Akilov K. A., Mirzakarimov B. Kh., Karimov D. K., Yulchiev K. S.
Center for the Development of Professional Qualifications of Medical Workers, Tashkent. Andijan State Medical Institute, Andijan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Surgical diseases of the genital organs should be the focus of attention of general practitioners, pediatric surgeons and urologists. This is often due to the difficulty of diagnosis and the low effectiveness of conservative treatment, which often leads to the death of the testicle, an important part of the reproductive system. Acute testicular disease suffered in childhood is the main cause of reproductive and spermatogenic dysfunction in adulthood.
Keywords:
Testicle, Acute, Hydotid, Orchitis, Children
Cite this paper: Akilov K. A., Mirzakarimov B. Kh., Karimov D. K., Yulchiev K. S., Optimization of Methods for Diagnosis of Acute Ovarian Inflammation, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 255-258. doi: 10.5923/j.ajmms.20241402.19.
1. Background
The problem of acute scrotum (AS) in children is one of the most pressing problems in pediatric surgery, accounting for about 20% of all emergency pathologies in childhood [1-4]. Among acute testicular diseases in children, the first place in terms of prevalence is pathology of the testicles and epididymis (torsion and necrosis of the hydatid). The next place is occupied by testicular torsion, nonspecific orchiepididymitis [5-8], and traumatic injuries. Most of the above conditions require prompt diagnosis [8-9]. In conclusion, it is necessary to develop general and non-invasive criteria, such as ultrasound, when diagnosing AS in such cases.
2. Purpose of the Study
Optimization of methods for non-invasive diagnosis of acute testicular inflammation in children.
3. Materials and Research Methods
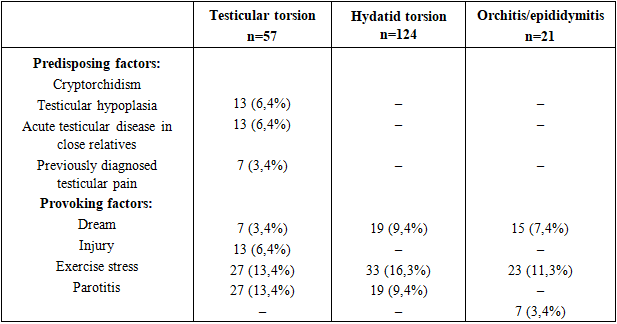
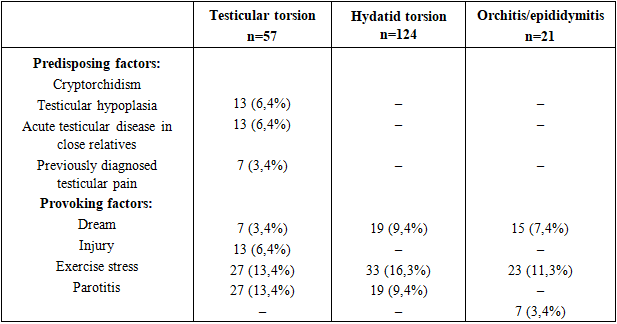
The clinical picture of the disease was assessed in 202 children who were treated with a diagnosis of AS in the emergency surgery and urology departments of the Andijan Regional Children's Multidisciplinary Medical Center during 2015-2022. Analyzes were carried out in 3 groups. In boys with testicular torsion in the 1st group (n=57), in the 2nd group - torsion of the epididymis (n=124), in the 3rd group - with orchiepididymitis (n=21). The following reasons have been identified that could provoke Syndrome acute scrotum (SAS) when collecting anamnesis vitae. In 13 patients (6.4%), prone to acute testicular diseases, testicular torsion occurred against the background of cryptorchidism. 13 of the operated children (6.4%) were under the supervision of a urologist and endocrinologist due to testicular hypoplasia detected in them. one child was also treated with human chorionic gonadotropin. From the anamnesis of 1 patient with intrauterine testicular torsion, it was revealed that his brother was also operated on as a newborn with the same diagnosis two years ago. Also, from the anamnesis, we identified testicular torsion in 1 patient with close relatives. In groups of children diagnosed with hydatid torsion and orchiepidymitis, no such cases were identified. (Table 1). Table (1). Predisposing and provoking factors of acute diseases of the scrotum
 |
| |
|
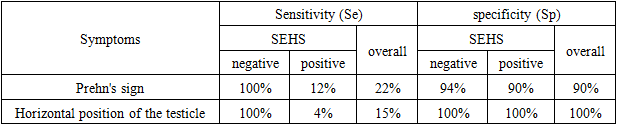
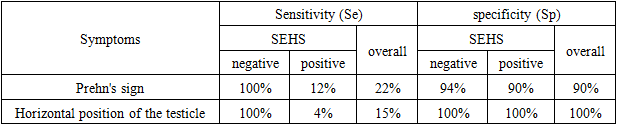
Short-term and self-limiting testicular pain was observed in 7 (3.4%) patients with testicular torsion, 19 (9.4%) with hydatid torsion and 15 (7.4%) with orchiepididymitis. The cause of exacerbation in the group of children with testicular torsion in 27 (13.4%) patients was trauma, and in 23 (11.3%) it was physical strain. In 13 (6.4%) adolescents, testicular torsion occurred during sleep. Torsion of the epididymis in 33 (16.3%) children was due to trauma, and in 19 (9.4%) after physical activity. No hydatid torsion was noted.. Orchiepididymitis developed in 23 (11.3%) children after injury, in 7 (3.4%) patients against the background of mumps. Sudden movements in our observation did not cause inflammation of the testicles and epididymis.Particular attention in the history of this disease was directed to common initial reactions, such as nausea, vomiting and increased body temperature. With testicular torsion, the disease began acutely in 40 (83.3%) patients, and gradually in 8 (16.8%) patients. Testicular torsion in newborns began acutely in 2 cases (22.2%) and subacutely in 7 cases (77.8%). Hydatid torsion, respectively, was acute in 26 (20.9%) and subacute in 100 (80.6%). In orchitis/epidymitis, acute in 3 (14.2%), and subacute in 18 (85.7%). An increase in body temperature above 37.0° was mainly observed in orchiepididymitis (6 cases (28.5%)) and with testicular torsion (12 cases (25.0%)). In newborns with testicular torsion and hydatid torsion, increased body temperature was observed in rare cases (2 (22.2%) and 12 (9.6%) patients, respectively). The main symptoms of testicular torsion were nausea and vomiting - in 4 cases (3.2%) versus 14 cases (29.2%) of Morgani hydatid torsion and in 2 cases (9.5%) orchiepidymitis.Local symptoms are the basis for making a diagnosis of COM. The first place is occupied by Prehn's symptom. Moyakning buralib kolishida y 22.8% cholat (13 nafar) and izhobiy baldi. Hydatid torsion and epididymitis orchioepididymitis were observed in 17 and 3 patients (13.7% and 14.2%, respectively). The horizontal position of the testicle was noted only when it was twisted (9 people (15.9%)). In cases of hydatid torsion and epididymitis, this symptom was always negative. Diffuse pain in the testicle was observed with testicular torsion in 98.2% of cases (56 observations). Local pain in the projection of the epididymis most often occurred with testicular torsion (48.4%), less often with orchiepididymitis (19.0%), in testicular torsion was observed only in 2 (3.5%) patients. In 30.6% of cases (38 people), a formation with a diameter of 0.5 cm was found at the upper pole of the testicle in torsion of the epididymis during palpation. In the group of children diagnosed with orchiepididymitis, this condition was noted in 14.3% (3 people). Secondary inflammatory changes in the layers of the scrotum were found in 89.5% (51 cases) of testicular torsion. In children with hydatid torsion and orchiepididymitis, local swelling and redness occurred in 79.0 and 66.7% of cases. The clinical diagnosis of testicular torsion was consistent with the final conclusion in 40.3% of cases (23), in 52.6% of cases it was suspicious (30). Hydatid testicular torsion was definitively diagnosed before surgery in 54 (43.5%) patients, and in 25 (20.2%) patients the diagnosis was suspicious. In the group with orchiepidymitis, only in 19.0% of cases (4 patients) the diagnosis was made without surgical intervention.In each group of patients, local inflammatory changes in the epithelial layers were studied. The patients were divided into two subgroups. The first subgroup included patients admitted before the development of edema-hyperemia of the scrotum, the second included children with inflammatory infiltration of the scrotum. In case of testicular torsion, in case of positive testicular edema-hyperemia syndrome, Prehn's symptom was positive in 100% of cases of observation, in case of negative testicular torsion - in 13.7%. Also, the horizontal position of the testicle was observed in 100% of all patients of the first subgroup and only in 5.8% of boys of the second subgroup. In conditions of the syndrome of edema and hyperemia, in 2 patients there was a predominance of pain in the upper pole of the testicle, and palpation revealed the presence of an additional formation in the projection of the epididymis (3.9%), which was not observed in the absence of edema and infiltration of the scrotum. In all patients, the first subgroup (100%) and only in 15 (29.4%) children of the second subgroup the clinical and postoperative diagnoses corresponded.In children with testicular torsion, a positive Prehn's sign was detected in 7 (16.7%) patients before the development of placental swelling and hyperemia syndrome and in 20 (12.2%) patients after the development of this syndrome. Horizontal position of the testicle was not observed in children with hydatid damage.Pain in the upper pole of the testicle and damage to the hydatid during palpation were detected in all children before the onset of local inflammatory reactions (24 patients (100%)), while pain in the area of the epididymis was observed in 36 (36.7%) patients with swelling-hyperemia syndrome testicle, damage to the hydatid during palpation was noted in 12 (12.2%) children. The agreement between the clinical diagnosis and the final conclusion was 83.3% (20 people) in the first subgroup and only 34.7% (34 people) in the second subgroup.In 2 (14.3%) children with ovarian swelling and hyperemia syndrome, a positive Prehn's sign was noted and a horizontal position of the testicle was not observed. In the absence of local inflammatory changes in the layers of the scrotum, pain inside and behind the testicle was observed in 50% of patients. After the addition of the syndrome of swelling and hyperemia of the scrotum, diffuse pain syndrome began to have a significant predominance (13 observations (92.8%)). In the first subgroup, 2 (33.3%) children had an additional formation in the upper pole of the testicle upon palpation, and in the second group this symptom was positive in only 3 (5.5%) patients. The agreement between clinical and final diagnoses was 33.3% (2) in the first subgroup versus 14.3% (2) in the second subgroup.From the point of view of proven medicine, the value of diagnostic tests is determined by their sensitivity (Se) and specificity (Sp) [3]. Regardless of the presence or absence of secondary inflammatory changes in the layers of the scrotum, the sensitivity and specificity of the listed symptoms in the clinical diagnosis of testicular torsion and its scrotum are presented in Tables 2 and 3. Information obtained from surgical examination of the testicle was used as the “gold standard” for diagnosis.Table (2). Sensitivity and specificity of symptoms before and after the development of scrotal edema and hyperemia syndrome (SEHS) in the diagnosis of testicular torsion
 |
| |
|
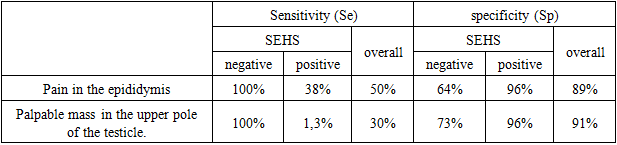
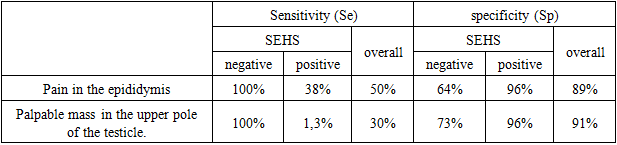
Table (3). Sensitivity and specificity of symptoms before and after the development of scrotal edema and hyperemia syndrome (SEHS) in the diagnosis of epididymal torsion
 |
| |
|
The table shows that the sensitivity and horizontal position of the testicle for the clinical diagnosis of torsion of the hydatid Morgani with local pain and palpable formation are very high (100%). However, it decreases sharply with the development of local inflammatory changes in the layers of the scrotum. Considering that 80% of children admitted to a surgical hospital have symptoms of scrotal edema and hyperemia, the overall diagnostic value of these clinical symptoms is not so great. At the time of hospitalization in the hospital, all children underwent a general blood and urine test. In children with acute testicular disease, the most informative indicators of a general blood test are: leukocytosis (109/l) was significantly more common in COM - 29.8% versus 23.8% with orchiepididymitis and 9.7% with damage to the hydatid (r=0.016). In children with orchiepididymitis (r=0.015), eosinophilia significantly predominated (28.5%), 20 cases (16.1%) of children with hydatid torsion were noted, while testicular torsion was only 7.0% (4 observations). Neutrophilia was rare: with torsion of the gonads - 10.5% and with orchitis and epididymitis - 9.5%. At the same time, analysis of variance did not reveal significant differences in these indicators (P>0.05). In cases of hydatid lesions, neutrophilia was not observed. In children with orchiepididymitis, lymphocytosis was reliably observed in 52.4% of cases (r = 0.009), while with testicular and hydatid torsion this figure decreased to 33.1% and 12.3%, respectively. Accelerated ESR was also more often observed in epididymitis orchioepididymitis (28.2%) compared with hydatid injury (20.2%) or testicular torsion (8.8%). However, analysis of variance did not show statistical significance of this indicator in all groups of children (P>0.05).In our study, the pathognomonic sensitivity of Prehn's sign in children with testicular torsion before the development of scrotal edema and hyperemia syndrome was high (95–98%). After the addition of secondary inflammation, the diagnostic value of this symptom decreased to 12%. Of particular note is the false-positive Prehn syndrome, found in 13.2% and 7.7% of cases of hydatid torsion and epididymitis orchioepididymitis, respectively. It is important to note that false-positive Prehn syndrome was predominantly observed in patients with hydatid torsion and epididymitis orchioepididymitis in combination with elevated testis syndrome (pulling the scrotum to the root) of a damaged hydatid and testicular torsion. Thus, Prehn's sign, considered a pathognomonic sign of testicular torsion, may not be detected in other nosological forms of “acute scrotum.” In our opinion, with hydatid torsion and epididymitis, tightening of the damaged testicle due to increased cremasteric reflex due to pain syndrome, doctors mistakenly interpreted this condition as Prehn's symptom.The symptom of a horizontal position of a twisted testicle did not give false positive results (specificity - 100%) and occurred in all patients before the development of edema and infiltration of the scrotal sac. However, testicular torsion in combination with edema-hyperemia of the scrotum was noted only in 5.5% of cases (sensitivity - 4%) and in newborns it was not detected at all. In young children with testicular torsion, changes in the scrotum have acquired specific features. In this case, hemorrhagic pus is visible through thin skin, which serves as a reason for differential diagnosis with hematocele.When determining the localization of pain in the testicle, in almost all children with gonadal torsion the pain was diffuse. With torsion of the hydatid (before the addition of secondary inflammatory changes), in all cases local pain was clearly manifested in the upper pole of the testicle, where damage to the hydatid could be palpated (sensitivity - 100%). however, the specificity of these symptoms was 64% and 73%, respectively. With the development of testicular edema-hyperemia syndrome, the pain was more diffuse in form, which was associated with the development of secondary orchitis, and the damaged hydatid could rarely be palpated due to the accumulation of fluid in the skin of the vaginal layer. A 50/50 ratio of testicular/epididymal pain was observed in late orchitis and epididymitis with local swelling and infiltration of the scrotum. When the layers of the scrotum were involved in the inflammatory process, 94.5% of patients had diffuse pain. The diffuse pain with epididymitis observed in our study, in our opinion, is associated with secondary inflammatory reactions in the testicle and scrotum. Interestingly, in 15.4% of cases of orchiepididymitis, an additional formation was palpated in the area of the upper pole of the testicle, which was regarded as a damaged hydatid. However, during surgical interventions, no additional formations were identified. In our opinion, a significantly enlarged testicle was mistakenly perceived as an additional formation. The predominance of leukocytosis during testicular torsion indicates the activity of the inflammatory response to more serious damage. Frequent lymphocytosis in epididymitis indirectly indicates the predominance of viral etiology of inflammation.Thus, local symptoms of acute testicular diseases in young children have a high sensitivity in the initial period of the disease (up to 100%), after combination with inflammatory changes in the testicular bursa, this sensitivity decreases significantly (up to 4–38%). % for individual symptoms). In children, the specificity of local symptoms in COM syndrome remains high during all periods of the disease, but does not help in the differential diagnosis between different nosological units of this syndrome. At the same time, anamnesis data, the nature of the general reaction of the body, indicators of general clinical blood and urine tests do not allow differential diagnosis between different nosological units of SAS.
References
| [1] | Minaev S.V. Ultrasound examination in the syndrome of “acute scrotal edema” in children. / S.V. Minaev, Yu.N. Bolotov, N.N. Pavlyuk // Surgery, 2008. No. 4. – pp. 55–58. |
| [2] | Sato N. Clinical study on 16 cases of testicular torsion / N. Sato, Z. Lee, M. Fujita // Hinyokika Kiyo. 2019 Nov; 35(l 1): 1877-80. |
| [3] | Hassan H & Farag D. The impact of polycystic ovary syndrome on women’s quality of life: Nursing guidelines for its management. Clinical Nursing Studies, 2019, 7(3):42-57. doi: 10.5430/cns.v7n3p42. |
| [4] | Hassan H. The Impact of Evidence-Based Nursing as The Foundation for Professional Maternity Nursing Practices. Open Access Journal of Reproductive System and Sexual Disorder, 2019; 2(2): 195-197. OAJRSD. MS. ID.000135. DOI: 10.32474/OAJRSD.2019.02.000135. |
| [5] | Aboev 3. A. Acute diseases of the scrotal organs. Clinic, diagnosis and treatment: abstract. diss. ...cand. honey. Sci. // 3. A. Aboev. – Moscow, 2001. – 95 p. |
| [6] | Averchenko M.V. Ultrasound diagnosis of volumetric fluid formations of the scrotal organs in children / V.I. Averchenko, I.A. Karachev, S.Yu. Komarova // Ninth Russian Congress “Innovative technologies in pediatrics and pediatric surgery”. – M., 2020. – P. 332. |
| [7] | Ishizu K. Two cases of testicular infarction: the usefulness of enhanced MRI for preoperative diagnosis / K. Ishizu. // Hinyokika Kiyo. Mar 2019; 45(3): 203. |
| [8] | Tereshchenko A.E. Immunological disorders in testicular torsion in children / A.E. Tereshchenko, V.P. Chernysho, A.N. Zinchenko // Vest. surgery named after I.I. Grekova, 2016. No. 5. – pp. 103–105. |
| [9] | Fenner M.N. Testicular scanning: evaluating the acute scrotum in the clinical setting. M.N. Fenner, D.A. Roszhart, J.H. Texter // Urology, 2021 Sep; 38(3): 237-41. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML