Mamurov Olimjon Islomovich
Independent Researcher, Center for the Development of Professional Qualification of Medical Workers, Uzbekistan
Correspondence to: Mamurov Olimjon Islomovich, Independent Researcher, Center for the Development of Professional Qualification of Medical Workers, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Along with this, the heart rate is one of the leading factors in the pathogenesis of coronary heart disease. The disease is one of the main determinants of myocardial oxygen consumption and is closely related to the duration of diastole. Data from numerous authors claim that with a decrease in the severity of tachycardia, myocardial perfusion improves duye to elongation of the diastole of the left ventricle.
Keywords:
Heart rate, Coronary heart disease, Myocardium, Oxygen, Pathogenesis, Disease, Tachycardia, Perfusion
Cite this paper: Mamurov Olimjon Islomovich, Hemodynamic Parameters in the Examined Women with Breast Cancer with and Without Coronary Heart Disease, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 263-267. doi: 10.5923/j.ajmms.20241402.21.
1. Introduction
The negative effect of high heart rate on coronary heart disease has long beyen proven. High heart rate figures can lead to a mismatch between the increased oxygen demand of the myocardium, as well as the ability to adequately increase coronary blood flow.Along with this, the heart rate is one of the leading factors in the pathogenesis of coronary heart disease. The disease is one of the main determinants of myocardial oxygen consumption and is closely related to the duration of diastole. The data of numerous authors claim that with a decrease in the severity of tachycardia, myocardial perfusion improves due to the elongation of the diastole of the left ventricle.In the patients we examined, before chemotherapy with doxorubicin at a dose of 550 mg/m2 in the main group, the heart rate was 79 yo 12 beats per minute, and after chemotherapy 80 yo 7.3 beats per minute. We did not find any negative dynamics in the heart rate, however, this indicator is very high for patients with a history of coronary heart disease. The study revealed that in patients with coronary heart disease with left ventricular dysfunction, having a heart rate of more than 70 beats per minute, the risk of cardiovascular mortality increases by 34%, myocardial infarction by 46%, heart failure by 53% and the need for cardiac revascularization by 38%.A high heart rate indicates that, in patients with coronary heart disease and breast cancer, the work of the heart increases and, naturally, the need for oxygen in the myocardium. Along with this, the diastole time decreases, and this leads to a deterioration in the perfusion of the heart muscle, which in turn contributes to an increase in pain in the heart area. This fact has been confirmed in our clinical studies.
2. Materials and Methods
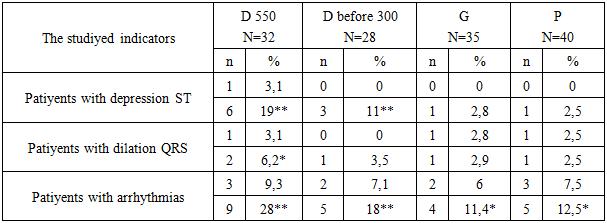
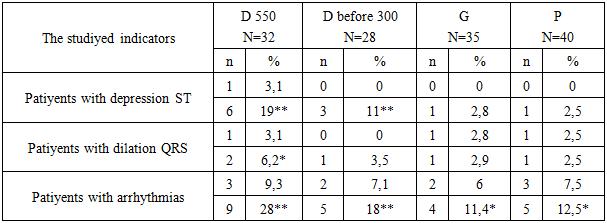
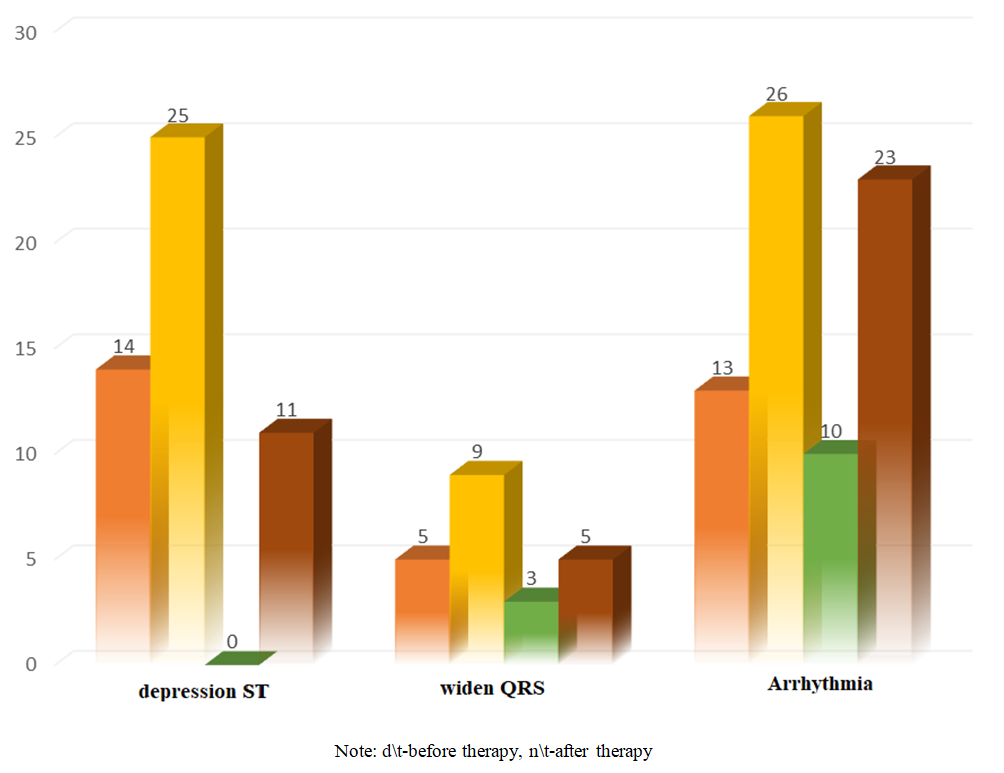
In the next step, we analyzed the prevalence of cardiac arrhythmia among women with breast cancer and coronary heart disease before and after therapy. Arrhythmias were detected in 13 (13.4%) women before therapy, and after therapy (a month later) in 26 (27%), that is, the incidence of cardiac arrhythmias increased by 50%. There is also a high percentage of arrhythmia in women with doxorubicin. Doxorubicin at a dose of 550 mg/m2 by 30% (n=10) (p>0.001) contributed to an increase in cardiac arrhythmia relative to the baseline data and amounted to 40%, before therapy the indicator was equal to 12% (n=3).Table 1. ECG electrocardiogram picture in women with breast cancer and without coronary heart disease during initial examination and on the background of therapy
 |
| |
|
A similar ECG electrocardiogram pattern is detected at a dose of 300 mg/m2 of this drug, which is also characterized by an increase in the number of patients with cardiac arrhythmias by 57% (n=7) (p> 0.001) relative to the baseline data (n=4). But patients with Herceptin also did not lag behind, in this group of patients, heart arrhythmias were detected in 3 (12.5%) before therapy, and after therapy in 5, which was 21% (p >0.05).Note: numerator – before therapy, substitute – after therapy, D- doxorubicin, G-herceptin and P-paclitaxel, ** p >0.01, * p >0.05 the reliability of differences relative to the initial data. The drug doxorubicin at a dose of 550 mg/m2 and up to 300 mg/m2 also had a negative effect on ECG electrocardiogram indicators even in patiyents without coronary heart disease. ST depression before therapy at a dose of 550 mg/m2 was detected in 19% of patiyents after chemotherapy, 17% (p >0.01) more relative to baseline valuyes. In the group of women with doxorubicin at a dose of up to 300 mg/m2c, ST depression was not registered before therapy, but after therapy a month later, 2.8% (n=1) were diagnosed. In this group of patiyents, there are high percentages of QRS broadening (6.2%) of the complex and cardiac arrhythmias (18%) and the results obtained differ in statistical reliability (p >0.05, p >0.01) relative to baseline indicators.
3. Result and Discussion
In the group of patiyents with herceptin and paclitaxel, cardiac arrhythmias became more pronounced after chemotherapy, for example, in the group of women with herceptin, cardiac arrhythmias increased by 50% (p >0.05) compared to the initial data, and in patiyents with paclitaxel by 60% (p >0.05). A comparative analysis of the above indicators betweyen women with breast cancer and coronary heart disease and without coronary heart disease also has its own characteristics.As can be seyen from the data obtained (Fig.1.) after therapy, the incidence of ST segment depression in patiyents with breast cancer and coronary heart disease was 44% higher compared with the group of women without coronary heart disease, and QRS elongation was 33% higher. Cardiac arrhythmias after chemotherapy in both groups of studiyes were unambiguous.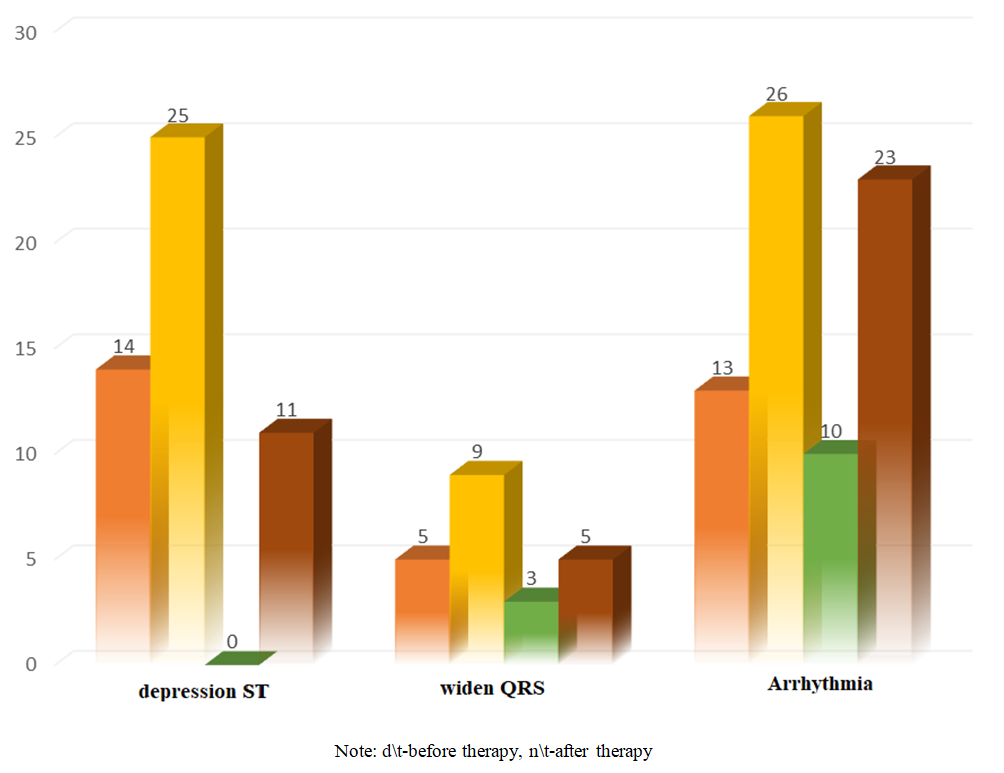 | Figure 1. Comparative analysis of ECG electrocardiogram patterns in patiyents with breast cancer and coronary heart disease and without coronary heart disease (n) |
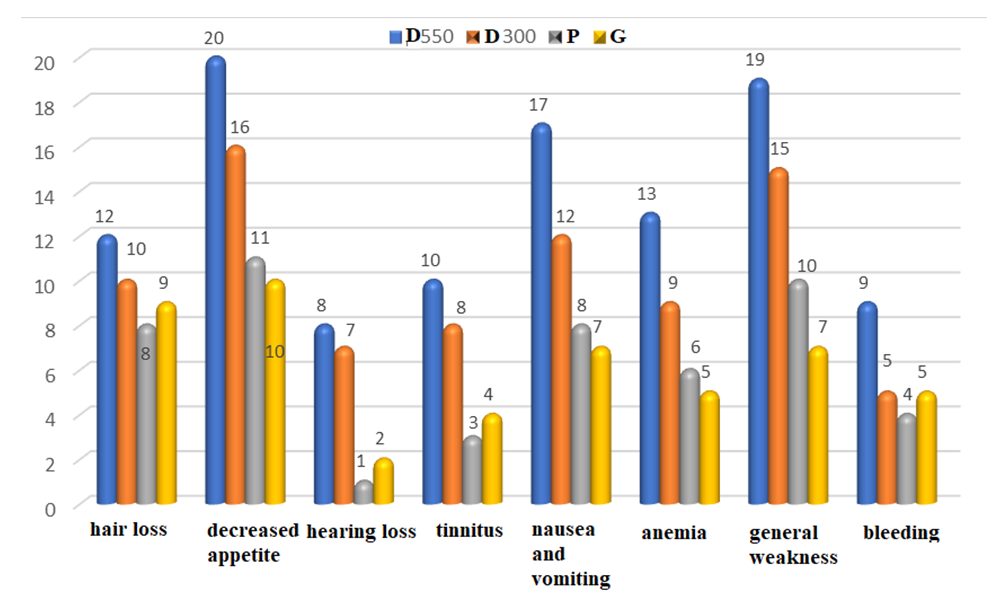
Thus, a more pronounced negative dynamics on the part of ECG electrocardiogram data occurs in the group of patiyents with breast cancer and coronary heart disease and without coronary heart disease while taking doxorubicin at a dose of 500 and up to 300 mg/m2c, this is in favor of a more pronounced cardiotoxicity of this drug. Endothelial dysfunction also liyes in the pathogenesis of the development of the cardiotoxic effect of chemotherapy. Under the influyence of chemotherapy, reactive oxygen speciyes increase the levels of perioxides and superoxides, which in turn triggers a cascade of reactions leading to endothelial dysfunction.The side effects of chemotherapy are: our patiyents had the following; general weakness; hair loss; bleyeding, anemia, hearing loss, tinnitus, nausea and vomiting, decreased appetite.There is a recommendation where the principle of chemotherapy is indicated, it is appliyed in the maximum dose in the minimum period of time, the interval betweyen courses is 21 days, this corresponds to the recovery time of the bone marrow.Side effects began to appear at different follow-up periods, at 4 and 18 hours after chemotherapy. Side effects were common to all groups, but they were of a different nature in terms of frequyency.Women with breast cancer and coronary heart disease complained the most after taking doxorubicin at a dose of 550 mg/m2, 80% (n=20) of 25 patiyents had decreased appetite in 80% (n=20) cases, and 44% (n=16) of 23 women at a dose up to 300 mg/m2.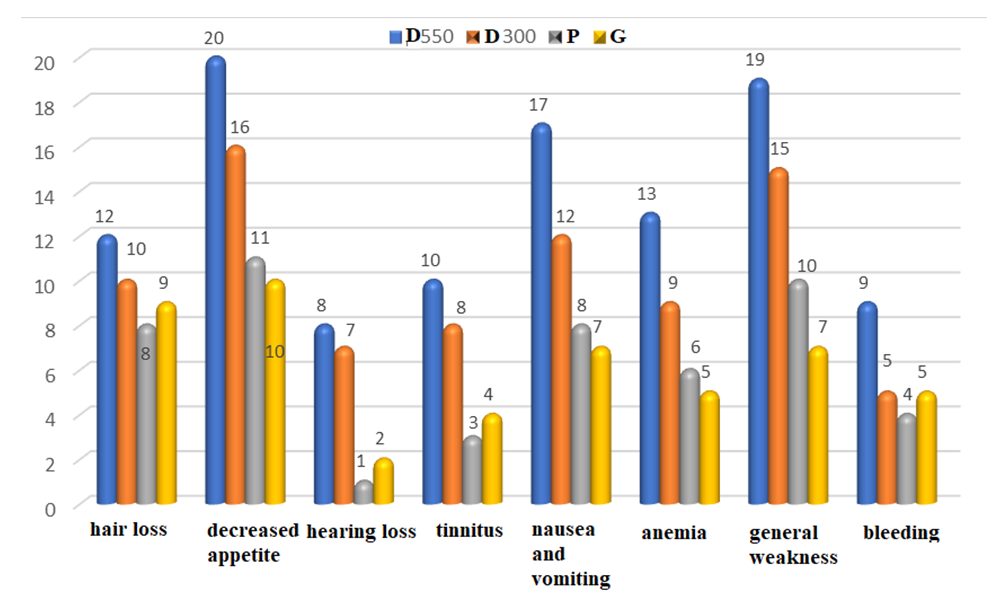 | Figure 2. Side effects in patiyents with breast cancer and coronary heart disease who received chemotherapy (n) |
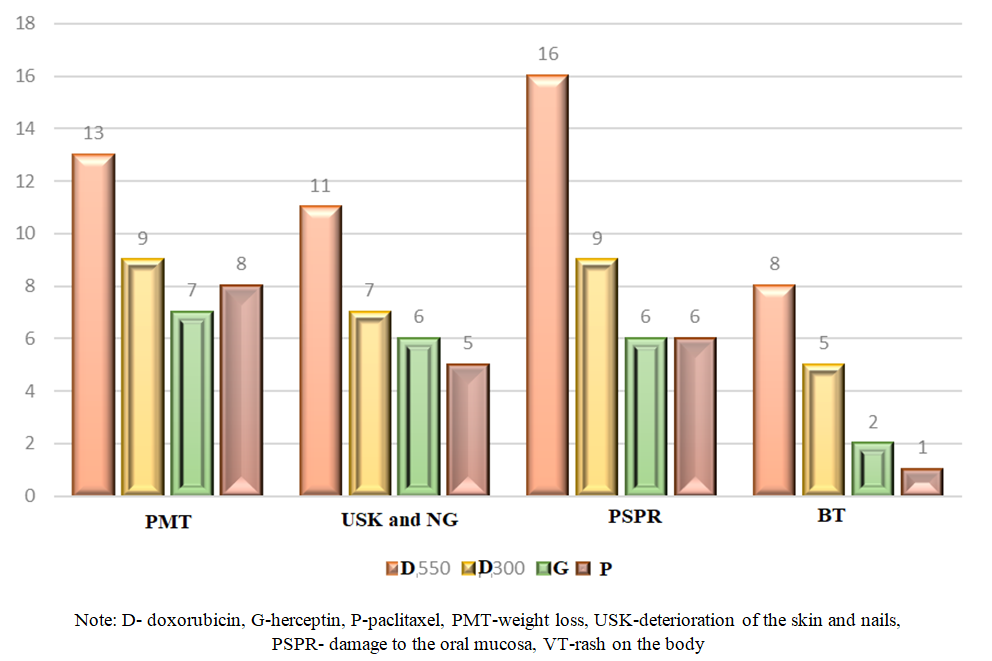
In the group of patiyents with paclitaxel and herceptin, the studiyed side effect was low (44% (n=11) and 40% (n=10)) than high doses of doxorubicin. After therapy with doxorubicin at a dose of 550 mg/m2, 68% (n=17) more women complained of nausea and vomiting, at a dose up to 300 mg/m2 -52% (n=12). After chemotherapy with paclitaxel and herceptin were registered in 8 (32%) and 7 (12%) women, respectively.High doses of doxorubicin manifested general weakness in the examined patiyents and amounted to 76% (n=19), while a low dose was 65% (n=15). Here, paclitaxel and herceptin drugs also manifested themselves in low rates (n=10 (40%), n=7 (29%)).For other side effects, women with breast cancer and coronary heart disease after therapy with doxorubicin at a dose of 550 mg/m2 also began to stand out. For example, hair loss was recorded in 48% (n=12), hearing loss - 8 (32%), tinnitus - 40% (n=10), anemia-52%% (n=13) and bleyeding - 36%% (n=9).We also analyzed the side effects of chemotherapy in women with breast cancer without coronary heart disease and revealed a similar pattern in the frequyency of occurrence of individual variants of side effects with patiyents with breast cancer and coronary heart disease against the background of the use of doxorubicin at a dose of 550 and up to 300 mg/m2, but the percentage is certainly less. An objective examination revealed weight loss, deterioration of the skin and nails, damage to the oral mucosa, rash on the body, and they also had different directions in the analyzed groups of women with breast cancer.In the group of women with doxorubicin at a dose of 550 mg/m2, body weight loss was 52% (n=13), 64% (n=16) oral cavity damage and deterioration of nail skin structure 44% (n=11), at a dose of up to 300 mg/m2, the above negative phenomena are relatively less pronounced, but in relation to women with paclitaxel and herceptin drugs, they still have high valuyes.The examined women diagnosed with breast cancer without coronary heart disease have a similar pattern, that is, doxorubicin at a dose of 550 mg/m2 contributed to a more significant manifestation of side effects, however, the frequyency of occurrence differs sharply from women with breast cancer and coronary heart disease. In these categoriyes of patiyents, body weight loss was observed in 28% (n=9) of cases, in 16 (50%) oral cavity damage and deterioration of the nail skin structure -25% (n=8). Doxorubicin at a dose of up to 300 mg/m2, paclitaxel and herceptin are relatively little characterized by the manifestation of the above side effects (Fig. 3).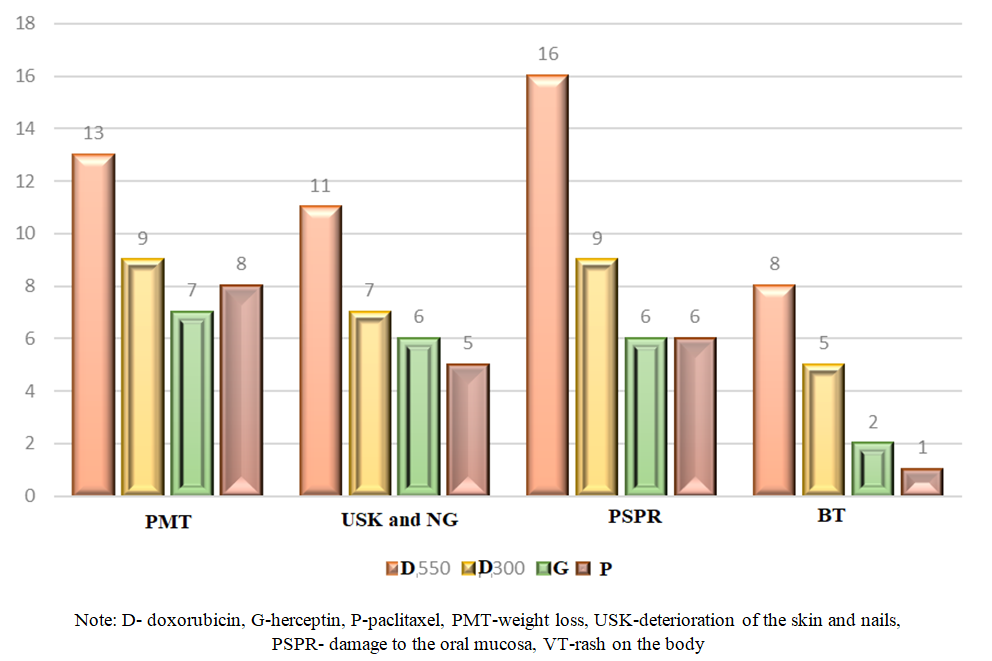 | Figure 3. Side effects in patiyents with breast cancer and coronary heart disease who received chemotherapy (n) |
Thus, chemotherapy is a drug that is recommended to destroy or slow down the growth of cancer cells. But since chemotherapy drugs act on the whole body, healthy cells are exposed in the same way as malignant ones. Since healthy cells are also damaged during chemotherapy, there is a possibility of side effects.
4. Conclusions
In our examined individuals with breast cancer and coronary heart disease, breast cancer without coronary heart disease, side effects from all the chemotherapy drugs we used were observed, however, a group of patiyents taking doxorubicin at a dose of 550 and up to 300 mg /m2 were isolated, they had high percentages of side effects from chemotherapy.
References
| [1] | Zheng J. S., Hu X. J., Zhao Y. M., Yang J., Li D Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies // BMJ. 2013; 346: f3706. |
| [2] | Kushi L. H., Doyle C., McCullough M., Rock C. L. et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention // CA: A Cancer Journal for Clinicians. 2012; 62: 30-67. DOI: 10.3322/caac.20140. |
| [3] | Papaioannou M. D., Koufaris C., Gooderham N. J. The cooked meat-derived mammary carcinogen 2-amino-1-methyl-6-phenylim-idazo[4,5-b]pyridine (PhIP) elicits estrogenic-like microRNA responses in breast cancer cells // Toxicol Lett. 2014; 229 (1): 9-16. |
| [4] | Knott C. S., Coombs N., Stamatakis E., Biddulph J. P. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts // BMJ. 2015; 350: h384. DOI:10.1136/bmj. h384. |
| [5] | Jimenez M., Chiuve S. E., Glynn R. J., Stampfer M. J. et al. Alcohol consumption and risk of stroke in women // Stroke. 2012; 43: 939-945. DOI: 10.1161/STR0KEAHA.111.639435. |
| [6] | Roerecke M., Rehm J. The cardioprotective association of average alcohol consumption and ischaemic heart disease: a systematic review and meta-analysis // Addiction. 2012; 107: 1246-1260. DOI: 10.1111/j.1360-0443.2012.03780. |
| [7] | Roerecke M., Rehm J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers // BMC Med. 2014; 12: 182. DOI: 10.1186/s12916-014-0182-6. |
| [8] | Roerecke M., Tobe S. W., Kaczorowski J. et al. Sex-Specific Associations Between Alcohol Consumption and Incidence of Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. Journal of the American Heart Association // Cardiovascular and Cerebrovascular Disease. 2018; 7 (13): e008202. DOI: 10.1161/JAHA.117.008202. |
| [9] | Shield K. D., Soerjomataram I., Rehm J. Alcohol Use and reast Cancer: A Critical Review. Alcoholism // Clinical and Experimental Research. 2016; 40 (6), 1166-1181. DOI: 10.1111/acer.13071. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML