О. K. Jalolov
Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: О. K. Jalolov, Andijan State Medical Institute, Andijan, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
According to the Global Cancer Observatory, in recent decades, about 400 thousand primary patients diagnosed with bladder cancer have been identified, and in 2020 the number of patients registered with bladder cancer has already reached 573.3 thousand (3% of all cancer cases). Men are much more likely to suffer from this cancer pathology and the ratio is approximately 1:9. In the overall structure of cancer incidence in 2020, breast cancer took 17th place in women and 6th place in men. This pathology caused death in 212.5 thousand patients in 2020, and the mortality rate per 100 thousand men was 3.3 cases and 0.9 cases in women. Invasive bladder cancer is a cancer that is becoming increasingly common among men. Radical cystectomy is widely used as the primary treatment for this type of tumor. In order to improve the quality of life of patients, which is no less important than the survival rate, specialists in modern practical oncology have introduced more than 46 types of urine diversion into practice in the period after such highly traumatic operations. Complications after these operations and the problem of their elimination also remain relevant.
Keywords:
Radical cystectomy, Complications, Invasive bladder cancer, Neocystoplasty, Studer orthotopic neobladder, Hautmann orthotopic neobladder ileal conduit
Cite this paper: О. K. Jalolov, Review of Standard and Advanced Surgical Treatments for Invasive Bladder Cancer, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 212-219. doi: 10.5923/j.ajmms.20241402.10.
1. The Urgency of the Problem
In modern applied Oncology, the main method of treating locally malignant tumors is surgical treatment. In 2015, more than 80% of patients diagnosed with a primary malignant tumor of 15.2 million people are addicted to surgical treatment. According to the Global Cancer Observatory, the primary with the diagnosis of a malignant tumor of the urinary bladder on Earth is recorded about 400 thousand, and by 2020 it claimed that this figure had reached 573.3 thousand. Urinary bladder cancer accounted for 3% of the total oncological structure. The main and standard treatment for bladder muscle invasive cancer is the practice of radical cystectomy. Despite the fact that in recent times the frequency of complications of this type of high-tech operas has come to a minimum, in some cases these indicators remain high [1-3]. In general, the most common intraoperational complications of this type of practice are bleeding, damage to blood vessels and adjacent organs, while early postoperation – injury infection, intestinal obstruction (dynamic and mechanical), anastomosis insufficiency, peritonitis, leaky wounds and cardiovascular diseases are noted [2,4-5]. In the late 20th century, death after this type of diagnosis was observed in 2.4-15%, while early complications were observed in 28-42% of cases [6-8]. Despite the decrease in mortality rates to date, the frequency of early complications remains high (11-68%) [9].In recent years, in the treatment of muscle invasive bladder cancer, the practice of radical cystectomy, with urine derivation into the ileum (Bricker), is standard. Bricker operation-surgical removal of the urinary bladder and 15-20 cm of the ileum is separated, both ureters are connected to the proximal part, and the distal part is pulled out to the skin of the iliac region (urostoma). Orthotopic neocystoplasty - 65 cm is separated from the ileum while preserving the blood supply, and a reservoir is formed in a J, W-shaped form, both ureters are connected to the distal part, and a ureteroileal anastomosis is placed in the proximal part, leaving the Foley catheter and it is removed on the 10th day after the operation. The main goal of this type of practices performed on such patients is considered to improve their quality of life. This criterion is also important in addition to survival in the lives of patients who have undergone a cystectomy due to bladder cancer [10-12].
2. Materials and Methods
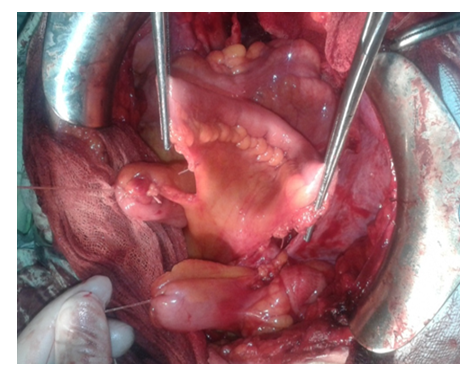
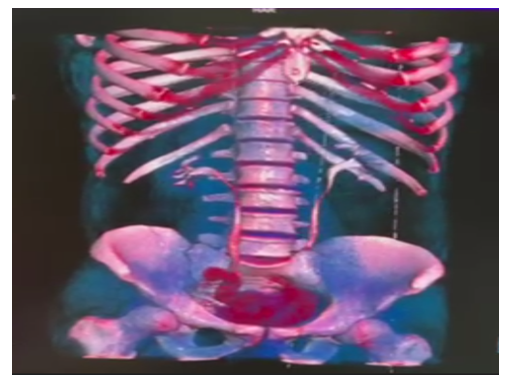
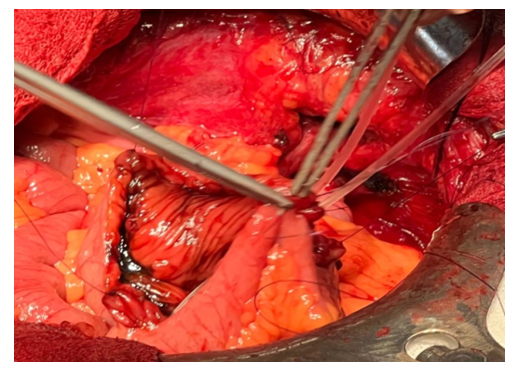
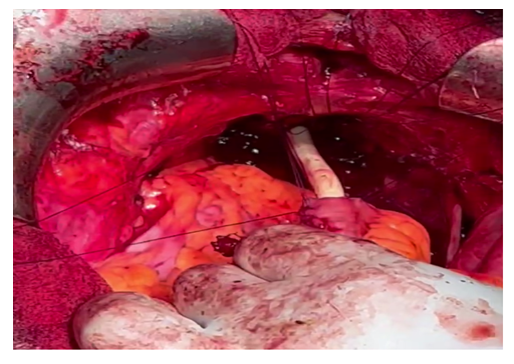
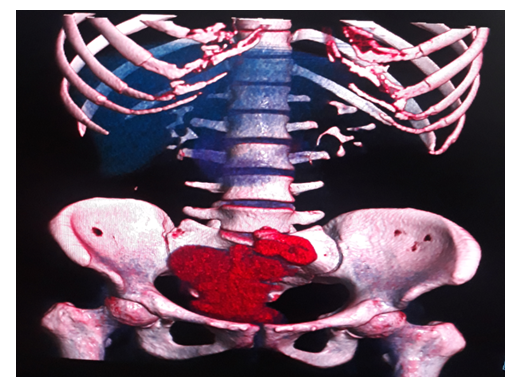
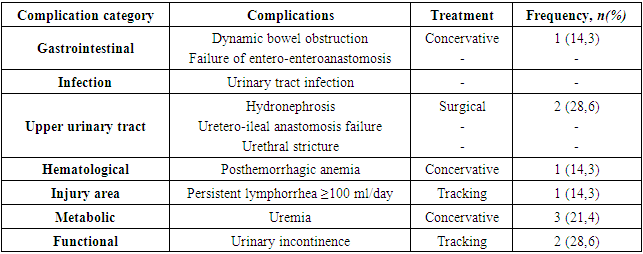
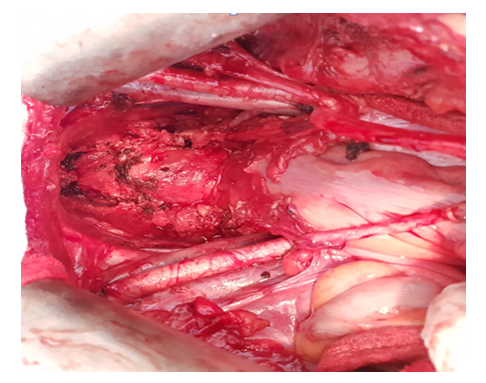
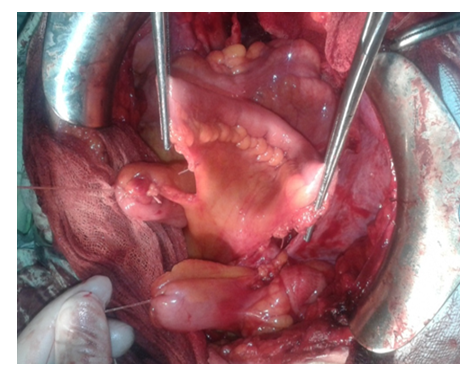
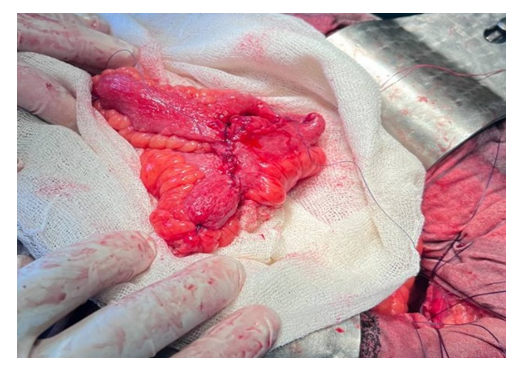
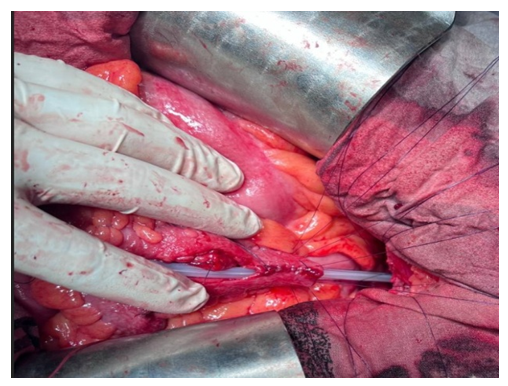
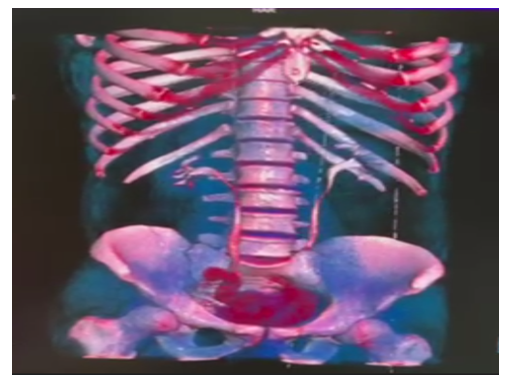
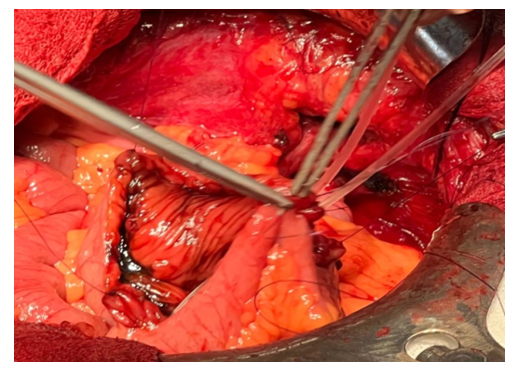
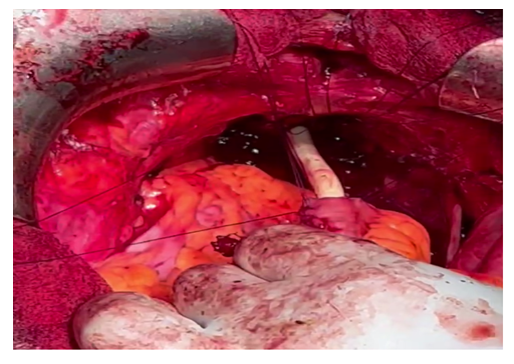
In the period from November 2017 to March 2023, 63 patient data were studied at the Andijan regional branch of the Republican specialized Scientific Applied Medical Center of oncology and radiology, which diagnosed urinary bladder muscle invasive cancer and performed cystectomy, neosystoplasty. 19 (30,2%) patients underwent radical cystectomy with bilateral ureterocutaneostomy(Group 1), 23 (36,5%) underwent Bricker(Group 2) (Figure 1-4), Studer for 14 (22,2%) patient(Group 3) (Figure 5-8), and Hautman neocystoplasty for 7 (11,1%) (Group 4) (Figure 9-12). All patients were divided into 4 groups respectively. The average age of patients who were analyzed was 62 (39-78), and in terms of the stage of the disease, the groups were in a consistent way. The duration of the practice performed in our study (minutes), intra - and postoperational complications, re-hospitalization (within 10-30 days) and the duration of treatment at the hospital (in the intensive and general surgery department) were studied and evaluated.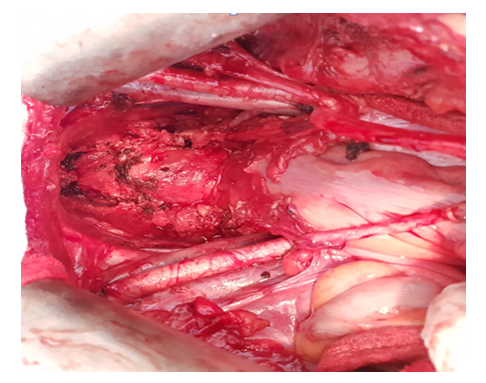 | Figure 1. Place of operation after radical cystectomy |
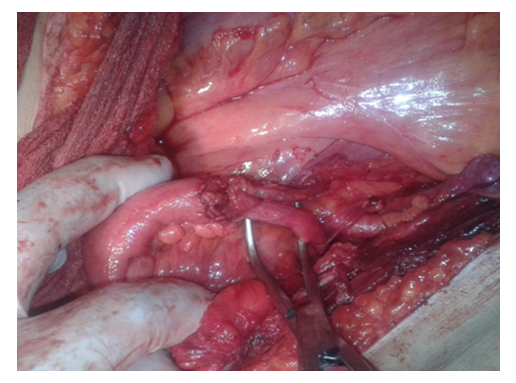
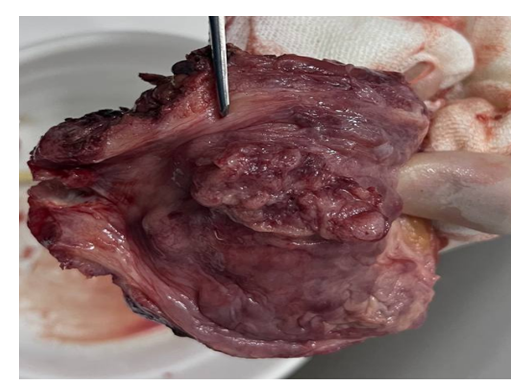
 | Figure 2. Mobilized ileal conduit |
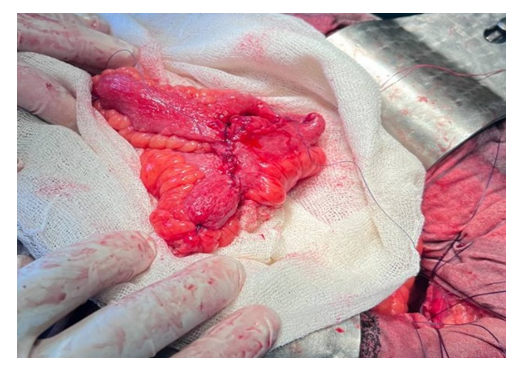
 | Figure 3. Ureteroileal anastomosis |
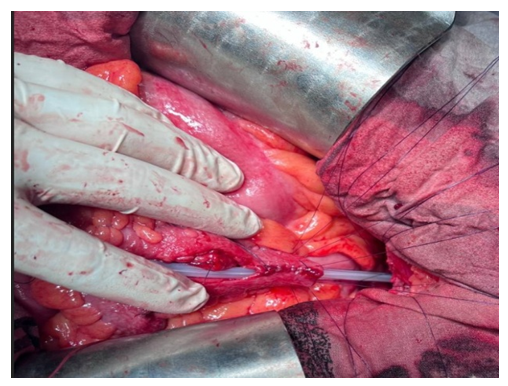
 | Figure 4. A urostomy removed in the right iliac region (after 1 month) |
 | Figure 5. Complete one-line enteroenteroanastomosis |
 | Figure 6. J-shaped reservoir according to Studer |
 | Figure 7. Reservourethral anastomosis stage |
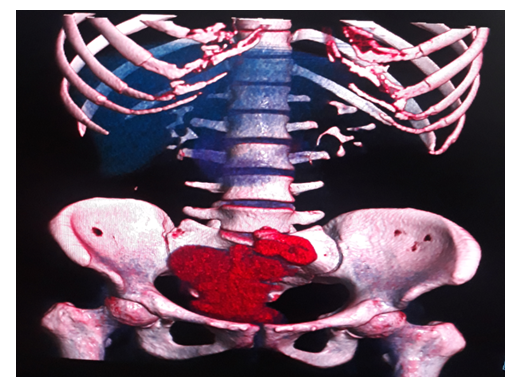
 | Figure 8. CT view of the reservoir after 3 months |
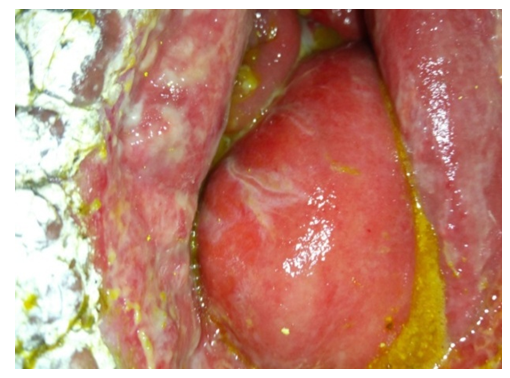
 | Figure 9. Reservoir formation stage |
 | Figure 10. Reservourethral anastomosis stage |
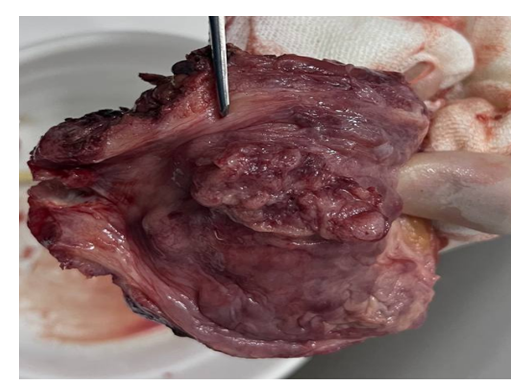 | Figure 11. Removed urinary bladder |
 | Figure 12. CT view of the reservoir after 3 months |
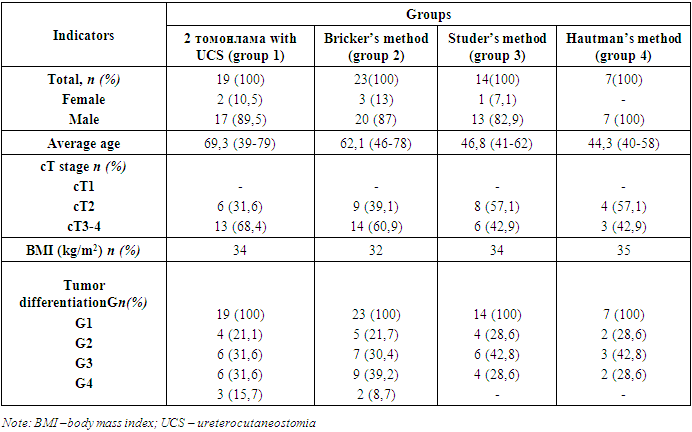
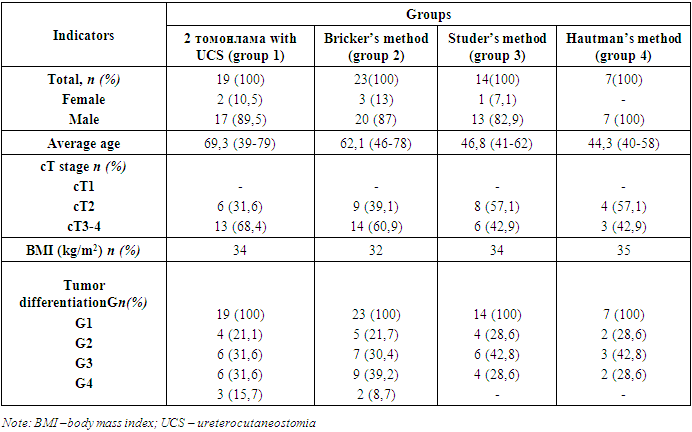
In the Study, 6 of them (9.5%) were female and 57 (90.5%) were male, according to the gender estimates of a total of 63 patients who performed operative treatment in the conditions of the Andijan regional branch (Table 1). In the group view, this was described as follows: in Group 1, women were 10.5%, men were 89.5%; in Group 2, women were 13%, men were 87%; in Group 3, women were 7.1%, men were 82.9%; in Group 4, women were not recorded. The median age of patients diagnosed was 62.3, compared to 69.3 (49-79) in Group 1, 62.1 (46-78) in Group 2, 46.8 (41-62) in Group 3, and 44.3 (40-58) in Group 4. in the st category taxile, not all groups had ST1 States. Among patients of Group 1 and 2, St3-4 was detected in most cases and accounted for 68.4 and 60.9% respectively. This showed 42.9% in Group 3 and 4. The body weight index (TVI) was proportional (32-35) in all groups. When tumor differential was studied, the main discrepancy among the groups was found only in the G4 case: 15.7% in Group 1, 8.7% in Group 2, not recorded in groups 3 and 4. The surgeries performed to all of the patients in the study were performed by two surgeons in an open manner (J.O. and D.M.). In patient anamnesis, no patient received specific treatment (radio and chemotherapy).Table 1. Patient characteristics
 |
| |
|
Patients were examined on the basis of the standard established by the Ministry of health of the Republic of Uzbekistan (2021) in the pre-operative period: physical examination, rectal examination with a finger, routine urine and blood test, biochemical blood test (protein, urea, creatinine), cystoscopy with biopsy, urinary bladder USG, MRI examination of small pelvic organs, excretory urography, chest X-ray, bone scintigraphy if suspected of metastatic change in the bone system.Complications in the 30-90–day period after tashrix were assessed based on the Clavien-Dindo modified classification. The follow-up period of patients was sufficient to assess the complications and condition of the post-dental period.Indicators during surgery (intraoperative) included the frequency of injury to the neighboring organs, volume of blood loss, plasma - and hemotransfusion. During the early period after the surgery, measures such as the assessment of the effect of the practice transferred to the duration of treatment in intensive care and intensive care units, the frequency of re-hospitalization and operative treatment, the restoration of intestinal activity were evaluated.
3. Results and Discussions
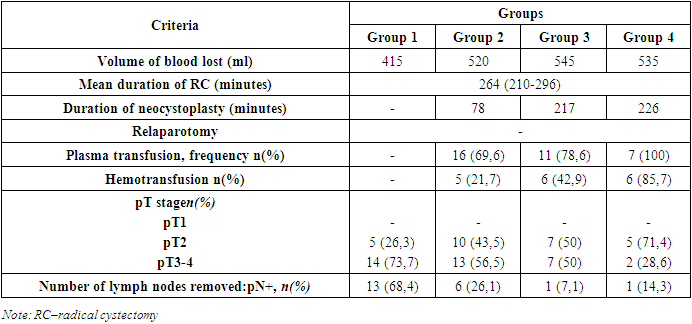
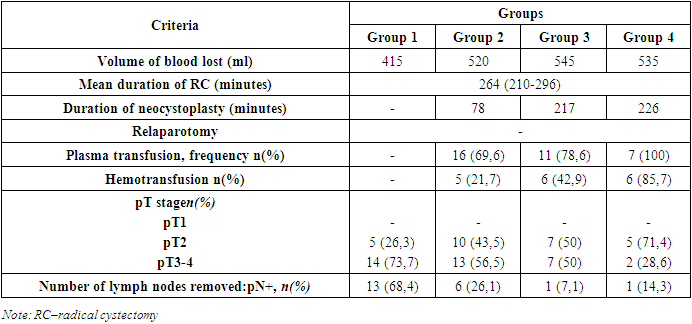
When the intraoperational indicators of the carried out operations were performed, the average volume of blood loss in group 1 was 415 ml, group 2 was 520 ml, group 3 was 545 ml and group 4 was 535 ml (Table 2). No plasma-hemotransfusion treatment was performed on group 1 patients. 16 (69.6%), 11 (78.6%) and 7 (100%) patients in the 2-3-4 group, respectively, received plasma transfusions. After these types of operations, plasma transfusion was performed to help the healing of entero-entero, entero-ureteral and entero-urethral anastomoses. Hemotransfusion was performed on all patients who underwent neocystoplasty. This indicator was 5 (21.7%) 6 (42.9%) 6 (85.7%) in group 1-2-3 patients. The average duration of radical cystectomy (RC) was 264 (210-296) minutes. The duration of neocystoplasty was 78 minutes in group 2, 217 minutes in group 3, and 226 minutes in group 4. In patients of groups 3-4, the duration of the first plastic surgery was extended to 340 minutes, but this indicator decreased significantly (160-215 minutes) in the subsequent examinations.Table 2. Intra-perioperative and pathomorphological indicators
 |
| |
|
According to the standard of diagnosis and treatment of oncology patients established by the Ministry of Health of the Republic of Uzbekistan (RIORIATM prof. Tillyashaykhov M.N. 3rd edition), G3/HG patients in the T1 category recommended by RC were not identified in any group, and pT2 stage 1-2-3- 5 (26.3%), 10 (43.5%), 7 (50%), 5 (71.4%) patients of group 4 respectively. The main reason for the higher percentage of pT2 stage and LG in groups 3 and 4 is the selection of patients in this category for better survival rate and quality of life after this type of highly technologically complex operations. The pT3-4 stage analysis was as follows: Group 1 - 14 (73.7%), Group 2 - 13 (56.5%), Group 3 - 7 (50%) and Group 4 - 2 (28.6%). When analyzing pN+ in patients, the percentage of this category was significantly higher in group 1 patients and made up 68.4% of patients. In groups 2-3-4, this indicator showed 6 (26.1%), 1 (7.1%) and 1 (14.3%), respectively. The pN+ stage and post-test lymphorrhea were directly proportional to each other.Table 3. Postoperative indications and complications
 |
| |
|
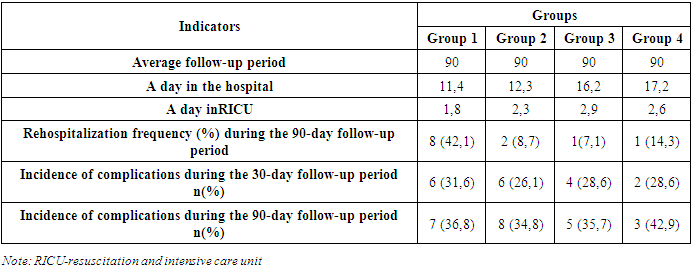
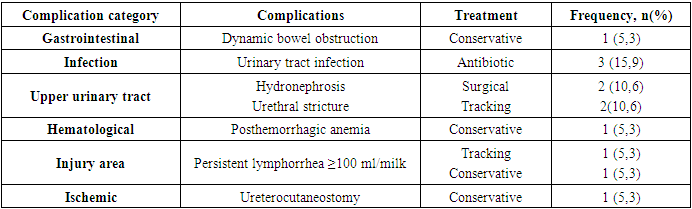
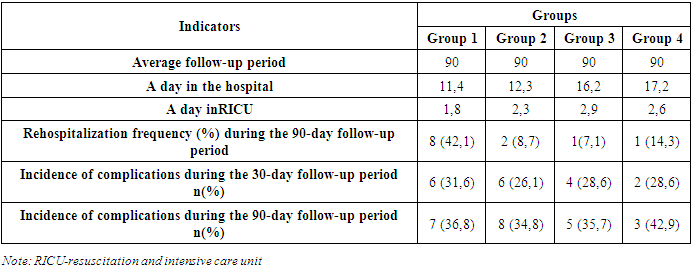
All patients who underwent surgery with the diagnosis of invasive bladder cancer were followed up for 90 days to assess the complications of the diagnosis. According to the analysis of inpatient treatment days, group 1 was 11.4 days, group 2 was 12.3 days, group 3 was 16.2 days, and group 4 was 17.2 days. The main reason for a longer hospital stay in patients of groups 3 and 4 is that the procedure for removing the catheter from the reservoir and the kidney stent is performed on the 10th day after the examination. Analysis of days treated in ICU is as follows: Group 1 showed 1.8 days, Group 2 2.3 days, Group 3 2.9 days and Group 4 2.6 days. The longer stay of patients in groups 2-3-4 in RICU can be explained by the fact that plasma-hemotransfusion procedures are performed for them under the supervision of a reanimatologist.The frequency of rehospitalization during the 90-day follow-up period was 42.1% in group 1 and 8.7, 7.1, and 14.3% in groups 2, 3, and 4, respectively. The high rate of rehospitalization in patients of group 1 can be attributed to the fact that adjuvant polychemotherapy was performed, not complications in the post-diagnosis period. Postoperative complications were analyzed in 2 periods (30 and 90 days). When 30-day complications were studied, there were 6 (31.6%) in group 1, 6 (26.1%) in group 2, 4 (28.6%) in groups 3 and 4, and 2 (28.6%) Analysis of patients with complications at 90 days: group 1 7 (36.8%), group 2 8 (34.8%), group 3 5 (35.7%) and group 4 3 (42.9%).The studied patients were classified according to types of complications, their treatment and Klaven-Dindo. In some cases, 2 or more complications were observed in one patient. This sentence applies to the analysis of all groups.Among the patients of group 1, this analysis was as follows (Table 4): dynamic bowel obstruction was observed in 1 case (5.3%) and was resolved by conservative treatment. Urinary tract infection was found in 3 (15.9%) patients. Patients were given antibiotic therapy. UCS catheterization is indicated as the main reason for the high incidence of this complication. In this group of patients, urethral stricture was observed in 2 cases (10.6%) and was complicated by hydronephrosis (10.6%). To eliminate this condition, it was decided by a surgical method (nephrostomy).Table 4. Types of complications after examination (group 1)
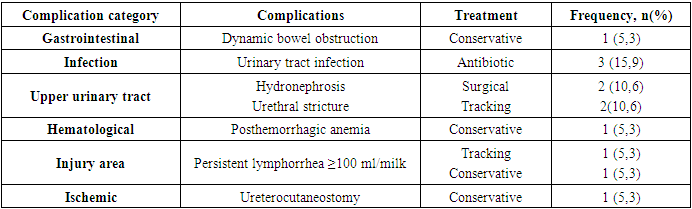 |
| |
|
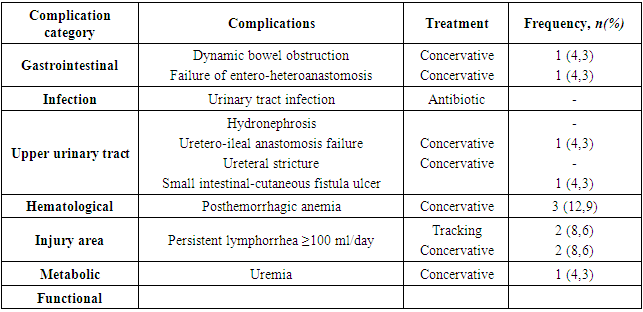
Posthemorrhagic anemia was detected in 1 case (5.3%) and was helped by conservative treatment. Blood loss in the patient was 740 ml as the local process was scattered. Persistent lymphorrhea (≥100 ml/milk) was observed in 2 (10.6%) patients. 1 patient was discharged from the hospital with a drainage tube and the dynamics decreased during follow-up without any treatment, but the second patient resolved with conservative treatment. Ischemic change (cyanosis) of the distal part of the UCS was observed in 1 patient in the first 6 hours after the examination and recovery was achieved with conservative treatment.When group 2 patients were analyzed (Table 5), dynamic bowel obstruction was observed in 1 (4.3%) case and resolved with conservative treatment. Anastomose failure was noted in one (4.3%) patient. This patient underwent surgery during the COVID-19 pandemic, and the patient was diagnosed with coronavirus on the 4th day of surgery. A small bowel-cutaneous fistula ulcer developed postoperatively and healing was observed after 12 months of conservative treatment (Figures 13-14). Reservoir function and intestinal integrity were restored. Due to infection, the patient developed cough and coagulopathy, which in turn affected the anastomosis. UIA deficiency was also noted in this patient.Table 5. Types of complications after examination (group 2)
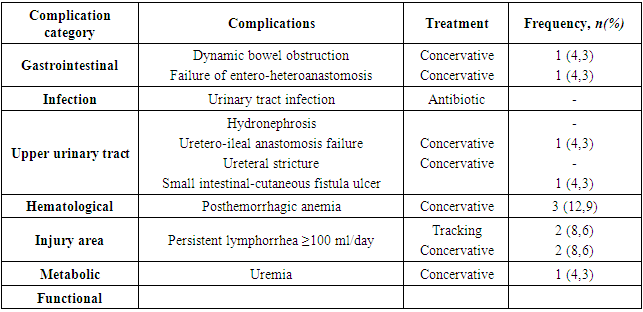 |
| |
|
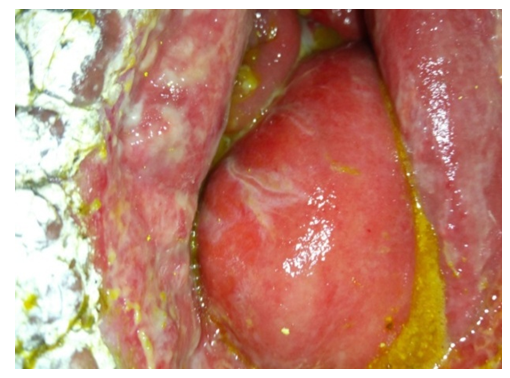 | Figure 13. Postoperative complication in a patient with COVID-19 |
 | Figure 14. Status after 1 year |
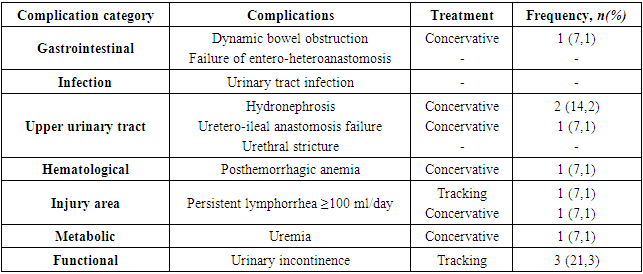
Posthemorrhagic anemia was found in 3 (12.9%) patients. Patients received antianemic treatment. Persistent lymphorrhea was detected in 4 (17.2%) patients and 2 had observation, 2 underwent conservative treatment. In general, higher levels of lymphorrhea were directly proportional to BMI and pN+ scores. Appearance of urostoma (cyanosis) was observed in 1 patient in the first 6 hours after examination, and vascularization was restored with conservative treatment.The analysis of complications observed in group 3 is as follows (Table 6): dynamic bowel obstruction was observed in 1 case (7.1%) and was resolved by conservative treatment. Unilateral hydronephrosis was noted in 2 (14.2%) patients in the post-examination period, and regression was observed after conservative treatment and observation. UIA deficiency was observed in 1 (7.1%) patient. This drainage was represented by urine coming from the tubes. Dynamics improved with the help of plasma-hemotransfusion and blood circulation restorative agents. Anemia was observed in 1 (7.1%) case.Table 6. Types of complications after examination (group 3)
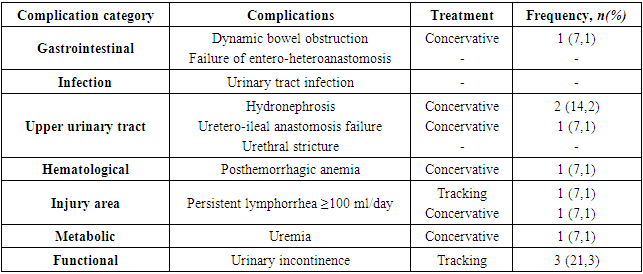 |
| |
|
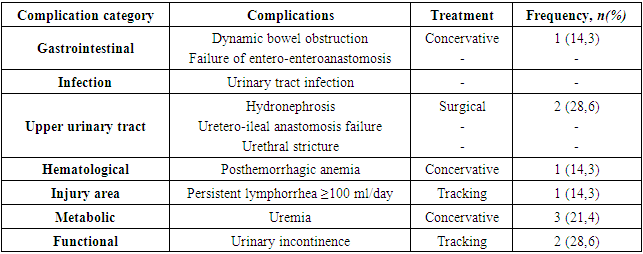
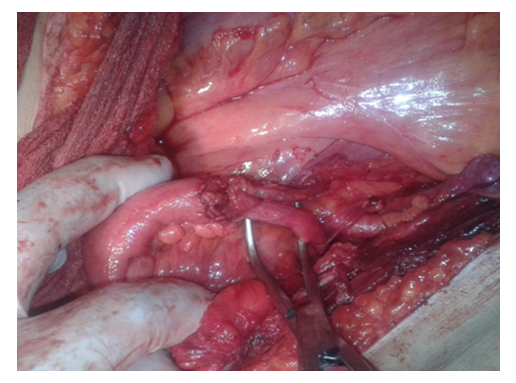
Persistent lymphorrhea was expected in 2 (14.2%) patients, and 1 of them received conservative treatment. Uremia was the main differential complication in patients who underwent orthotopic neocystoplasty. Uremia was observed in 1 (7.1%) of group 3 patients. It can be suspected that the absorption property of the reservoir caused this complication. In the next period, the condition improved with the acceleration of the urine exit time from the reservoir and conservative support. Urinary incontinence was observed in 3 (21.3%) patients, and this complication is typical for this type of surgery. This complication was also eliminated by giving the patients exercises that improve the function of the muscles of the small pelvic organs.Groups of complications were also analyzed in group 4 patients. Dynamic intestinal obstruction was observed in 1 (14.3%) patient in this group and resolved with conservative treatment. A complication such as hydronephrosis was detected in 2 patients, and in the post-examination period, urinary flow was restored by stenting the ureters. Persistent lymphorrhea was observed in 1 patient and the patient was discharged from the hospital with a drainage tube. On the 26th day after the examination, the drain was removed due to the fact that the amount of discharge in dynamics decreased to 5 ml per day. The patient was not given any conservative treatment.Table 7. Types of complications after examination (group 4)
 |
| |
|
Complication of uremia was noted in 3 (21.4%) patients. In neocystoplasty according to Hautman, the volume of the reservoir is significantly larger compared to the Studer type, and the effect on the biochemical and electrolyte parameters of the blood was high. This complication was eliminated by conservative treatment. Urinary incontinence was observed in 2 (28.6%) patients, and this complication was later resolved with exercises that improve the function of the muscles of the small pelvic organs.
4. Conclusions
The results of the analysis of early complications of radical cystectomy and neocystoplasty carried out in the conditions of the Republican specialized scientific practical medical center of oncology and radiology Andijan regional branch as the main effective treatment method for muscle invasive bladder cancer were confirmed to be satisfactory when compared with the results of the world's leading centers. Due to the fact that the number of neocystoplasty procedures was less, the percentage of the number of complications became larger. The study is ongoing because the number of patients is not yet sufficient to compare the results of the analysis.
References
| [1] | Паршин А.Г. Радикальнаяцистэктомиясотведениеммочивсегментподвздошнойкишки: результатыиосложнения (клиническоеисследование). Автореф. дис. … канд. мед. наук. 2004.159 с. |
| [2] | ПетровС.Б., ЛевковскийН.С., КорольВ.Д., ПаршинА.Г. Радикальнаяцистэктомиякакосновнойметодлечениямышечно-инвазивногоракамочевогопузыря (показания, особенноститехники, профилактикаосложнений). Практическаяонкология 2003; 4(4): 225–30. |
| [3] | Challacombe B.J., Bochner B.H., Dasgupta P. et al. The role of laparoscopic and robotic cystectomy in the management of muscle-invasive bladder cancer with special emphasis on cancer control and complications. Eur Urol 2011; 60(4): 767–75. |
| [4] | Chang S.S., Baumgartner R.G., Wells N. et al. Causes of increased hospital stay after radical cystectomy in a clinical pathway setting. J Urol 2002; 167: 208–11. |
| [5] | Chang S.S., Cookson M.S., Baumgartner M.G. et al. Analysis of early complications after radical cystectomy: results of a collaborative care pathway. J Urol 2002; 167: 2012–6. |
| [6] | Daneshmand S., Ahmadi H., Schuckman A.K. et al. Enhanced recovery after surgery in patients undergoing radical cystectomy for bladder cancer. J Urol 2014; 192(1): 50–6. |
| [7] | Dindo D., Demartines N., Clavien P.A. Classification of surgical complications. A new propisal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2005; 240: 205–13. |
| [8] | Gill I.S., Kaouk J.H., Meraney A.M. et al. Laparoscopic radical cystectomy and continent orthotopic ileal neobladder performed completely intracorporeally: the initial experience. J Urol 2002;168: 13–8. |
| [9] | Hautmann R.E., Abol-Enein H., Davidsson T. et al. ICUD-EAU International Consultation on Bladder Cancer 2012: urinary diversion. Eur Urol 2013; (63): 67–80. |
| [10] | Hollenbeck B.K., Miller D.C., Taub D. et al. Identifying risk factors for potentially avoidable complications following radical cystectomy. J Urol 2005; 174: 1231–7. |
| [11] | Johnson D.E., Lamy S.M. Complications of a single stage radical cystectomy and ileal conduit diversion: review of 214 cases. J Urol 1977; 117: 171–3. |
| [12] | Lawrentschuk N., Colombo R., Hakenberg O.W. et al. Prevention and management of complications following radical cystectomy for bladder cancer. Eur Urol 2010; 57: 983–1001. |
| [13] | Madersbacher S., Schmidt J., Eberle J.M. et al. Long-term outcome of ileal conduit. J Urol 2003; 169(3): 985–90. |
| [14] | Philip J., Manikandan R., Venugopal S. et al. Orthotopic neobladder versus ileal conduit urinary diversion after cystectomy – a quality-of-life based comparison. AnnRCollSurgEngl 2009; 91: 565–9. |
| [15] | Ramirez J.A., McIntosh A.G., Strehlow R. et al. Definition, incidence, risk factors and prevention of paralytic ileus following radical cystectomy: a systematic review. Eur Urol 2013; 64(4): 588–97. |
| [16] | Shabsigh A., Korets R., Vora K.C. et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methology. Eur Urol 2009; 55: 164–76. |
| [17] | Skinner D.G., Crawford E.D., Kaufman J.J. Complications of radical cystectomy for carcinoma of the bladder. J Urol 1980; 123: 649–53. |
| [18] | Somani B.K., Gimlin D., Fauers P., N’dow J. Quality of life and body image for bladder cancer patients undergoing radical cystectomy and urinary diversion – a prospective cohort study with a systematuc review of literature. Urology 2009; 74: 1138–43. |
| [19] | Thomas D.M., Riddle P.R. Morbidity and mortality in 100 consecutive radical cystectomies. Br J Urol 1982; 54: 716–9. |
| [20] | Anderson C.B., Morgan T.M., Kappa S. et al. Ureteroenteric anastomotic strictures after radical cystectomy - does operative approach matter? J Urol 2013; 189(2): 541–7. |





 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML