-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 237-242
doi:10.5923/j.ajmms.20241402.15
Received: Jan. 19, 2024; Accepted: Feb. 2, 2024; Published: Feb. 4, 2024

Obstetric and Perinatal Outcomes in Pregnant Women with Placenta Previa and Placenta Accreta
Matyakubova S. A.1, Olimova N. X.2
1Director of Khorezm Regional Perinatal Center, Doctor of Medical Sciences, Khorezm, Uzbekistan
2Perinatal Center of Khorezm Region, Khorezm, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Placenta previa is defined as ultrasonography detection of placenta previa before delivery or by clinical examination during caesarean section. Aim of the study: Analysis of obstetric and perinatal outcomes in pregnant women with placenta previa and placenta accrete. Subjects and Methods: A retrospective descriptive study conducted at perinatal center of Khoresm region. Total 59 cases of placenta previa were included in this study which was admitted at our perinatal center during January 2021 to May 2023. Total patients 15289 delivered during this study period at our perinatal center. Results: Women who were admitted to the blood bank with a diagnosis of placental abruption or tissue growth were required to prepare a reserve of blood components in their group before the planned procedure. In the Department of Pathology of Obstetrics and Gynecology, women with the above diagnoses are marked in red lines on the observation boards. Conclusion: Women in all regions of the risk group should undergo an examination at our Perinatal Center during pregnancy. Women whose pregnancy is detected with the full advance of the placenta should be scheduled, if there are no signs of danger, at 36 weeks 0 days, the signs of danger in the dynamics include bloody discharge from the vagina, problems in the fetus. Prevention of severe complications was strengthened by solving at 34 weeks if the conditions are identified.
Keywords: Perinatal outcomes, Pregnant women, Placenta previa and placenta accrete
Cite this paper: Matyakubova S. A., Olimova N. X., Obstetric and Perinatal Outcomes in Pregnant Women with Placenta Previa and Placenta Accreta, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 237-242. doi: 10.5923/j.ajmms.20241402.15.
Article Outline
1. Topicality
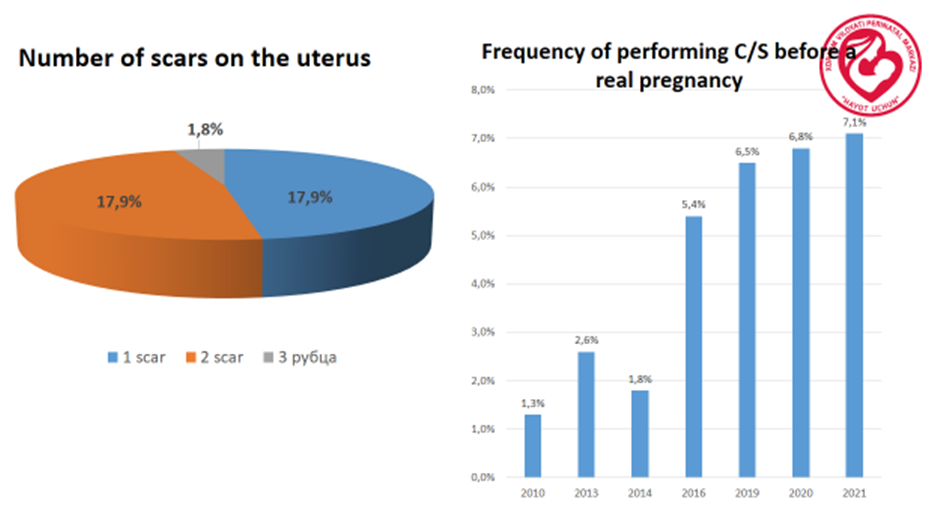
- Among the world Placenta previa, placenta accreta, and vasa previa are important causes of bleeding in the second half of pregnancy and in labor. Main risk factors for placenta previa contain prior cesarean delivery, pregnancy termination, intrauterine surgery, multifetal gestation, increasing parity, and maternal age. The diagnostic modality of choice for placenta previa is transvaginal ultrasonography, and women with a complete placenta previa should be delivered by cesarean. A few studies observe that, while the placenta to cervical os distance is greater than 2 cm, women may safely have a vaginal delivery. Regional anesthesia in oreder to cesarean delivery in women with placenta previa is safe. Delivery should take place at our perinatal center with adequate blood banking facilities. The occurence of placenta accreta is rising, primarily because of the rise in cesarean delivery rates.
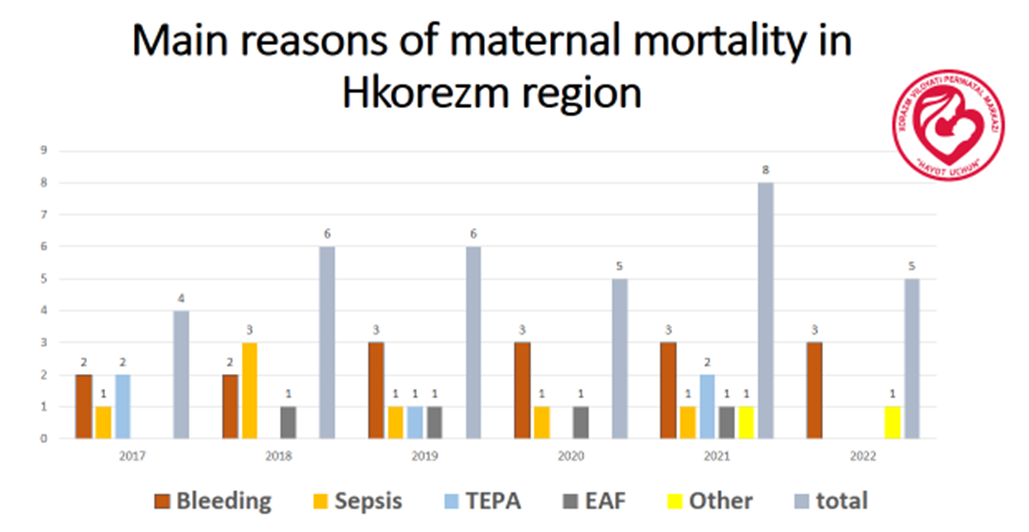
2. Aim of the Research
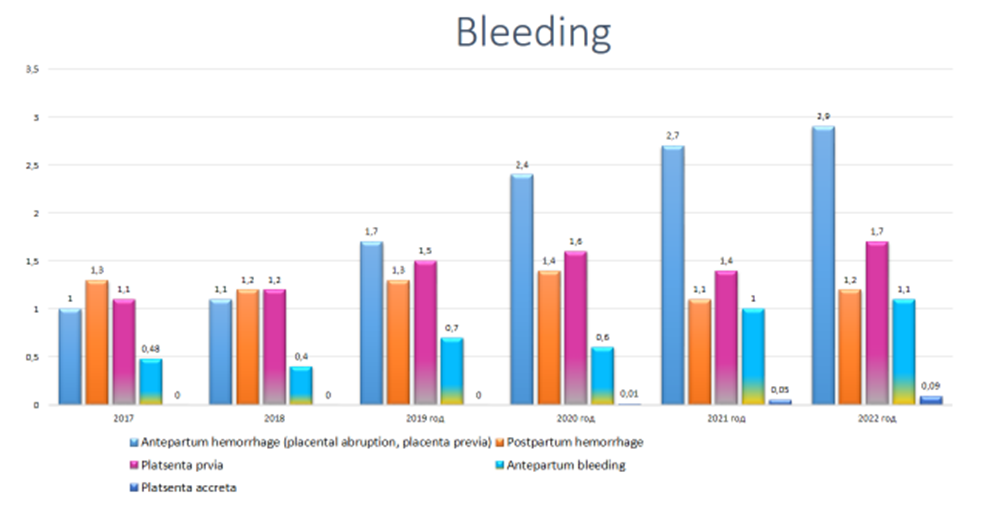
- This situation can be connected with massive blood loss at delivery. Prenatal diagnosis by imaging, followed by planning of peripartum management by a multidisciplinary team, may base reduce morbidity and mortality. Women known to have placenta accreta should be delivered by cesarean, and not take part in should be made to diveded the placenta at the time of delivery. The most of women with outstandingly degrees of placenta accreta will demand a hysterectomy. Although successful conservative management has been presented, there are not enough data to recommend this approach to management routinely. Clinically paramount important causes of bleeding during the second half of pregnancy and in labor include placenta previa, placenta accreta, and vasa previa. These situations are connected to significant maternal and perinatal mortality and morbidity. This review observed a contemporary evidence-based approach to the management of theseevedences.. Obstetric hemorrhage is first of the most common causes of maternal morbidity and mortality on the world. About one third of the all cases of ante partum hemorrhage be owned to placenta previa. Placenta previa is defined as implantation of placenta in lower uterine segment, overlying or approaching internal cervical os. Placenta previa effects approximately 0.3-0.4% of all labours. The most characteristic condition in placenta previa is sudden, painless and apparently causeless hemorrhage, which usually does not appear until near end of second between 12-24 weeks. Incidence of placenta previa is estimated to be 3to 4 per 1000 pregnancies. There are mainly factors, especially obstetrical, which has been identified to associated with placenta previa. Maternal age after 30 years, multiparity, previous cesarean delivery, previous abortions, previous history of placenta previa etc; has been conneced with increased risk of placenta previa. Placenta previa is considered high risk pregnancy because of the adverse maternal outcome like postpartum hemorrhage, cesarean hysterectomy, increased need for blood transfusion and septic problems and as a result of bleeding total organ disfuntions.
3. Material and Methods
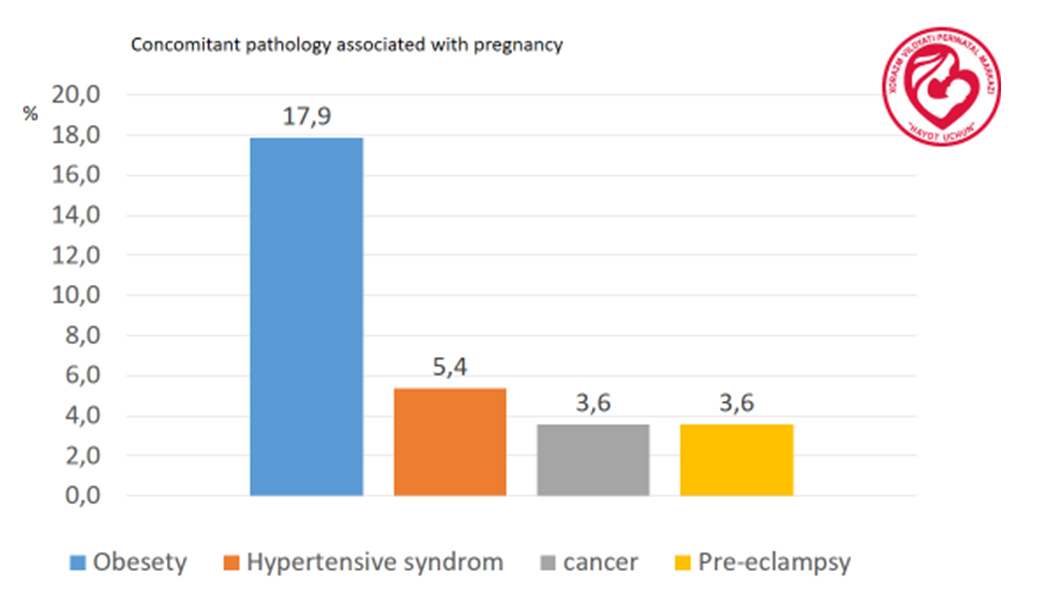
- The present study is a retrospective descriptive study conducted at perinatal center of Khoresm region. Total 59 cases of placenta previa were included in this study which were admitted at our Perinatal center during January 2021 to May 2023. Total patients 15289 delivered during this study period at our Perinatal center. Placenta previa was defined as ultrasonographic detection of placenta previa before delivery or by clinical examination during caesarean section. Objective of this study is to determine the incidence, demographic features, obstetric risk factors, obstetric management, maternal mortality and morbidity, perinatal outcome in women presenting with placenta previa. Main part of the pregnant women with placenta previa already diagnosed as placenta previa by ultrasonography irrespective of age, parity, blood and another analyses, demographic status is also. Pregnant gestational is age more than 28 weeks and 28 weeks also are included. A main part of patients which are referred from other hospitals, during the observation, regional obstetrical center s are also included some patients came with the complaint of vaginal bleeding. While some are diagnosed antenatally during routine sonography examinations. A few parts of patients went into labor spontaneously, while others are electively terminated due to heavy bleeding or fetal heart abnormalities. Data were collected regarding delivery data (presentation of fetus, mode of delivery and gestational age at delivery), neonatal data (birth weight, APGAR score at 1 and 5 minute and NICU admission) and maternal complications, seriously problems (post-partum hemorrhage, need for postpartum blood transfusion and peri-partum hysterectomy). Patient’s demographic details, history of previous pregnancy and risk factors, past medical surgical history and family history were noted. An analysis of maternal mortality and morbidity was done with respect to development of hypovolemic shock, DIC, anemia, acute kidney injury, septicemia and maternal deaths. In the study of pregnant women with placenta previa, we made full use of all the clinical laboratory tests available at the Perinatal Center of the Khorezm region. The women gathered for this study addressed the reception department with various complaints. In addition, 10% of women who complained of bleeding during duty hours and night duty had a pregnancy complicated by placenta previa. women in this contingent were on the doctor's list during pregnancy and had full ambulatory examinations. Necessary recommendations were given and the obstetrician was under the supervision of a gynecologist. Complaints of a large amount of bloody discharge from the vagina during admission were brought to the Medical Emergency Service or by relatives. During the initial assessment of the woman's condition during the examination, cases of hemorrhagic shock were observed in this contingent, and emergency cesarean section was performed. There were no cases of fetal death. But childbirth is a serious complication, including hemorrhagic shock. DVS syndrome, excision of uterus with both excesses, ligation of internal iliac arteries from both sides, intubation of intestines were performed. According to national standards, general blood and urine analysis, blood biochemical analysis, and blood type were determined from all women. An immediate order was placed for the blood components of his group general blood and urine analysis, blood biochemical analysis, coagulogram analysis, complete abdominal cavity and uterine-fetal state, dopplerography, specialist examinations are planned for women who are regularly admitted through the reception department. was admitted to the department of pregnant women with complications. All women had severe anemia and underwent a hematological examination. Blood components were routinely transfused.A course of corticosteroids was prescribed in order to prevent fetal distress syndrome in pregnant women with a risk of premature birth and less than 39 weeks of gestation. The blood coagulation system in pregnant women was observed dynamically based on coagulogram examination. Before the operation, the vagina was cleaned. The blood components of their group are prepared and the operational brigade is ready. Before the planned operation, the women were examined by a reanimatologist and an anesthesiologist, and the issue of anesthesia was resolved.This is a retrospective study of 59 cases of placenta previa, which were admitted in our Perinatal center during January 2021 to May 2023. All patients of placenta previa with gestational age > 28and 28 weeks up to full term were included in the study. All cases were confirmed by ultrasound examination. Outcome measures prevalence of placenta previa, maternal and neonatal outcomes, and case fatality rate. Among this patients Placenta previa associated with pre-eclampsia and obesity, extra-genitial diseases. That’s why all patients observed biochemical and total analyses of blood and urinary, PTI, ultrasound analysis.
 | Figure 1 |
4. Results
- The number of deliveries performed during the study period was 15289, of them, 59 cases were placenta previa. Previous birth among all pregnancy women who diagnosed by Placenta previa had normal vaginal delivery in 42% and 58% cesarean. According to number of pregnancies most of percentage proper to second and third pregnancies after cesarean, fourth pregnancy in 0.25%, 6.77% of fifth pregnancies. While previous cesarean were 17% proper to only one time uterine scar and 19% in double uterine scar, placenta previa was during the second and third pregnancy in 12.3%. In contrast by year, most of part of pregnancy occurred in 2010-2021, at the top with 19 numbers in 2011-2015 periods. The bleeding index separated main 4 groups according to the size of the bleeding. During the operation 74.5% of pregnancy were bleeding approximately 1000-1500 ml, 13.5% in until 2000 ml and 6.7% 300-3500 ml. In 3 woman complicated with hemmoragic shock.
 | Figure 2 |
 | Figure 3 |
5. Discussion
- There is consensus that a placenta previa that totally or partially overlies the internal cervical os requires delivery by cesarean. However, the mode of delivery when the placenta lies in proximity to the internal os is more controversial. Three small retrospective studies using transvaginal or trans abdominal sonography have evaluated the role of ultrasonography in determining the optimal mode of delivery for women whose placentas were in proximity to the internal cervical os. 33–35 All 3 studies found that women in whom the distance between the lower placental edge and the internal cervical os was greater than 2 cm could safely have a vaginal delivery. Conversely, among women with a placenta-internal os distance less than 2 cm, the overwhelming majority required cesarean delivery, usually for bleeding. However, in none of these studies were the clinicians blinded to the results of the scan, and this may have influenced obstetric management. Furthermore, these studies had relatively small numbers. Nonetheless, the studies suggest that women with placenta previa should have a transvaginal sonogram in the late third trimester, and that those with a placental edge to internal os distance of less than 2 cm should be delivered by cesarean. It has been our experience that women with a placenta internal os distance of less than 2 cm who undergo a trial of labor almost invariably experience significant bleeding during labor, necessitating cesarean delivery. Consequently, it is now our practice to deliver these women by elective cesarean. Women whose placentas are 2 cm or more from the os undergo a normal labor. It is important though to realize that, in women with a placenta that extends into the noncontractile lower uterine segment who have a vaginal delivery, there is potential for postpartum hemorrhage.
 | Figure 4 |
6. Conclusions
- 1. In conclusion, as a result of this study, we can re-qualify all medical staff in primary care and make recommendations, algorithms for planning follow-up during pregnancy of women who have had a cesarean section, from rigorous and complete clinical analysis. we gave conclusions about the need to carry out inspections of the planned screen.2. Women in all regions of the risk group should undergo an examination at our Perinatal Center during pregnancy. Women whose pregnancy is detected with the full advance of the placenta should be scheduled, if there are no signs of danger, at 36 weeks 0 days, the signs of danger in the dynamics include bloody discharge from the vagina, problems in the fetus. Prevention of severe complications was strengthened by solving at 34 weeks if the conditions are identified.3. Women who were admitted to the blood bank with a diagnosis of placental abruption or tissue growth were required to prepare a reserve of blood components in their group before the planned procedure.4. In the Department of Pathology of Obstetrics and Gynecology, women with the above diagnoses are marked in red lines on the observation boards.Achieving positive outcomes with placenta previa, placenta accreta, and vasa previa depends on prenatal diagnosis and appropriate management at the time of delivery. Advances in ultrasonography have made it possible to diagnose all 3 conditions with reasonable accuracy, which allows appropriate management planning. Women with these conditions should be considered at high risk and should be delivered at our perinatal cents with skilled personnel, adequate blood transfusion facilities, and good neonatal resources. 90% of this pregnants diagnosed by ultrasound diagnostics our doctors. Our skilled personnel took part during the opearation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML