing, one of them is bronchial asthma. According to WHO data, in 2018, about 4-10% of the world's population, i.e. 235 million people, and in 2021, this number will be 360 million people, is confirmed to suffer from bronchial asthma. Research conducted in our country today shows that the incidence of this disease among children and adults is increasing from year to year, especially among children compared to adults it is found to be 1.3-1.5 times higher. Patients with developed bronchial asthma suffer not only from somatic complaints, but also from medical and psychological problems. Because 12-25% of patients suffering from somatic diseases found in general practical medicine have masked depression [1,2,6]. The development of psycho-emotional disorders leads to an increase in somatic and vegetative clinical symptoms in patients, which in turn serves as one of the main factors affecting the quality of life of patients and the course of the disease. In addition, most patients with somatic diseases suffer from anxiety, anxiety-phobic, anxiety-stress and maladaptive disorders in addition to depression, which in turn affects the dynamics of therapeutic processes. requires the organization of both medical and psychological support [3,4,5]. Taking into account the relevance of the topic, this work is aimed at identifying and correcting adaptive disorders in patients with developed bronchial asthma.
2. Objective
To use psycho-diagnostic methods and effective medical and psychological correction in the screening of adaptation disorders in patients with bronchial asthmatreated in the department of allergology and pulmonology of the Samarkand city medical hospital.
3. Materials and Methods
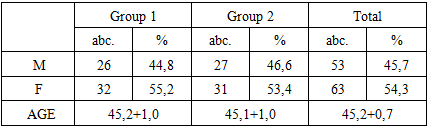
It was conducted in 116 patients with asthma in the department of allergology and pulmonology at the Samarkand city medical hospital. Of these, 53 were men and 63 were women. The patient group consisted of individuals aged 30–65 years, with an average age of 45.2±0,7. The somatic condition of our patients is studied on the basis of complaints, anamnesis, objective and subjective, paraclinical data when they come to the clinic for treatment. A special medical-psychological questionnaire was used to assess the mental status of our patients. In assessing the degree of adaptive disorders in patients, the following psychometric tests were used in our study:● Statistical analysis of pre- and post-treatment parameters was performed using the Eysenck (assessment of patients ’own mental state) questionnaire. In our study, psycho-correction of psycho-adaptation disorders was performed by dividing patients into two groups:Group 1: A psychotherapeutic algorithm based on basic treatment and cognitive-behavioral psychotherapy was applied to patients in this group: n - 58.Group 2: Basic treatment and rational psychotherapy were used in patients in this group: n - 58.Rational psychotherapy and cognitive-behavioral psychotherapy were selected from the psychotherapeutic methods performed on patient the distribution of our patients was as follows: (Table 1).Table 1
 |
| |
|
According to the table, 26 (44.8%) of our patients in group 1 were men, 32 (55.2%) were women, their average age was 45,2+1,0, 2 - 27 (44.6%) patients in the group were men, 31 (53.4%) were women, their average age was 45,1+1,0.
4. Results
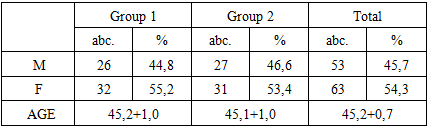
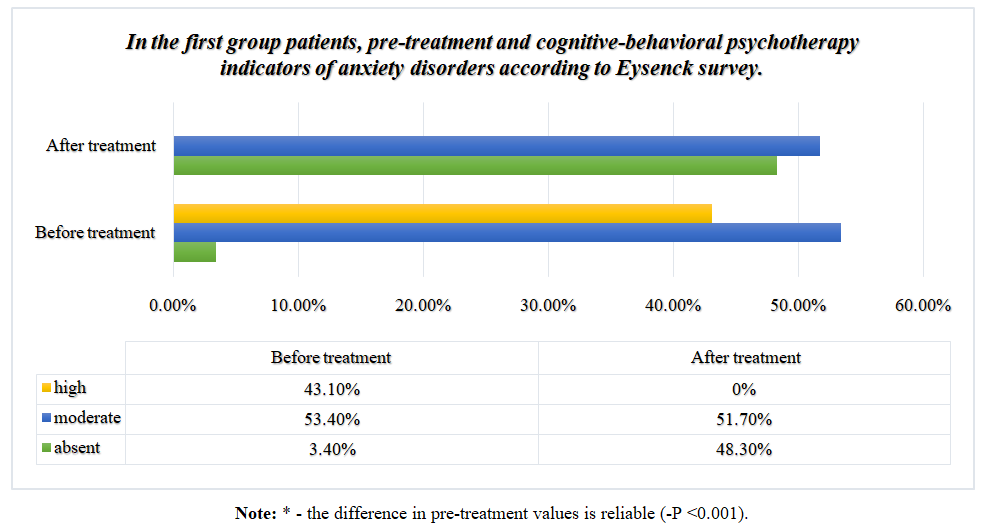
The following results were obtained using the Eysenck survey to identify advanced adaptive disorders in our patients. According to the survey, the structure of adaptive disorders developed in our patients was formed on the basis of 4 small scales of the questionnaire, namely, anxiety, aggression, frustration and rigidity, and pre-treatment and post-treatment indicators were statistically analyzed on the basis of diagrams and tables. According to the analysis, the pre-treatment and post-treatment indicators on the anxiety scale of the Eysenck survey of our patients in group 1 were as follows (Diagram 1).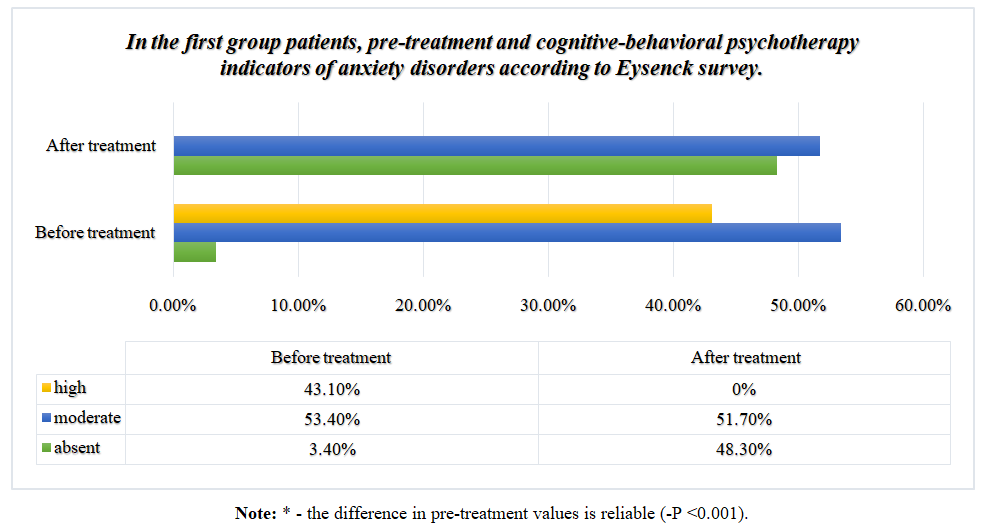 | Diagram 1 |
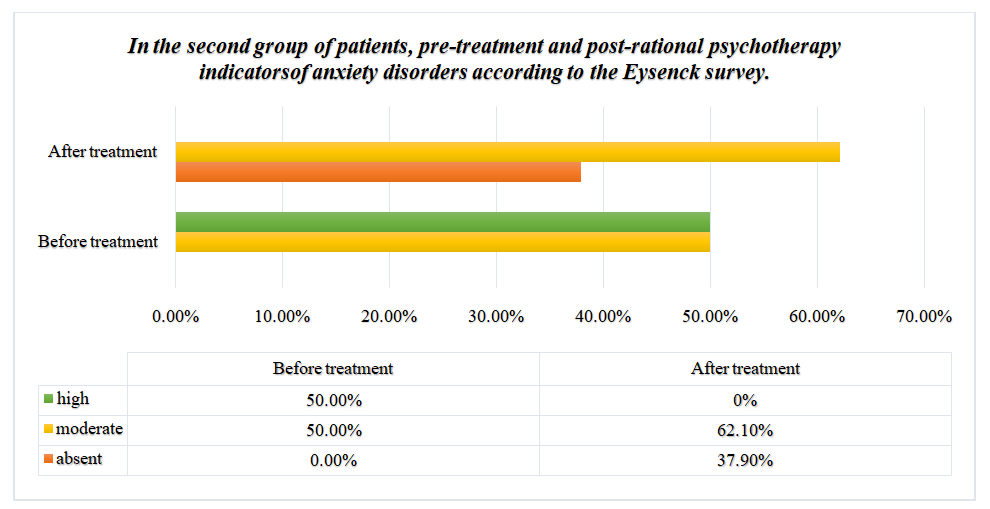
Analysis of the results showed that in 3.4% (n = 2) of our patients before the treatment there was no anxiety or mild (7.0 + 0.0), 53.4% (n = 31) (12.8 + 0.21) moderate, 43.2% (n = 25) severe (17.8 + 0.25) anxiety disorders were detected. This figure is higher in 48.3% (n=28) of patients after cognitive-behavioral psychotherapy (CBP), when anxiety disorders were not detected at all or were mild (6.4 + 0.12), 51,7% (n= 0.26) anxiety disturbances (-P<0.001). In our group 2 patients, the following results were obtained during the comparative analysis of pre-treatment and post-treatment indicators (Diagram 2). | Diagram 2 |
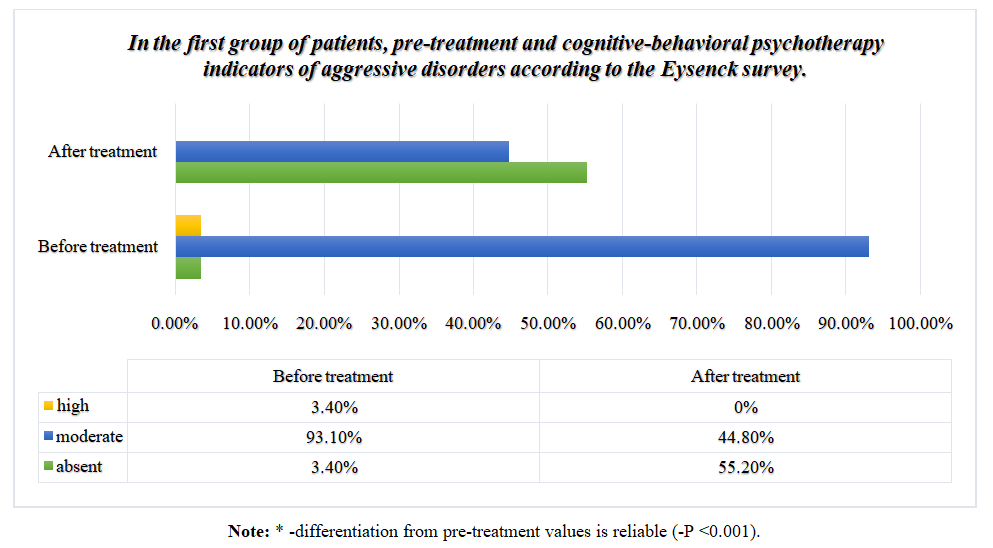
Analysis of the results showed, which obtained in the second group of patients that before treatment in 50% (n=28) was moderate (12.6+0.21), in 50% (n=28) was high (17.6+0.18) anxiety diturbances were detected. This figure was significantly higher in 37.9% (n = 22) of patients with anxiety disorders who were not detected at all or had a mild appearance (6.5 + 0.18) after 62 days of rational psychotherapy (RP). % (n = 36) reported moderate (9.4 + 0.22) disturbances (-p <0.001). Analyzing the indicators identified on the anxiety scale of the above Eysenck questionnaire, we can say that in patients with mild and moderate anxiety disorders after psychotherapy in both groups of symptoms associated with mild or anxiety disorders.In our patients with high levels of anxiety disorders, we can see that these indicators decreased to moderate and mild (-p <0.001).The following results were obtained when analyzing the second scale of the Eysenck questionnaire, i.e., pre-treatment aggression in patients, compared with post-treatment indicators. Analysis of the results obtained from our patients in group 1 (diagram 3).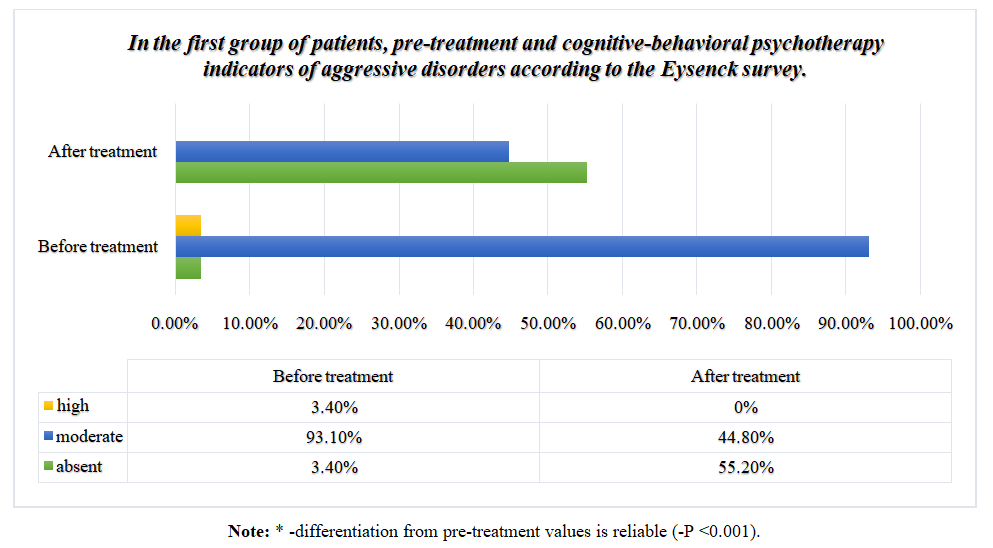 | Diagram 3 |
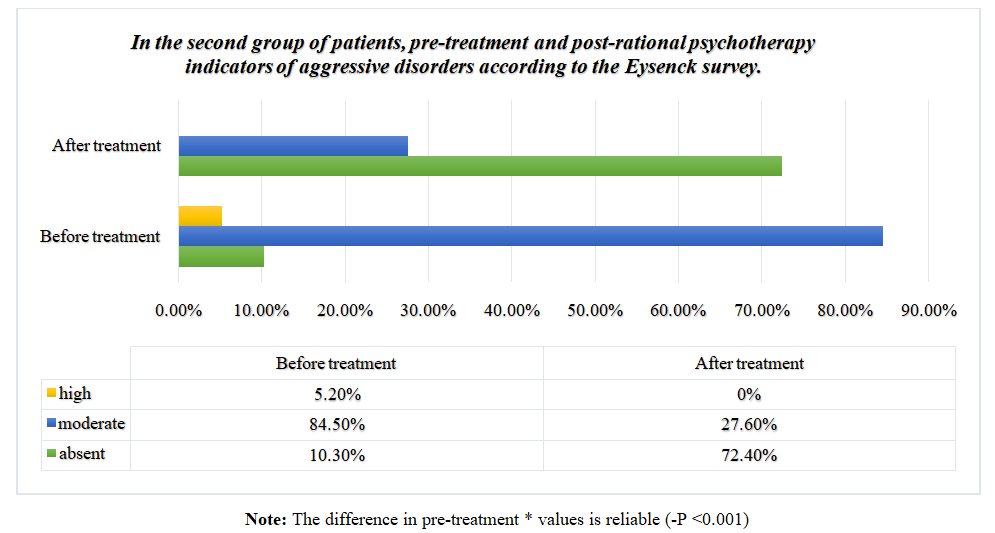
Analysis of the results obtained in group 1 showed that 3.4% (n = 2) of our patients had no aggressive disorders before treatment or were mild (7.0 + 0.0), 93.4% (n = 54) (12.0 + 0.18) moderately severe, 3.4% (n = 2) severe (18.0 + 0.0) aggressive disorders were detected.This indicator is similar to that in 55.2% (n = 32) of patients after cognitive-behavioral psychotherapy (CBP), aggressive disorders were not detected at all or were mild (6.3 + 0.09). , 44.8% (n = 26) reported moderate (8.7 + 0.16) aggressive disturbances (-P <0.001).In our second group, the following results were obtained when analyzing these indicators (Diagram 4).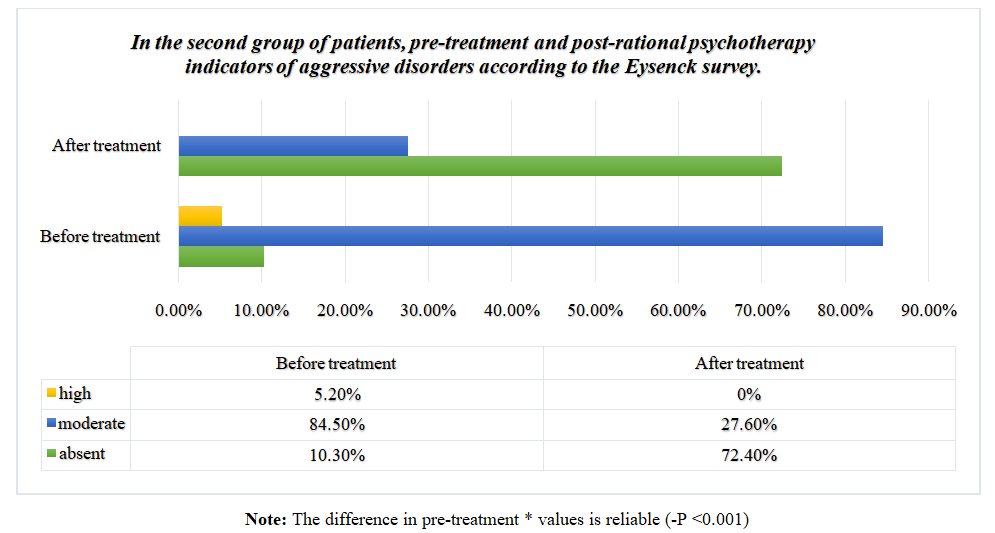 | Diagram 4 |
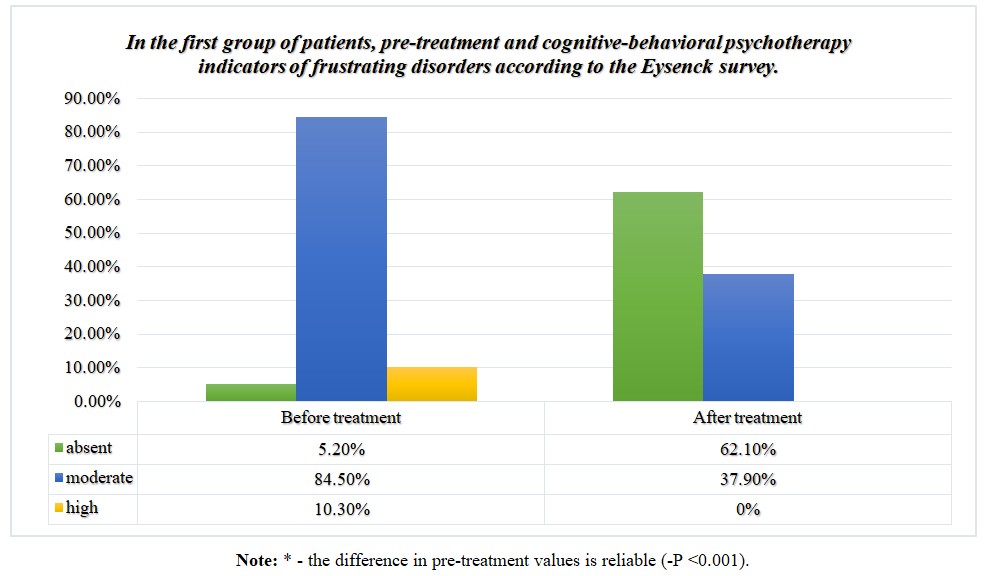
Analysis of the results obtained in group 2 showed that 10.3% (n = 6) of our patients had no aggressive disorders before treatment or were mild (7.0 + 0.0), 84.5% (n = 49). moderate (11.7 + 0.23), high-level (17.0 + 0.58) aggressive disorders were detected in 5.2% (n = 3). This figure was higher in 72.4% of patients (n = 42) after rational psychotherapy (RP) who had no or no aggressive symptoms at all (6.2 + 0.10), 27, 6% (n = 16) reported moderate (8.7 + 0.12) aggressive disturbances (-P <0.001). Analyzing the indicators of the Eysenck survey on the scale of aggression, we can say that the regression of symptoms associated with mild and aggressive disorders was observed in both groups after psychotherapy in patients with mild and moderate aggressive disorders identified in our patients. In our patients with high levels of aggressive disorders, we can see that these indicators decreased to moderate and mild (-p <0.001).The following results were obtained when the third scale of the Eysenck questionnaire, i.e., pre-treatment frustration indicators in patients, was compared with post-treatment indicators. Analysis of the results obtained from our patients in group 1 (diagram 5).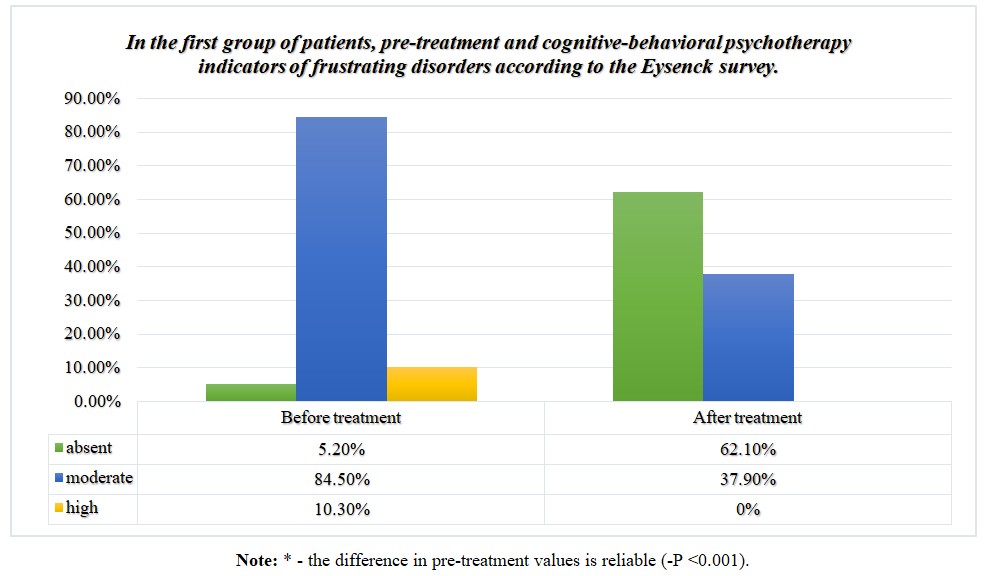 | Diagram 5 |
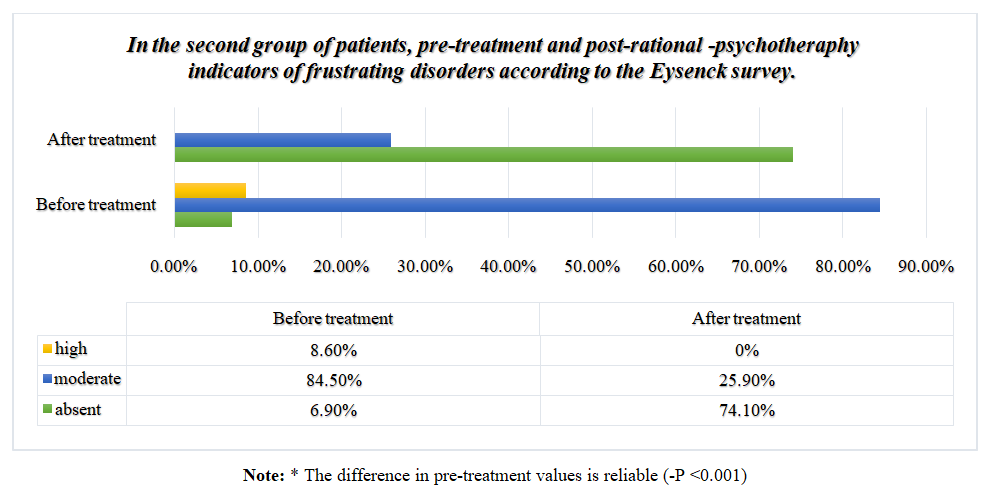
Analysis of the results obtained in group 1 showed that in 5.2% (n = 3) of patients before treatment there were no disorders of frustration or mild (7.0 + 0.0), 84.5% (n = 49) had moderate (12.6 + 0.16) and 10.3% (n = 6) had severe (18.3 + 0.21) frustration disorders. These indicators showed that frustration disorders were not detected at all or were mild in 62.1% (n = 36) of patients after cognitive-behavioral psychotherapy (CBP) (6.4 + 0.10). , 37.9% (n = 22) reported moderate (8.4 + 1.0) frustration disorders. (-P <0.001).Analysis of these indicators in patients of group 2 gave the following results (diagram 6).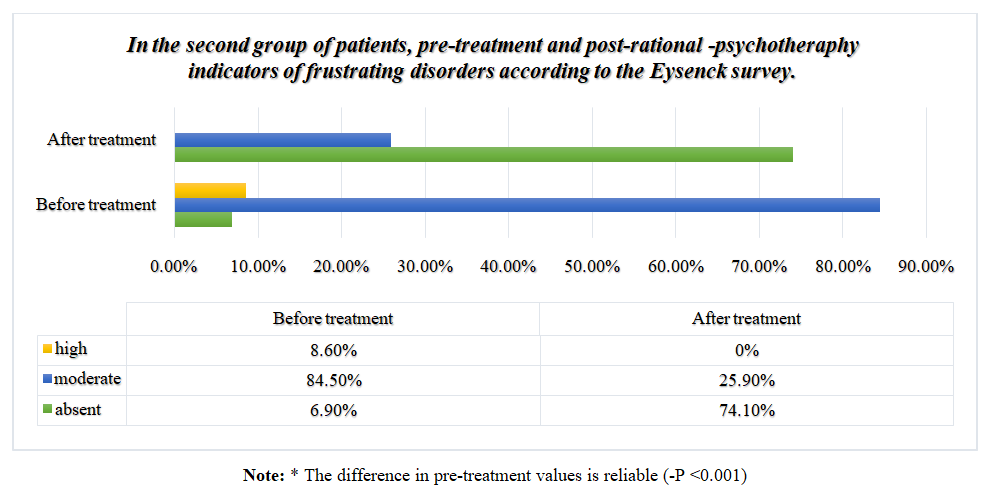 | Diagram 6 |
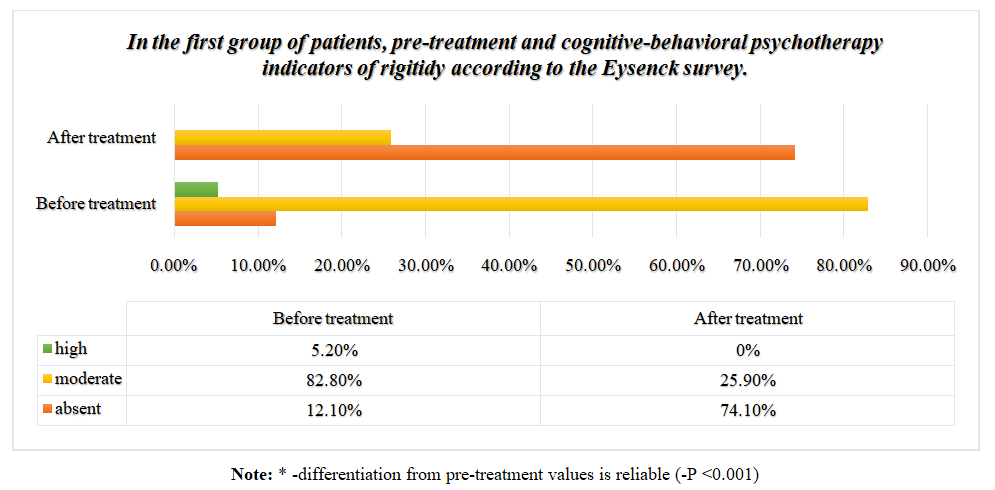
Analysis of the results obtained in group 2 showed that 6.9% (n = 4) of our patients had no frustration disorders before treatment or were mild (7.0 + 0.0), 84.5% (n = 49). moderate (12.4 + 0.22), 8.6% (n = 5) and high (17.0 + 0.58) frustration disorders were detected. These indicators showed that in 74.1% (n = 43) of patients after rational psychotherapy (RP), frustration disorders were not detected at all or were mild (6.4 + 0.12), 25, 9% (n = 15) reported moderate (8.7 + 0.18) frustration disorders (-P <0.001). Analyzing the indicators identified on the frustration scale of the Eysenck survey above, we can say that regression of symptoms associated with mild frustrating disorders was observed in both groups after psychotherapy in patients with mild to moderate frustration disorders identified in our patients. And in our patients with high levels of frustration disorders, we may see a decrease in these rates to moderate to mild (-p <0.001).The next scale of the Eysenck questionnaire, i.e., pre-treatment rigidity levels in patients, was analyzed in comparison with post-treatment indicators, and the following results were obtained. Analysis of the results obtained from our patients in group 1 (diagram 7).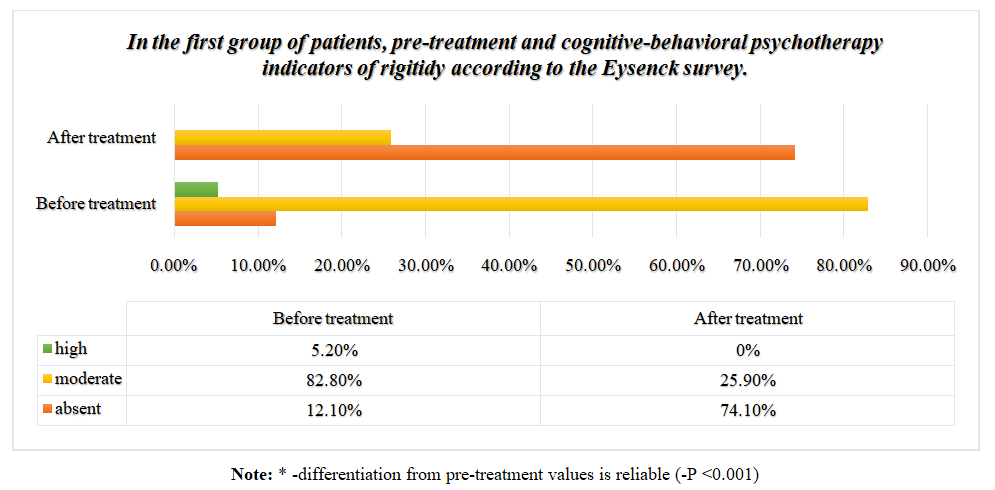 | Diagram 7 |
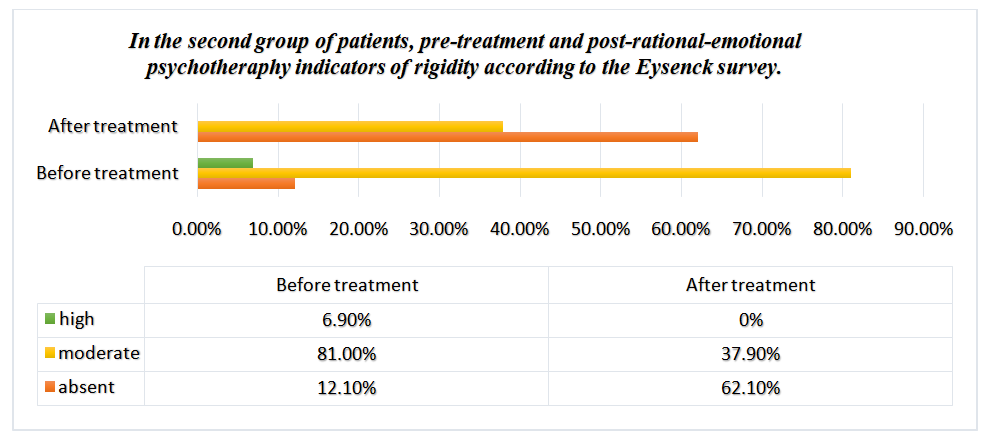
Analysis of the results obtained in group 1 showed that 12.1% (n = 7) of our patients did not have rigidity disorders before treatment or were mild (7.0 + 0.0), 82.8% (n = 48) in moderate (12.7 + 0.21), 5.2% (n = 3) in severe (18.0 + 1.5). These indicators showed that after cognitive-behavioral psychotherapy (CBP), 74.1% of patients (n = 43) had rigidity disorder. These indicators showed that in 74.1% (n = 43) of patients after cognitive-behavioral psychotherapy (CBP), frustration disorders were not detected at all or were mild (6.4 + 0.12), 25,9% (n = 15) reported moderate (8.7 + 0.18) frustration disorders (-P <0.001). In group 2 patients, the analysis of these indicators allowed to obtain the following results (Diagram 8).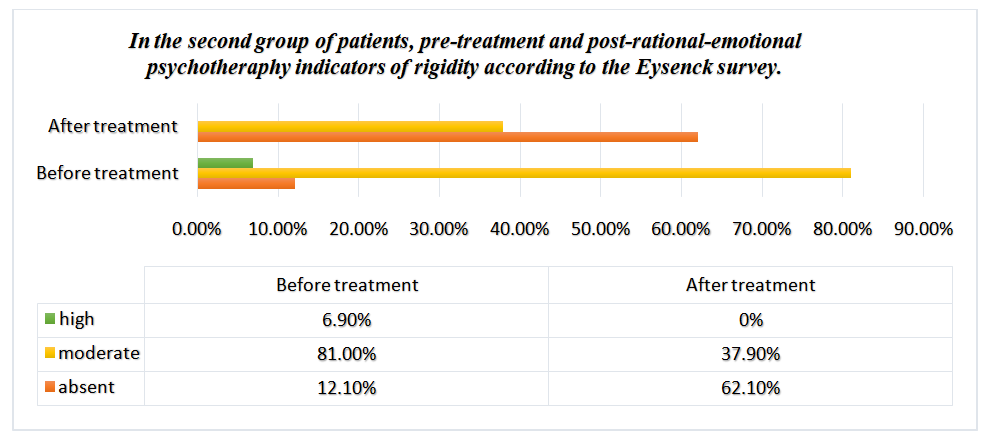 | Diagram 8 |
Analysis of the results obtained in group 2 showed that 12.1% (n = 7) of our patients had no rigidity before treatment or mild (7.0 + 0.0), moderate in 81.0% (n = 47) (12.3 + 0.24), 6.9% (n = 4) and high (8.9 + 0.19) stiffness were detected. These indicators showed that after rational psychotherapy (RP), 62.1% (n = 36) of patients had no rigidity that was not detected at all or was mild (6.4 + 0.12), 37. Medium (8.9 + 0.19) stiffness was observed in 9% (n = 22) (P <0.001). Analyzing the indicators of the rigidity scale of the Eysenck survey above, we can say that the regression of mild or rigidity-related psychological disorders was observed in both groups after psychotherapy in patients with mild to moderate rigidity identified in our patients. In our patients with high levels of rigidity, we can see that these values decreased to moderate and mild (-p <0.001).
5. Conclusions
From the above results, it can be concluded that timely psychodiagnostics of adaptive disorders in patients with plays a significant role in the analysis of the psychological status of each patient, as well as in assessing the effectiveness of psychotherapy. Secondly, during the medical and psychological care of our patients, it was found that the method of psychotherapy used in the correction of adaptive disorders in the first group of patients, the method of cognitive-behavioral psychotherapy (CBP), was more effective than rational psychotherapy in the second group. our observations have shown that choice in correction is a method of psychotherapy and at the same time plays an important role in improving the quality of life of patients.
References
| [1] | Bogovin L.V., Perelman J.M., Kolosov V.P. Psikhologicheskie osobennosti bol'nykh bronkhial'noy astmoy [Psychological features of the patients with bronchial asthma]. Vladivostok: Dal'nauka; 2013. |
| [2] | Borisova E.O. Atmosfera. Pul'monologiya i allergologiya 2004; 3:14–18. |
| [3] | Ibodullaev B. B. Structure and correction of psychoemothical disorders in patients with second type of diabetes // Asian Journal of Multidimensional Research. – 2021. – Т. 10. – №. 9. – С. 227-230. |
| [4] | Ибадуллаев Б. Б. Қандли диабетнинг иккинчи типи билан касалланган беморларда психоэмоционал бузилишларни коррекция қилишда психотерапиянинг роли // Журнал неврологии и нейрохирургических исследований. – 2022. – Т. 3. – №. 6. |
| [5] | Ибодуллаев Б. Б. Қандли диабет иккинчи типи билан касалланган беморларда ривожланган ҳавотирли бузилишлар психокоррекцияси // Academic research in educational sciences. – 2021. – Т. 2. – №. 6. – С. 1107-1112. |
| [6] | Smulevich A.B. Depressii pri somaticheskikh i psikhicheskikh zabolevaniyakh [Depression at somatic and psychic diseases]. Moscow: MIA; 2003. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML