-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 4(2): 268-271
doi:10.5923/j.ajmms.20241402.22
Received: Jan. 9, 2024; Accepted: Feb. 2, 2024; Published: Feb. 8, 2024

The Influence of Intraocular Lens Implantation with a Yellow Filter on the Quality of Life in Patients with Age-Related Macular Degeneration in the Long Term
A. F. Yusupov1, M. X. Karimova1, R. A. Abdusamatova2
1Doctor of Medical Sciences, Professor, Republican Specialized Scientific Practical Medical Center of Microsurgery of the Eye, Uzbekistan
2PhD Post-Graduate Course Student, Republican Specialized Scientific Practical Medical Center of Microsurgery of the Eye, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

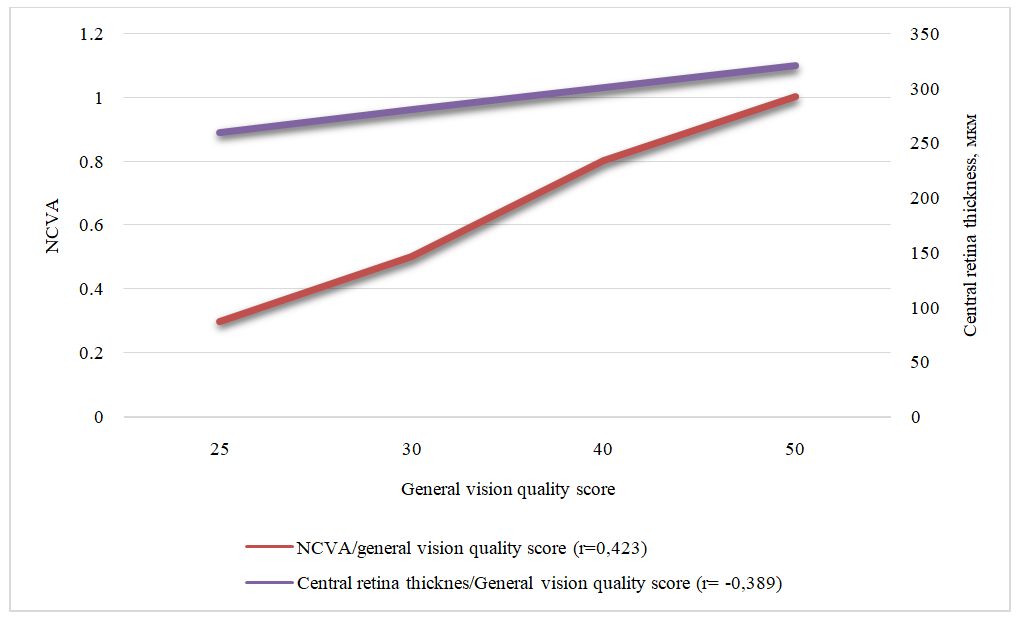
Objective. To assess the quality of life in patients after the implantation of intraocular lenses with a yellow filter for age-related macular degeneration (AMD) using the adapted NEI-VFQ-25 questionnaire. Methods. The study included 68 patients (80 eyes) with confirmed diagnosis of dry form AMD, who underwent cataract surgery using phacoemulsification with intraocular lens (IOL) implantation following standard procedures during the period 2016-2018. A Russian-language validated version of the National Eye Institute Visual Function Questionnaire (NEI VFQ-25) was employed to evaluate patients' quality of life. Results. The average scores of patients in the main group, who received IOLs with a yellow filter, surpassed those of the comparative group. The study results indicated a direct correlation between the quality of life score and uncorrected visual acuity, as well as an inverse correlation with retinal thickness in the central zone. Conclusion. The assessment of long-term outcomes of intraocular lens implantation with a yellow filter in patients with age-related macular degeneration, using the adapted NEI-VFQ-25 questionnaire, demonstrated higher scores reflecting better quality of life in terms of visual function.
Keywords: Cataract, Age-related macular degeneration, Intraocular lenses with yellow filter, Quality of life
Cite this paper: A. F. Yusupov, M. X. Karimova, R. A. Abdusamatova, The Influence of Intraocular Lens Implantation with a Yellow Filter on the Quality of Life in Patients with Age-Related Macular Degeneration in the Long Term, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 268-271. doi: 10.5923/j.ajmms.20241402.22.
Article Outline
1. Introduction
- Age-related macular degeneration (AMD) and cataracts are common eye conditions among elderly patients worldwide. Cataracts are most frequently observed in individuals over 60 years old. According to the World Health Organization, AMD ranks third, after cataracts and glaucoma, among diseases leading to blindness. While cataract surgery effectively treats vision impairment due to lens opacification, several authors [1,2,3] suggest that cataract surgery is a risk factor for the progression of AMD. Simultaneously, cataract surgery in the presence of concomitant AMD may worsen its course, especially without adequate treatment [2,4].Following cataract surgery, patients with pre-existing or progressing AMD do not experience the expected improvement in visual acuity, leading to a decrease in their quality of life and additional healthcare costs. Some scientists, relying mainly on large epidemiological studies demonstrating an adverse association between cataract surgery and AMD, have raised concerns about the risk of surgical intervention for cataracts in eyes with advanced forms of AMD. Others have advocated for stricter indications for cataract removal in patients with AMD [5,6].Currently, various models of intraocular lenses (IOLs) exist for implantation in patients with AMD. IOLs with a yellow filter block blue spectrum rays without disrupting color perception, similar to the protective filter of the natural human lens possessed by next-generation lenses [2,6,7]. With such IOLs, theoretically, it may be possible to slow down the progression of AMD, protecting the retina from the negative impact of blue light. However, the effectiveness of this approach is not fully understood, making the assessment of various aspects of AMD in patients who have undergone cataract surgery with yellow-filter IOL implantation a pertinent research task.
2. Research Objective
- To assess the quality of life of patients after the implantation of intraocular lenses with a yellow filter in age-related macular degeneration using the adapted NEI-VFQ-25 questionnaire.
3. Materials and Methods
- The study was conducted at the Republican Specialized Scientific Practical Medical Center of Microsurgery of the Eye. The research included 68 patients (80 eyes) with confirmed diagnosis of dry form age-related macular degeneration (AMD), categorized as 2, 3, and 4 according to the Age-Related Eye Disease Study (AREDS) classification. These patients underwent cataract surgery using phacoemulsification with intraocular lens (IOL) implantation following standard procedures from 2016 to 2018. The study involved questionnaire-based surveys. The average age of participants was 69.5±5.2 years.Patients were divided into two homogeneous groups based on gender and age. The main group comprised 32 patients (36 eyes) who received IOLs with a yellow filter (Aurolab, EV Gold), while the comparative group included 36 patients (44 eyes) who received colorless hydrophobic acrylic IOLs (Aurolab, Aurovue EV).All patients underwent standard ophthalmological examinations, including visual acuity testing, biomicroscopy, tonometry, autorefractometry, as well as additional investigations such as optical coherence tomography (OCT).To assess patients' quality of life, a Russian-language validated version of the National Eye Institute Visual Function Questionnaire (NEI VFQ-25) was utilized. Comprising 25 questions, this adapted questionnaire is a validated version of the Visual Function Questionnaire, the reliability of which has been confirmed by numerous studies [1,2,8]. The VFQ-25 questionnaire, after scaling, forms 12 scales: General Health, General Vision, Ocular Pain, Near Activities, Distance Activities, Social Functioning, Mental Health, Role Difficulties, Dependency, Driving, Color Vision, and Peripheral Vision. Additionally, composite scores for each scale were calculated, resulting in the VFQ-25 Composite score. The numerical scores in each scale range from 0 to 100, reflecting the percentage of the maximum possible result.Standard functions of Microsoft Excel 2019 were used for statistical analysis. Quantitative data were presented as mean ± standard error (M±m). Student's t-test was employed to determine the statistical significance of differences in mean values between groups and within groups before and after treatment (p<0.05). Correlation analysis was also conducted, calculating the correlation coefficient (r) using standard methods.
4. Results and Discussion
- The results of assessing various components of the quality of life in patients with age-related macular degeneration (AMD) after the implantation of different intraocular lens (IOL) models are presented in Figure 1. From the graph, it is evident that the average scores of patients in the main group, who received IOLs with a yellow filter, surpassed those of the comparative group. Statistical significance at p<0.05 was determined only for the indicators of overall vision quality and near vision function.
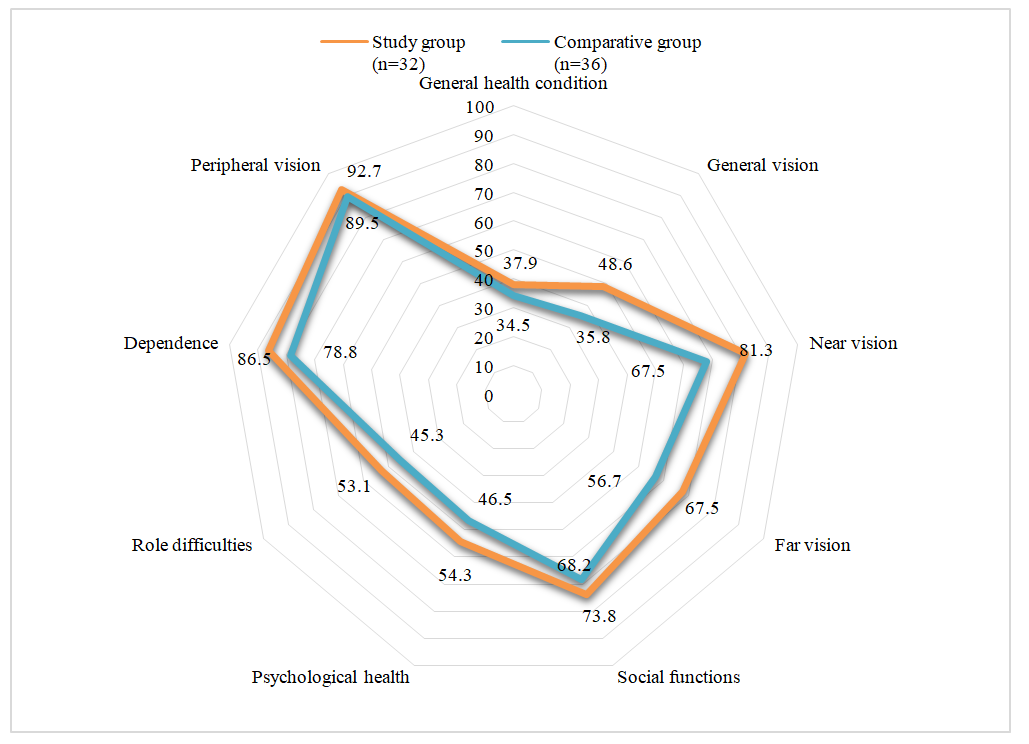 | Figure 1. Comparative analysis of components of visual perception in quality of life based on NEI VFQ-25 results |
5. Conclusions
- The assessment of long-term outcomes of intraocular lens implantation with a yellow filter in patients with age-related macular degeneration, using the adapted NEI-VFQ-25 questionnaire, demonstrated higher scores reflecting better quality of life in terms of visual function.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML