-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 224-226
doi:10.5923/j.ajmms.20241402.12
Received: Jan. 9, 2024; Accepted: Feb. 2, 2024; Published: Feb. 4, 2024

Markers of Liver Damage in Respiratory Allergies in Children
Matniyozova Zaynab Tuxtaboyevna, Xodjayeva Nafisa Abayevna
Bukhara State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Bronchial asthma and respiratory allergies in children are an urgent problem for many countries and its medical and social significance is currently increasing. The article is devoted to the study of the optimal method for diagnosing liver pathologies in respiratory allergies in children, which is very important when organizing a specialized pediatric and allergological service. The proposed method allows early diagnosis and prevention of liver damage in children with respiratory allergies.
Keywords: Children, Respiratory allergy, Diagnosis, Immunity, Liver damage
Cite this paper: Matniyozova Zaynab Tuxtaboyevna, Xodjayeva Nafisa Abayevna, Markers of Liver Damage in Respiratory Allergies in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 224-226. doi: 10.5923/j.ajmms.20241402.12.
Article Outline
1. Introduction
- Globally, it is generally recognized that in most industrialized countries, the three main forms of allergic diseases – asthma, rhinitis and atopic eczema – individually or in various combinations affect up to 20% of the population [3]. Allergic diseases are among the most common in children, and in recent years there has been a significant increase in the frequency and more severe course of allergic diseases, in connection with which they are considered in modern society as a major medical and social problem. The frequency of allergic diseases, according to different authors, varies widely, depending on the diagnostic criteria used and methods of epidemiological research [5]. Thus, the prevalence of bronchial asthma (BA), according to domestic and foreign authors, ranges from 0.2 to 8.1%. According to the generalized data of the ISAAC study (International Study of Asthma and Allergies in Childhood - International Study of Asthma and Allergies in children), the frequency of asthma symptoms ranges from 1.0 to 30.8% [1,4]. Allergic rhinitis and pollinosis in different regions account for 0.2-20%, atopic dermatitis and eczema - 1.6-4.2% [2].Allergic rhinitis (AR) is one of the most common human diseases affecting from 10 to 50% of the general population. In Russia, from 12 to 24% of the population suffers from allergic rhinitis and more than 600 million people in the world. The widespread, widespread increase in morbidity, the negative impact on the quality of life of patients and the cost of therapy define AR as a medical, social and economic problem [7].Pollinosis is a frequently registered allergopathology in Uzbekistan (185.95 per 100,000 population), characterized by a 10.4% increase in morbidity over the period 2007-2014. Pollinosis is a risk factor for the formation of bronchial asthma (BA) and precedes its development in 32-64% of cases [6]. Allergic diseases, in particular asthma, also remain an urgent problem in our region. In Uzbekistan, the prevalence of asthma per 1000 population is 4.6 and, according to this indicator, the Republic ranks 19th globally. Among allergic diseases, BA is one of the most common. According to epidemiology data, over the past 10 years, 4-10% (about 300 million people) of the world's population have suffered from this disease. BA is widespread in all countries of the world to varying degrees, due to factors such as climate, geographical location, flora, degree of air pollution, urbanization and the level of culture of the population [8].The aim of the study development of a method for diagnosing liver damage in respiratory allergies in children and a program for its prevention.
2. Materials and Methods of Research
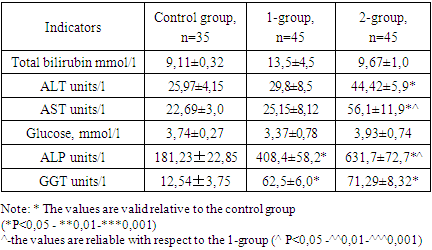
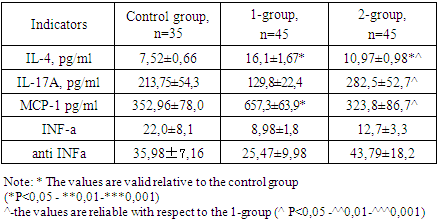
- The study was conducted on the basis of the Department of Allergology and Gastroenterology of the Bukhara Regional Multidisciplinary Medical Center in the periods 2019-2023. Of all the examined (125) aged 2 to 17 years, 45 patients suffering from bronchial asthma (BA), (group 1), 45 patients suffering from respiratory allergosis (RA), (group 2) were selected. The control group consisted of 35 healthy children of the appropriate age (group 3).All children (125) selected for examination underwent general and biochemical blood tests (glucose, ALT, AST, total bilirubin, alkaline phosphatase (alkaline phosphatase), gammaglutamintranspeptidase (GGT), determination of immunoglobulin E, IL-4, IL-17A, MCP-1, INF-a and anti-INF-blood test, blood test for allergenic panels and ultrasound of the liver.
3. Results and Discussion
- The study of hepatic transaminases in respiratory allergies allowed to establish an increase in ALT and AST in group 2 patients to 44.42±5.9 u/l and 56.1±11.9 u/L, against the control -25.97±4.15 u/l and 22.69±3.0 u/l, respectively (p<0.005), Table 1.
|
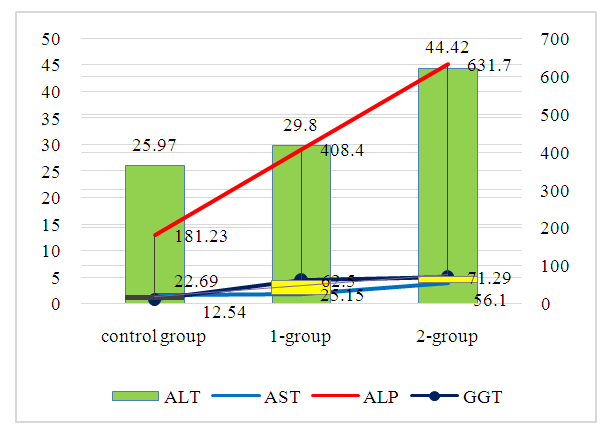 | Figure 1. Markers of liver damage in respiratory allergies in children |
|
4. Conclusions
- 1. It was found that BA in children occurs against the background of anemia and relative lymphocytopenia, there is an increase in the level of alkaline phosphatase by 2.25 times, GGT by 5.0 times, IL-4 by 2.2 times, MCP-1 by 1.86 times than in respiratory allergoses (rhinitis, conjunctivitis, bronchitis).2. RA is characterized by a course against the background of anemia and relative leukocytosis, an increase in ALT by 1.5 times, AST by 2.23 times, ALP by 3.5 times, GGT by 5.73 times, IL-4 by 1.5 times, IL-17A by 2.2 times, the degree of reactivity to allergens of house dust by 1.37 times (P<0.001), to a mixture of meadow grasses - 2.5 times (P<0.05), to a mixture of weeds - 2.88 times (P<0.001), to a mixture of food products - 1.42 times than in bronchial asthma.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML