-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 4(2): 248-251
doi:10.5923/j.ajmms.20241402.17
Received: Jan. 16, 2024; Accepted: Feb. 1, 2024; Published: Feb. 8, 2024

Optimization of Surgical Treatment of Biliary Pancreatitis
Ishankulov Odil Azamkulovich, Kurbaniyazov Zafar Babajanovich, Zayniev Alisher Faridunovich, Kurbaniyazov Bobojon Zafarjonovich
Samarkand State Medical University, Uzbekistan
Correspondence to: Ishankulov Odil Azamkulovich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance of the study. Pancreatitis of biliary genesis accounts for 26% to 60% of cases of acute pancreatic inflammation. Purpose of the study. Improving the results of surgical treatment of patients with biliary pancreatitis. Materials and methods of research. The study was based on the analysis of clinical data of 116 patients with acute and chronic biliary pancreatitis treated at the multidisciplinary clinic of Samarkand State Medical University from 2012 to 2023. Results and their discussion. Surgical treatment was performed in 94 (81.1%) patients. Determination of surgical tactics and choice of the type of surgical aid were based on the etiologic form of the disease. Conclusions. Differentiated stage application of modern minimally invasive surgical techniques allows to achieve satisfactory results in treatment of patients with chronic biliary pancreatitis in 71,1%. At acute biliary pancreatitis elimination of the leading factors of pathogenesis in 66,7% of cases is possible due to the use of endoscopic and endovideosurgical techniques (EPST, laparoscopic interventions). The use of urgent EPST is effective in 31.6% of cases.
Keywords: Biliary pancreatitis, Surgical treatment, Minimally invasive methods
Cite this paper: Ishankulov Odil Azamkulovich, Kurbaniyazov Zafar Babajanovich, Zayniev Alisher Faridunovich, Kurbaniyazov Bobojon Zafarjonovich, Optimization of Surgical Treatment of Biliary Pancreatitis, American Journal of Medicine and Medical Sciences, Vol. 4 No. 2, 2024, pp. 248-251. doi: 10.5923/j.ajmms.20241402.17.
Article Outline
1. Relevance of the Study
- Pancreatitis of biliary genesis accounts for 26% to 60% of cases of acute pancreatic inflammation [2,6,8,12]. Chronicization of acute biliary pancreatitis reaches 43% of cases. The leading factors of pathogenesis of biliary pancreatitis are outflow disturbance through extrahepatic biliary tracts and ductal system of pancreas, occurrence of biliary-pancreatic reflux with development of intraductal hypertension. There is no unanimity in the issues of verification of the above factors and morphologic causes of their formation at the early stage of disease development [3,4,7,10].As a morphologic substrate of ductal hypertension, biliary concretions provoking acute pancreatitis by "transient" passage or by impingement in the greater duodenal papilla are most frequently diagnosed. With prolonged traumatization of the mucous membrane of the ducts, scar stricture of the distal part of the choledochus is formed, which is included in the pathogenesis of chronic biliary pancreatitis along with concretions [1,5,9,11].Given the constant growth in the number of patients with cholelithiasis and pancreatitis of biliary genesis, the study of diagnosis and treatment of these diseases, as well as the role of endoscopic and open surgical interventions remain relevant and require further development. The use of highly informative diagnostic and minimally invasive surgical technologies has led to significant changes in the tactics of management of patients with pancreatitis of biliary genesis.
2. Purpose of the Study
- Improving the results of surgical treatment of patients with biliary pancreatitis.
3. Materials and Methods of Research
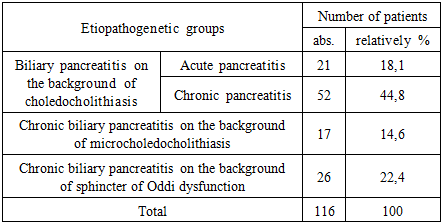
- The study was based on the analysis of clinical data of 116 patients with acute and chronic biliary pancreatitis treated at the multidisciplinary clinic of Samarkand State Medical University from 2012 to 2023.The criteria for inclusion of patients in the study were: the presence of clinico-instrumental confirmed acute pancreatitis combined with signs of biliary hypertension on the background of cholelithiasis, as well as secondary chronic changes of the pancreas with external secretory or endocrine insufficiency on the background of pancreatobiliary hypertension due to cholelithiasis, benign changes in the area of the large duodenal nipple.Acute biliary pancreatitis was diagnosed in 21 (18.1%) and chronic pancreatitis in 95 (81.9%) patients. Surgical interventions were performed in 94 (81.1%) patients, conservative treatment was performed in 22 (18.9%) patients. In the acute phase of the disease 21 patients were operated on. Interventions for chronic pancreatitis were performed in 73 patients.The mean age of men was 52.1±14.4 years, women - 55.2±12.7 years (20-90 years), examined by conventional methods (clinical examination, laboratory diagnosis, ultrasonography, esophagogastroduodenoscopy, radiologic examination of esophagus, stomach, duodenum, magnetic resonance cholangiopancreaticography). According to the results of clinical examination of patients, supplemented by laboratory and instrumental methods, etiopathogenetic groups of patients were distinguished (Table 1).
|
4. Results and Their Discussion
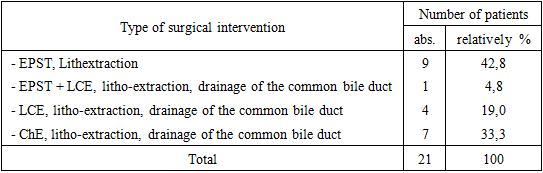
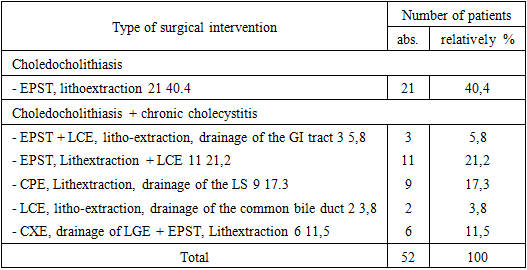
- Surgical treatment was performed in 94 (81.1%) patients. Determination of surgical tactics and choice of the type of surgical aid were based on the etiologic form of the disease.Surgical treatment in acute biliary pancreatitis was performed in 25 (11.3%) patients (Table 2).
|
|
|
5. Conclusions
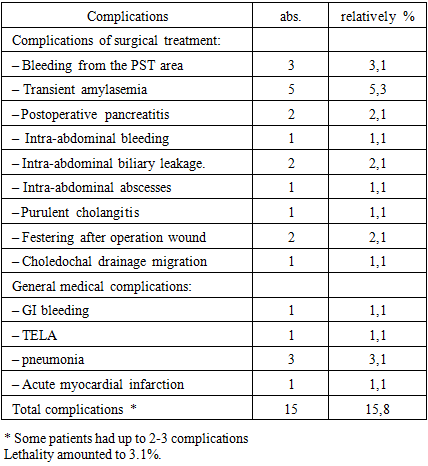
- The following etiopathogenetic factors were revealed in the structure of the causes of biliary pancreatitis: choledocholithiasis in 62.9% of cases, sphincter of Oddi dysfunction in 22.4%, microcholedocholithiasis was the cause in 14.6% of cases. In case of chronic biliary pancreatitis, the use of minimally invasive technologies (EPST, MBD stenting, laparoscopic interventions) leads to a reduction in hospitalization time o treatment. Differentiated stage application of modern minimally invasive surgical techniques allows to achieve satisfactory results in treatment of patients with chronic biliary pancreatitis in 71,1%. At acute biliary pancreatitis elimination of the leading factors of pathogenesis in 66,7% of cases is possible due to the use of endoscopic and endovideosurgical techniques (EPST, laparoscopic interventions). The use of urgent EPST is effective in 31.6% of cases.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML