Kurbaniyazov Zafar Babajanovich, Khamroev G’ulom Abdug’anievich, Nurillaev Khusan Jamshidovich, Rakhmanov Kosim Erdanovich
Samarkand State Medical University, Uzbekistan
Correspondence to: Kurbaniyazov Zafar Babajanovich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Studied results surgical treatment 112 patients. An individualized approach to the surgical treatment of inguinal hernias in elderly and senile patients made it possible to reduce the frequency of specific long-term postoperative complications - hernia recurrence from 10.6% in the comparison group to 3.1% in the main group. An improved method of open prosthetic Lichtenstein plastic surgery with strengthening of the anterior and posterior walls of the inguinal canal eliminates the development of recurrent hernia, prevents scrotal swelling in the early postoperative period and is indicated in patients of older age groups with degenerative-dystrophic changes in the tissues of the inguinal region and high (ASA III - IV degree) operational and anesthetic risk. Laparoscopic hernioplasty using the TAPP method is characterized by low-invasiveness, early rehabilitation (reduction of treatment time by 2 times), better quality of life results. The presence of severe comorbid pathology (surgical and anesthetic risk grade III - IV according to ASA) limits its use (32.3% completed) elderly and senile patients.
Keywords:
Inguinal hernia, Elderly and senile age, Surgical treatment
Cite this paper: Kurbaniyazov Zafar Babajanovich, Khamroev G’ulom Abdug’anievich, Nurillaev Khusan Jamshidovich, Rakhmanov Kosim Erdanovich, Results of Surgical Treatment of Inguinal Hernia in Elderly and Senile Patients, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 231-236. doi: 10.5923/j.ajmms.20241402.14.
1. Relevance of the Research Topic
External abdominal hernias occur in 3-4% of the population, and among elderly and senile people - in 15-17%, which undoubtedly leads to a decrease in their quality of life, loss of ability to work and disability [2,10]. Among patients with external abdominal hernias, inguinal hernias account for approximately 80%. To treat them, various surgical methods are used, the number of which today reaches more than 1000, which indicates surgeons’ dissatisfaction with the results of treating this disease [1,4,8,13].Despite the improvement of hernioplasty methods, the percentage of hernia recurrences still remains high, the frequency of which varies according to the literature from 5 to 45% [6,9,12,14]. The introduction of new methods of surgical treatment has led to a significant reduction in the incidence of recurrent inguinal hernia (down to 1-5%). In clinics specifically involved in the diagnosis and treatment of inguinal hernias, the recurrence rate is reduced to a minimum and does not exceed 1-1.5% [3,5,7,11].The reasons for the recurrence of the disease cannot always be clarified, but are often a consequence of the standard use of one or more methods of plastic surgery without taking into account the topography of the groin area, the type of hernia, the age of the patient, and the condition of the tissues.
2. The Purpose of the Study
To improve the results of surgical treatment of inguinal hernias in elderly and senile patients by optimizing the choice of open prosthetic repair and laparoscopic TAPP hernioplasty.
3. Material and Methods
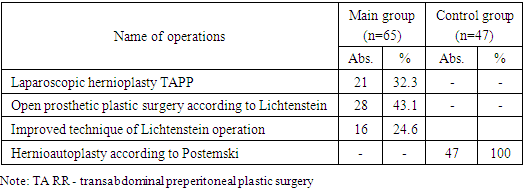
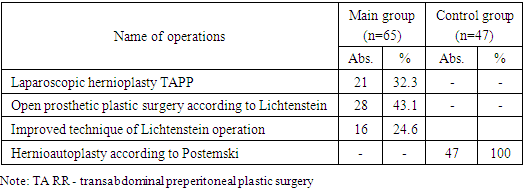
And learned results _ surgical treatment 112 patients with inguinal hernias seniors age groups hospitalized from 2014 to 2023 in the surgical department of the multidisciplinary clinic of Samarkand State Medical University, being clinical base of the Department of Surgical Diseases No. 1, Transplantology and Urology. IN main group entered 65 sick, at which tension-free prosthetic repair according to Lichtenstein (n = 28) and its improved technique (n = 16), as well as laparoscopic hernioplasty using the TAPP method (n = 21) were used. IN comparison group – 47 sick, at which tension methods were used hernioautoplasty according to Postempsky (n = 47).Table 1. Structure of surgical interventions for inguinal hernias in older patients age groups
 |
| |
|
The age of the patients ranged from 60 to 82 years. There were 15 (13.4%) patients over 75 years old, 97 (86.6%) aged 60-74 years.Patients PG With duration hernia before 1 year was 2 (1.8%), from 1 to 3 years – 16 (14.3%), from 3 to 5 years – 33 (29.5%) and more than 5 years – 61 (54.5%) observations. Main mass patients made up unilateral – 88 (78.6%) and irreducible PG – 31 (27.7%). Double sided PG were marked in 24 (21.4%).Researched patients distributed By classification inguinal hernias EHS (35th International Congress of the European Hernia Society, 2014).Table 2. Distribution of patients in older age groups By EHS classification of inguinal hernias (2014)
 |
| |
|
Analysis according to the EHS classification showed that 76.8% of older patients age groups hospitalized with primary hernias, A 23.2% - With recurrent. Only V 5 (4.6%) cases PG turned out to be oblique. Rest 95.4% patients hospitalized with straight PG (V 74.1% cases – 2nd class, in 24.2% - 3 class).U examined us patients more often In total, such concomitant pathologies were found as: IHD – 93 (83.0%), hypertension – 82 (73.2%), benign prostatic hyperplasia – 79 (70.5%), diabetes – 56 (50.0%) and pneumosclerosis – 33 (29.5%) cases.At studying degrees anesthesiological risk V compliance with scale A.S.A. at observed patients’ seniors age groups was It was found that the identified high risk was largely associated with the presence related pathologies from the outside cardiovascular system and at the same time in 22.3% stage III was stated. risk, in 1.8%, stage IV. Necessary Mark, what often met combination various related pathologies, What rendered significant influence on increasing degree _ risk upcoming surgical interventions.
4. Results and Its Discussion
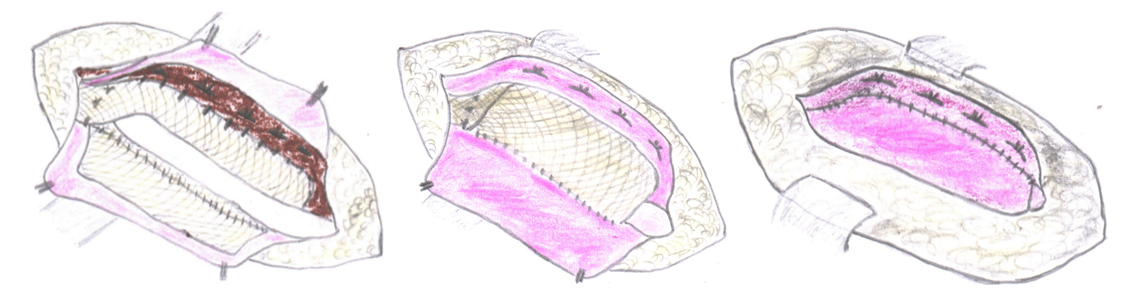
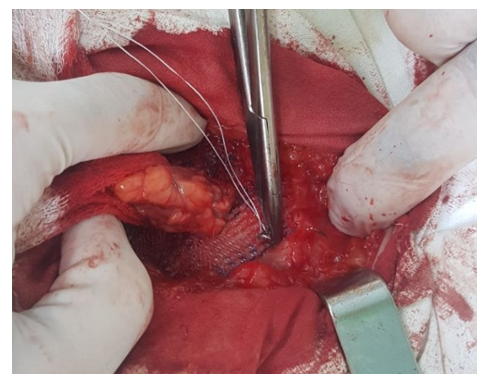
All patients were operated on as planned. The comparison group consisted of 47 patients with inguinal hernias who underwent hernioautoplasty using the Postempsky method. The main group consisted of 65 patients who underwent “non-tension” inguinal hernia alloplasty using the Lichtenstein method – 28 (43.1%) patients, of which 16 (24.6%) according to our modified method. Also in the main study group, laparoscopic hernioplasty – TAPP (transabdominal preperitoneal plastic surgery) was performed in 21 (32.3%) patients.The “gold standard” for the treatment of inguinal hernia is hernioplasty using the Lichtenstein method. This technique is recommended for use by the European Society of Herniology and is performed through an open access 5-10 cm long, which allows you to eliminate an inguinal hernia of any type and size.However, often the inguinal ligament is so disintegrated that it can hardly be a reliable place for fixing the prosthesis. There is a need for additional fixation. The use of the Cooper ligament for this, as recommended by many authors, only partially solves the problem, and Kozlov’s methods with the formation of an artificial inguinal ligament and Fletching using a “three-layer mesh” are technically complex.In addition, it is not always possible to observe the “no tension” principle with the Lichtenstein technique. The encountered weakness of the inguinal ligament forces, for a more durable fixation of the prosthesis, to resort to gripping part of the aponeurosis of the external oblique abdominal muscle in a continuous suture. In addition, entrapment of the Cooper ligament in the suture displaces the inguinal ligament inferiorly. As a result, suturing flaps of the aponeurosis of the external oblique abdominal muscle is impossible without tension. Even slight tissue swelling that occurs in the postoperative period leads to even greater tension in the anterior wall of the inguinal canal. Incomplete restoration of the integrity of the anterior wall of the inguinal canal, leaving a large external inguinal ring, leads to straightening of the inguinal canal and disruption of its valve function.It should also be noted that exudation arising as a result of surgical trauma and in response to the prosthesis, like a foreign body, can lead to the accumulation of fluid in the cavity of the inguinal canal, swelling of the spermatic cord and testicle. Another important thing is that the posterior wall of the inguinal canal is strengthened only due to the weakened transverse fascia and mesh implant. The mechanical load is immediately placed on the graft. There is a need to use dense “heavy” meshes, because the use of lightweight and semi-absorbable meshes with increased intra-abdominal pressure leads to separation or rupture of the mesh and, as a consequence, recurrence of the hernia. In addition, fixing the upper edge of the graft to the surface of the internal oblique abdominal muscle leads to a number of negative consequences: cutting through the sutures and migration of the mesh implant due to the low mechanical strength of the muscle tissue; to the danger of injury to muscle vessels, and in conditions of early loading - to the formation of intermuscular hematomas, suppuration of the postoperative wound; to the formation of a rough, rigid scar in place of the formed folds.Lichtenstein method in 2 (7.1%) patients observed and reoperated out of 28 patients in the late postoperative period, we found that in both cases the cause of the relapse was the separation of the muscular aponeurotic tissue, the cutting of sutures and migration of a mesh implant under mechanical load in obese patients with high intra-abdominal pressure.Taking into account all the above-mentioned disadvantages and possible complications in the postoperative period, we have developed and introduced into practice an improved “non-tension” inguinal hernia alloplasty. The objective of the proposed method in developing a safe and effective method for the surgical treatment of inguinal hernias was to strengthen the anterior and posterior walls of the inguinal canal through the proposed fixation of a mesh implant, prevent relapses and reduce postoperative complications, early activation and rehabilitation of patients.The “tension-free” inguinal hernia alloplasty we improved was carried out as follows. The skin, subcutaneous tissue and aponeurosis of the external oblique abdominal muscle were dissected according to the generally accepted technique. The hernial sac was isolated and removed or immersed in the abdominal cavity.A mesh implant measuring 10×15 cm was cut intraoperatively, taking into account the individual characteristics of the inguinal space, and plastic surgery of the inguinal canal wall was performed. For this purpose, the upper inner part of the graft was fixed between the lower edge of the transverse muscle and the transverse fascia of the abdomen with U-shaped sutures, and the middle part, by overlapping evenly with straightening the mesh without tension, was fixed to the inguinal ligament with interrupted sutures to a point located 2 cm lateral to the internal inguinal ring (Figure 1).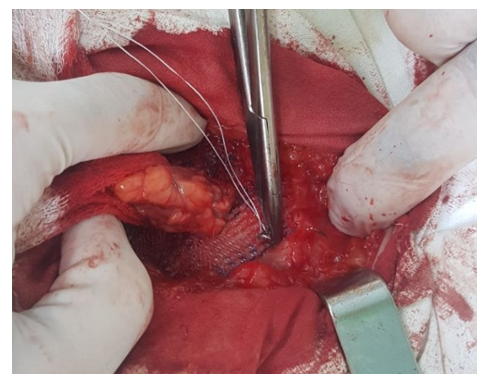 | Figure 1. Fixation of the implant to the upper wall of the inguinal canal |
Next, in the projection of the center of the internal inguinal ring, the mesh was folded with a clamp and a hole measuring 7-8 mm in diameter was cut out with scissors for the spermatic cord. The mesh was cut vertically upward from it. The spermatic cord was placed through the incision into the prepared hole. This ensured an extremely accurate comparison of the exit site of the spermatic cord and the window in the straightened mesh implant; wrinkling of the mesh and compression of the elements of the spermatic cord by the edge of the mesh implant were eliminated.The medial edge of the mesh was fixed to the aponeurosis of the rectus abdominis muscle with a continuous suture. Next, with the same thread, the upper outer part of the mesh implant was fixed with U-shaped sutures from the inside to the aponeurosis of the external oblique abdominal muscle. To do this, the upper flap of the dissected aponeurosis of the external oblique abdominal muscle was turned upward using hooks. As a result, a fold was formed from the mobilized area of the aponeurosis, resembling the Pupart ligament in appearance. After final straightening of the mesh, the excess lateral flap was excised. The aponeurosis of the external oblique abdominal muscle was sutured edge to edge. The operation was completed by suturing the subcutaneous tissue and a continuous intradermal suture. All edges were sutured with No. 3.0 Prolene thread. The stages of fixation of a composite mesh implant are depicted in Figure 2.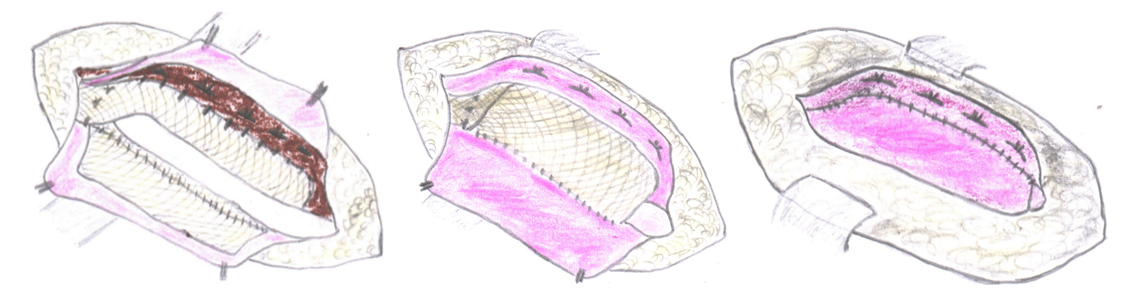 | Figure 2. Stages of performing a modified “tension-free” inguinal hernia alloplasty: a) fixation of the graft with the upper inner part between the lower edge of the transverse muscle and the transverse fascia of the abdomen using U-shaped sutures, and the middle part, by overlapping evenly with straightening the mesh without tension, to the Pupart ligament with interrupted sutures to a point located 2 cm lateral to the internal inguinal ring, the spermatic cord is located above the mesh; b) fixation with U-shaped sutures of the upper outer part of the mesh implant from the inside to the upper flap of the aponeurosis of the external oblique abdominal muscle; c) suturing the edges of the upper and lower flap of the aponeurosis of the external oblique abdominal muscle with interrupted sutures |
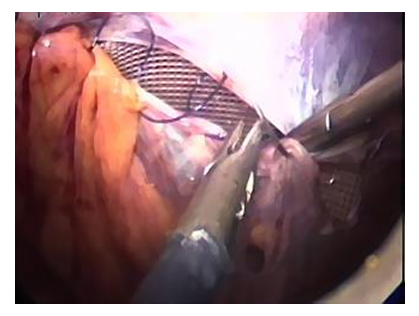
Modified method hernialloplasty of an inguinal hernia allows solving several problems simultaneously: fixing the graft to the walls of the inguinal canal by simplifying the suturing of tissue in a direction parallel to the horizontal plane, strengthening the walls of the inguinal canal and protecting the spermatic cord from possible external household injuries, preventing massive growth of connective tissue between the prosthesis and the spermatic cord, minimizing stagnation in the venous system of the spermatic cord, preventing scrotal swelling in the postoperative period, early rehabilitation of patients.Before mesh implantation, the posterior and anterior walls of the inguinal canal are strengthened by suturing the upper inner edge of the transverse abdominal muscle with the transverse fascia to the graft to prevent the risk of relapse.The method was used in 16 patients of older age groups. All patients were examined at different times after surgery. The cosmetic results of the operations are satisfactory. There was no recurrence of inguinal hernias in the operated patients.Lichtenstein plastic surgery with strengthening of the anterior and posterior walls of the inguinal canal eliminates the development of recurrent hernia, prevents scrotal swelling in the early postoperative period and is indicated in patients of older age groups with degenerative-dystrophic changes in the tissues of the inguinal region and high (ASA III - IV degree) operational and anesthetic risk.In 21 (23.3%) cases, patients with inguinal hernias of older age groups underwent laparoscopic hernioplasty - TAPP (transabdominal preperitoneal plastic surgery).TAPP technique was standard. Under general anesthesia, a 10 mm port was inserted into the abdominal cavity in the peri-umbilical area for the camera. Taking into account the presence of concomitant diseases, the level of carboxyperitoneum created was maintained in the region of 11-12 mmHg. An inspection of the abdominal cavity and the fossae of the inguinal canal on both sides was performed. Then, under laparoscope monitoring, 5 mm trocars were introduced at points along the right and left anterior axillary line. After this, from the abdominal cavity, access was created into the preperitoneal cellular space to the inguinal space, after which a peritoneal incision was made at a level of 2 cm above the inguinal space, which makes it possible, under color visualization, to accurately differentiate the vascular structures of the inguinal space from the pathology side. Then an incision was made from the internal inguinal ring to the medial fold, the length of the incision was approximately 10 cm. After this, dissection of the preperitoneal space was performed, and elements of the spermatic cord were also isolated. Using instruments, the hernial sac, pubic tubercle, and pectineal ligament were carefully isolated, while the epigastric and iliac vessels were very carefully differentiated. Next, careful hemostasis was performed, after which a mesh synthetic prosthesis was introduced through a 10 mm port installed in the abdominal cavity, which was placed in the groin space (Fig. 3). | Figure 3. Final stage. Peritonization of the endoprosthesis |
Then the mesh was fixed to the Cooper ligament and soft tissues using a herniostapler (Fig. 4). Careful control of hemostasis is considered the key point of the operation after mesh fixation, which is essentially the prevention of specific postoperative complications. Peritonization of the endoprosthesis was performed using a herniostapler. Fixation of the mesh material, as well as its peritonesis, was performed according to the recommendations, bypassing the danger triangle area in order to prevent the development of serious complications (Fig. 5). Upon completion of the control revision of the abdominal cavity and dessufflation, layer-by-layer suturing of the trocar wounds was performed. The muscular aponeurosis was sutured only in a 10 mm hole located above the navel. | Figure 4. Final stage. Peritonization of the endoprosthesis |
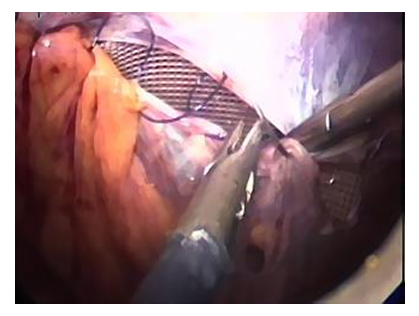 | Figure 5. Final stage. Peritonization of the endoprosthesis |
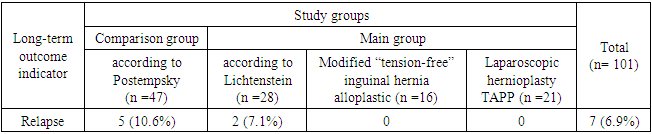
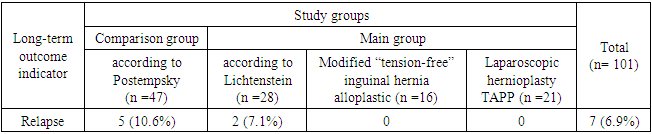
Laparoscopic hernioplasty using the TAPP method is characterized by low trauma, early rehabilitation, and better quality of life results. However, the presence of severe comorbid pathology (surgical and anesthetic risk grade III - IV according to ASA) limits its use (32.3% performed) in elderly and senile patients. Due to the need to create a tense carboxyperitoneum.Long-term results were analyzed in 101 (90.2%) of 112 patients who underwent inguinal hernioplasty. To assess long-term results, patients underwent a thorough questionnaire, outpatient and inpatient examination. Long-term results were studied over a period of 1 to 5 years. At the same time, the fate of 82.3% was traced for a period of more than 3 years, sufficient for the final formation of a clinically significant relapse of the disease.Of 101 patients examined in the long term, recurrence of the inguinal hernia was noted in 7 (6.9%), while in the comparison group this figure was 10.6% (5 patients), and in the main group – 3.1% (2 patients) (Table 3).Table 3. Recurrence rate of inguinal hernia
 |
| |
|
As can be seen from Table 3, due to the use of a mesh implant, it was possible to minimize the frequency of recurrence of inguinal hernia from 10.6% to 8.7%, and when fixing the mesh implant simultaneously to the anterior and posterior walls of the inguinal canal and with laparoscopic TAPP hernioplasty in the late postoperative period, allowed cases of relapse to be reduced to zero.According to the program for determining the quality of life of patients who underwent inguinal hernioplasty, 101 (90.2%) of 112 patients observed in the long-term postoperative period were assessed. After “tension” inguinal hernia autoplasty, excellent results were obtained in 31.7% of patients, good in 40.6%, satisfactory in 17.1% of patients and unsatisfactory in 10.6% of cases. In turn, in the main group, excellent results were obtained in 55.0% of 60 patients, good in 35.0%, satisfactory in 6.6% of patients and unsatisfactory in 3.1% of cases.
5. Conclusions
The choice of inguinal hernioplasty method in patients of older age groups with competing comorbid pathologies should be individualized and based on clarification of surgical and anesthetic risk factors, as well as the type of hernia, the condition of the posterior wall of the inguinal canal and pathological changes in the tissues of the inguinal region. Lichtenstein plastic surgery with strengthening of the anterior and posterior walls of the inguinal canal eliminates the development of recurrent hernia, prevents scrotal swelling in the early postoperative period and is indicated in patients of older age groups with degenerative-dystrophic changes in the tissues of the inguinal region and high (ASA III - IV degree) operational and anesthetic risk. Laparoscopic hernioplasty using the TAPP method is characterized by low trauma, early rehabilitation (reduction of treatment time by 2 times), and better quality of life results. The presence of severe comorbid pathology (surgical and anesthetic risk grade III - IV according to ASA) limits its use (32.3% performed) in elderly and senile patients. An individualized approach to the surgical treatment of inguinal hernias in elderly and senile patients made it possible to reduce the frequency of specific long-term postoperative complications - hernia recurrence from 10.6% in the comparison group to 3.1% in the main group.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
References
| [1] | Abdurakhmanov D. S., Rakhmanov Q. E., Davlatov S. S. Criteria for choosing surgical treatment of patients with ventral hernias and obesity // Electronic Innovation Bulletin. – 2021. – №. 7. – С. 57-67. |
| [2] | Abduraxmanov D. S. H. et al. Criteria for choosing surgical treatment of patients with ventral hernias and obesity //International Journal of Pharmaceutical Research (09752366). – 2020. – Т. 12. – №. 3. |
| [3] | Belokonev V.I., Kovaleva Z.V., Pushkin S.Yu. Anterior prosthetic hernioplasty using a combined method for large and giant ventral hernias // Surgery. Journal named after NI Pirogov. – 2018. – No. 5. – pp. 45-50. |
| [4] | Davlatov S. S. Ways to Eliminate Postoperative Complications after Ventral Hernia Repair in Patients with Morbid Obesity. American Journal of Medicine and Medical Sciences 2017, 7(3): 147-150. DOI: 10.5923/j.ajmms.20170703.07. |
| [5] | Khakimov M. Sh. et al. Advantages of minimally invasive technologies in the surgical treatment of umbilical hernias // Endoscopic surgery. – 2017. – T. 23. – No. 4. – pp. 29-32. |
| [6] | Khujamov O. B., Davlatov S. S. An Improved Method of Non-Tension Hernioplasty for Inguinal Hernias. American Journal of Medicine and Medical Sciences 2023, 13(8): 1114-1117. DOI: 10.5923/j.ajmms.20231308.17. |
| [7] | Kurbaniyazov Z. B., Mardanov B. A., Davlatov S. S., Rakhmanov K. E. Justification of Simultaneous Operations on the Organs of the Abdominal Cavity and Abdominal Wall in Patients with Ventral Hernia. American Journal of Medicine and Medical Sciences 2020, 10(8): 563-566. DOI: 10.5923/j.ajmms.20201008.05. |
| [8] | Nasirov M. Ya. et al. Analysis of long-term results of simultaneous hernioallo- and abdominoplasty in patients with postoperative ventral hernias and obesity // Surgery. Journal named after NI Pirogov. – 2015. – No. 2. – pp. 70-74. |
| [9] | Nazirov, F.G., Turakulov, U.N., Akbarov, M. M., Saatov, R.R. The use of minimally invasive methods for correcting iatrogenic damage to the extrahepatic bile ducts and external bile fistulas // Endoscopic surgery. – 2018. – T. 24. – No. 5. – pp. 7-9. |
| [10] | Nazyrov F. G. et al. Age-related structural changes in aponeuroses of the rectus abdominal muscles in patients with postoperative ventral hernias // Клінічна та yeкспериментальна патологія. – 2018. – Т. 17. – №. 3. |
| [11] | Sayinaev F. K. et al. Endovideosurgical preaperitoneal prosthetic hernioplasty in ventral hernias // International Journal of Medical Sciences and Clinical Research. – 2023. – Т. 3. – №. 05. – С. 5-15. |
| [12] | Sayinaev F. K. et al. Modified method for laparoscopic hernioalloplasty in vental hernias //British Medical Journal. – 2023. – Т. 3. – №. 3. |
| [13] | Sayinayev F. K. et al. Laparoscopic treatment of incisional ventral hernias // 湖南大学学报 (自然科学版). – 2021. – Т. 48. – №. 7. – С. 143-149. |
| [14] | Shamsiyev A. M., Davlatov S. S. Method of surgical treatment of ventral hernias in patients with concomitant obesity. Hospital Surgery // Journal Named by L. Ya. Kovalchuk. – 2016. – Т. 1. – С. 78-83. |





 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML