-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 227-230
doi:10.5923/j.ajmms.20241402.13
Received: Jan. 7, 2024; Accepted: Jan. 31, 2024; Published: Feb. 4, 2024

Optimization of Technical Aspects of Endovideo Surgery for Combined Abdominal Pathology
Batirov Bekhzod Aminjanovich, Babajanov Akhmadjon Sultanboyevich
Samarkand State Medical University, Uzbekistan
Correspondence to: Batirov Bekhzod Aminjanovich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Presented results of treatment of 227 patients operated on in the period 2017-2021, for whom endovideosurgical technologies were used as a priority in the surgical correction of a ventral hernia and concomitant surgical pathology of the abdominal organs. When the concomitant abdominal pathology is located at a remote distance from the hernia defect, priority is given to performing the simultaneous stage using laparoscopic technology, which was successfully performed in 37.5% of patients, i.e. in more than 1/3 of patients in the main group. Optimization of the tactical and technical aspects of simultaneous surgical correction of ventral hernias and concomitant abdominal pathology with the priority use of endovideosurgical technologies made it possible to reduce the frequency of postoperative complications from 8.6% to 5.3%, and reduce the duration of the operation from 72.5 ± 3.4 minutes. up to 58.5±4.1 min. and reduce the duration of inpatient treatment from 10.2±0.4 to 8.3±0.6 bed days. At the same time, curing a patient from several surgical diseases within the framework of one anesthesia and surgical intervention justifies the need for simultaneous operations.
Keywords: Simultaneous operations, Endovideosurgery
Cite this paper: Batirov Bekhzod Aminjanovich, Babajanov Akhmadjon Sultanboyevich, Optimization of Technical Aspects of Endovideo Surgery for Combined Abdominal Pathology, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 227-230. doi: 10.5923/j.ajmms.20241402.13.
Article Outline
1. Introduction
- According to Nazirov F.G. (2018) [2,8,12,15], combined surgical pathology is present in 20-30% of surgical patients. Of these, only up to 6-8% of cases undergo simultaneous correction, i.e. simultaneous surgery. The reserved attitude of surgeons towards simultaneous operations is explained by the lack of consensus on the indications and contraindications for them, and insufficiently studied results. In the few scientific articles devoted to this problem, little attention is paid to such important indicators as the duration of the simultaneous operation, features of the postoperative period and a number of other factors characterizing the severity of the surgical injury [1,5,6,9,13,16].Recently, the problems of abdominal surgery and herniology have been significantly revised in connection with the development and introduction into clinical practice of new minimally invasive laparoscopic methods of surgical treatment, performed under the control of modern instrumental tracking methods. They, according to a number of enthusiasts, are designed to practically eliminate or at least sharply reduce the use of laparotomy operations [3,4,7,10,11,14].
2. Purpose of the Study
- Improving the results of surgical treatment of patients with combined abdominal pathology by optimizing the tactical and technical aspects of a one-time simultaneous operation with the priority use of endovideosurgical technologies.
3. Material and Research Methods
- The study included the results of treatment of 227 patients operated on in the period 2017-2021, for whom endovideosurgical technologies were used as a priority in the surgical correction of a ventral hernia and concomitant surgical pathology of the abdominal organs.In all patients, the main surgical disease was a ventral hernia. A total of 334 concomitant surgical pathologies were identified, with some patients having two or more. Among them, adhesive disease of the abdominal cavity prevailed 106 (46.7%), obesity grades III and IV. with a saggy abdomen was present in 67 (29.5%) patients, cholelithiasis - in 69 (30.1%) patients, cysts of the liver and pancreas in 13 (5.7%) patients, in 19 (8.4%) patients had surgical pathology of the anterior abdominal wall (ligature fistulas and pseudocysts of the anterior abdominal wall), pathology of the pelvic organs in women 70 (30.8%).It should be noted that in patients with an increase in the size of the hernia, the frequency of concomitant surgical pathology of the anterior abdominal wall and abdominal organs increased proportionally - with W3 59.6%, W4 -66.3%.Simultaneous pathology was diagnosed preoperatively in 74.6%, intraoperatively in 25.4%.Of those examined, 62.8% of patients had various concomitant somatic diseases of vital organs. Of these, 41.9% of patients had two or more concomitant somatic diseases. Taking into account the ASA classification, 53.7% of patients were classified as class II, and 9% of patients were classified as class III.Computed tomography was performed in 58 (25.9%) patients. The method made it possible to verify the presence of simultaneous pathology of the abdominal organs and identify defects in the topography of the anterior abdominal wall.
4. Results and Its Discussion
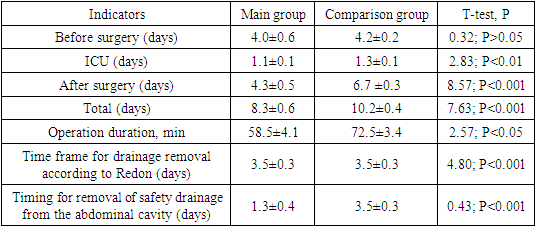
- Since in all patients the main pathology was a ventral hernia, and the simultaneous pathology was a surgical disease of the abdominal organ, when choosing a surgical approach, the location of the hernial orifice was first taken into account, then the location of the organ with the simultaneous pathology in the abdominal cavity.In 46 (20.3%) patients with ventral hernias and simultaneous pathology of the abdominal cavity, both stages of the operation were performed from laparoscopic approaches using EVS. These patients underwent stage 1 LCE in 19 cases, supravaginal amputation or hysterectomy for fibroids was performed in 11 patients, ovarian cystectomy in 7 patients, fenestration of cysts from the liver in 2 patients, and adhesiolysis in 27 patients due to adhesive disease of the abdominal cavity and chronic intestinal obstruction. The 2-stage operation was completed with laparoscopic hernioplasty.In 39 (17.6%) patients at stage 1, simultaneous pathology was corrected laparoscopically, the main stage of the operation - hernialloplasty - was performed through a herniolaparotomy approach. In this case, 23 patients underwent LCE, supravaginal amputation of the uterus for uterine fibroids - 1, ovarian cystectomy - 4, in 1 case a cyst was removed from the liver, 14 patients were subjected to adhesiolysis.Thus, out of 227 patients, laparoscopic correction of both the main and simultaneous pathology was performed in 46 (20.3%), endovideosurgical correction of simultaneous pathology was performed in 39 (17.6%), i.e. when the simultaneous pathology is located at a wide distance from the hernia defect, simultaneous stages of the operation using laparoscopic techniques were performed in 85 (37.5%) patients, more than 1/3 of the patients. At the same time, in 142 (62.6%) patients, both stages of the operation were performed using a herniolaparotomy approach. The reason for this was the proximity of the pathology of the abdominal organs to the hernia defect. 67 (29.5%) patients of the main group who had concomitant pathology in the form of obesity II - III degree. After completion of the anterior abdominal wall plastic surgery, dermatolipidectomy was performed.Laparoscopic prosthetic hernioplasty for ventral hernias was used in 46 patients of the main group (20.3%), in the presence of small and medium hernias, with the corresponding sizes of the aponeurosis defect - up to 5 cm and from 5 to 10 cm using polypropylene implants using the "Ipom" method (Laparoscopic Intra Peritoneal Onlay Mesh). The trocar insertion sites were standardized and chosen where it was more convenient and safer after the simultaneous stage of the abdominal surgery.34 (73.3%) of 46 patients underwent laparoscopic prosthetic hernia repair using standard polypropylene mesh implants; in 12 (26.7%) composite mesh implants “Physiomesh” or “Prosid” (Ethicon) were used.When using standard implants in the abdominal cavity, the peritoneum was opened, the hernial sac was isolated and a “pocket” was created in the preperitoneal space, with a distance of 5-6 cm along the perimeter from the hernial orifice. Next, a mesh implant rolled into a tube was inserted into the abdominal cavity through a trocar, unfolded and placed into the created preperitoneal “pocket”. It was pressed against the anterior abdominal wall using ligatures tied along the edges of the implant. The implant was sutured to the anterior abdominal wall using a modified Endo Close needle.The use of composite mesh implants “Physiomesh” or “Prosid” (Ethicon) in 12 (26.7%) patients avoided the need to create a preperitoneal “pocket” before fixing the prosthesis to the anterior abdominal wall.To assess the effectiveness of treatment results for patients in the compared groups (the main group, where simultaneous operations were performed using EVH, the comparison group, where simultaneous operations were performed using laparotomy access), the following parameters were used as the main criteria: - abdominal complications of the early postoperative period; - extra-abdominal complications early postoperative period; - wound complications in the early postoperative period.In the comparison group, compartment syndrome was observed in 2 (1.9%). On a comparative basis, the number of complications showed uniform indicators in both groups of patients (Criterion χ 2 =4.043; Df=1; p=0.045). When considering time periods, it was noted that the improvement of tactical and technical aspects ensured a reduction in all main perioperative periods (Table 1).
|
5. Conclusions
- When the concomitant abdominal pathology is located at a remote distance from the hernia defect, the priority is to perform a simultaneous stage using laparoscopic technology, which was successfully performed in 37.5% of patients, i.e. in more than 1/3 of patients in the main group. Endovideosurgical hernialloplasty is methodologically justified and effective in the surgical treatment of ventral hernias of small (W 1) and medium (W 2) sizes, which was used in 20.3% of cases. Improving aspects of laparoscopic hernia alloplasty using composite mesh implants, as well as the use of a modified Endo needle at the stage of prosthesis fixation Close with extracorporeal knot tying greatly simplified the surgical technique. Optimization of the tactical and technical aspects of simultaneous surgical correction of ventral hernias and concomitant abdominal pathology with the priority use of endovideosurgical technologies made it possible to reduce the frequency of postoperative complications from 8.6% to 5.3%, and reduce the duration of the operation from 72.5 ± 3.4 minutes. up to 58.5±4.1 min. and reduce the duration of inpatient treatment from 10.2±0.4 to 8.3±0.6 bed days. At the same time, curing a patient from several surgical diseases within the framework of one anesthesia and surgical intervention justifies the need for simultaneous operations.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML