-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 194-197
doi:10.5923/j.ajmms.20241402.05
Received: Jan. 3, 2024; Accepted: Jan. 28, 2024; Published: Feb. 4, 2024

Treatment of Patients with Erythema Multiforme
Khaydar Kamilov, Kamolakhon Takhirova
Hospital Therapeutic Dentistry Department, Tashkent State Dental Institute, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study aimed to optimize the treatment of patients with exudative erythema multiforme (EM) by comparing traditional therapy with the addition of laser irradiation using photodynamic therapy (PDT). A total of 64 patients with EM participated in the study, and their clinical courses and risk factors for oral mucosa lesions were analyzed. The main group received local and general treatments, including lidocaine gel, chlorhexidine solution, and PDT, while the comparison group received traditional treatment. The effectiveness of therapy was assessed using a 3-point system based on subjective sensations and clinical symptoms. No side effects or complications were identified during the treatments. The results showed that patients in the main group experienced a significant reduction in clinical manifestations of EM compared to those in the comparison group. The average intensity of symptoms decreased by nearly 2 times on the 5th day and more than 11 times on the 15th day in the main group, whereas the reduction was 4 times and 8 times, respectively, in the comparison group. These findings suggest that the addition of laser irradiation using PDT to the treatment regimen may improve the outcomes for patients with exudative erythema multiforme. Further research is warranted to validate these results and explore the long-term effects of this approach.
Keywords: Erythema multiforme, Local therapy, Optimization, Comparative study, Photodynamic therapy, Oral mucosa
Cite this paper: Khaydar Kamilov, Kamolakhon Takhirova, Treatment of Patients with Erythema Multiforme, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 194-197. doi: 10.5923/j.ajmms.20241402.05.
Article Outline
1. Introduction
- Erythema multiforme (EM) is an acute hypersensitivity reaction characterized by characteristic skin lesions. Although it is generally a self-limiting disease, its spectrum can extend to Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). Its pathophysiology is not fully understood, but it is defined as damage to keratinocytes caused by a cell-mediated immune response to an antigenic stimulus [2,5,7] While infections play the most important role in the etiology of erythema mutiformis, drugs play an important role in SJS and TEN. Other rare causes of EM include: factors such as vaccination, leukemia, lymphoma, radiation, sun exposure and cold. [1,9,11] The prevalence of oral EM lesions varies from 35% to 65% among patients with skin lesions. Mortality rates from EM are not well documented. However, the literature suggests that between 5% of SJS and 30% of TEN can be fatal [3,4,6].Despite the variety of locally acting drugs used in the treatment of MEE, there is no single, effective, clinically and laboratory-based method (scheme) of local therapy. [8,10,12] Therefore, scientific research on the issue of local therapy for patients with MEE continues.
2. Object of Research
- Optimization of treatment of patients with erythema multiforme exudative.
3. Material and Methods of Research
- 40 people, aged 18-55 years old, with a diagnosis of exudative erythema multiforme, who applied and were under outpatient observation, took part in the study. The anamnesis of the course of MEE and the clinical course of the present relapse were studied. The frequency of occurrence of erythema multiforme exudative was determined and the causal relationships of lesions of the oral mucosa in this pathology were analyzed, including risk factors in the development of pathological conditions of the oral mucosa.The local and general treatment we use in the comparison group is considered traditional. For patients in the main group, in addition to traditional treatment, we added laser irradiation using a photodynamic therapy (PDT) device (wavelength 620-650 nm). PDT is prescribed in all periods of the disease; the method has an analgesic, epithelializing, desensitizing, and anti-relapse effect.We treated patients in the main group with local and general treatments. In local treatment the following was used:1. Lidocaine gel for anesthesia of lesions in the form of an application to the lesions (7-10 days);2. Chlorhexidine _ bigluconate 0.05% solution (1:1 dilution with distilled water) to prevent secondary infection in the form of irrigation 4-5 times a day for 5-7 days;3. Laser diode radiation was applied locally at the location on the red borders of the lips, at the border with the skin, as well as in the oral cavity (cheeks, tongue, traumatic areas of the oral mucosa). Irradiation time is 15-20 minutes. Depending on the area of the wound surface, the frequency of the procedure was 3-6 sessions.For general treatment, patients of the main group were recommended:1. Diet (the patients were recommended a hypoallergenic non-irritating diet).2. Strong AG 1amp+100.0 0.9% sodium chloride solution intravenously No. 5.3. Cycloferon IM according to the scheme.Treatment of patients in the comparison group with MEE was carried out both local and general. In local treatment, traditional treatment was recommended:1. Lidocaine gel for anesthesia of lesions in the form of an application to the lesions (7-10 days);2. Chlorhexidine _ bigluconate 0.05% solution (1:1 distilled water) to prevent secondary infection in the form of rinsing 4-5 times a day for 5-7 days (5-7 days);3. Hollisal gel application for 5-7 days.4. Vitanim A application (retinol acetate).For the general treatment of patients in the comparison group, it was recommended:4. Diet (the patients were recommended a hypoallergenic non-irritating diet).5. Strong AG 1amp+100.0 0.9% sodium chloride solution intravenously No. 5.6. Cycloferon IM according to the scheme.The local and general treatment we use in the comparison group is considered traditional. For patients in the main group, in addition to traditional treatment, we added laser irradiation using a PDT device.
4. The Results of the Study
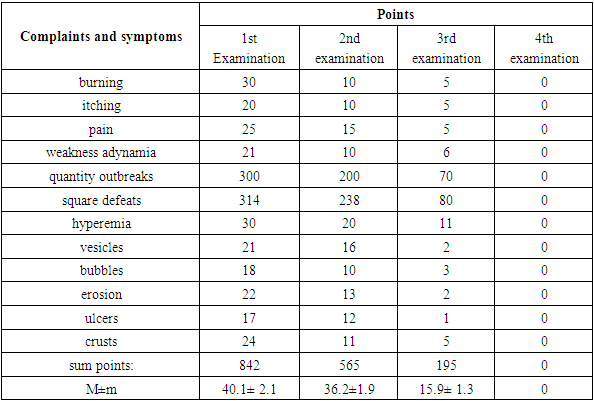
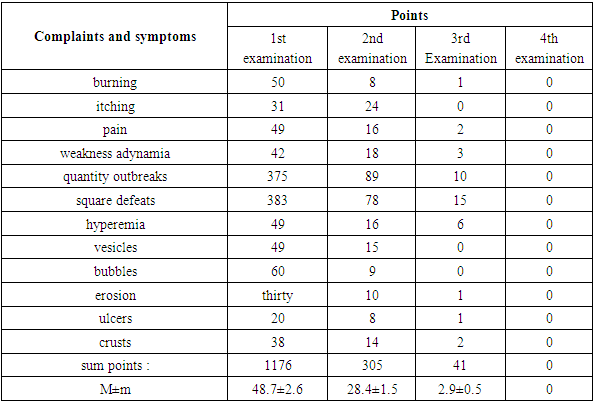
- During the treatment of patients with exudative erythema multiforme using various techniques, no side effects or complications were identified.To make the data more objective, the effectiveness of therapy for patients with exudative erythema multiforme who received various types of treatment was assessed using a 3-point system, taking into account the dynamics of subjective sensations and clinical symptoms of the disease. The three-point system included (Table 1):1. Subjective sensations:- mild itching, burning, pain - 1 point each.- constant itching, burning, pain - 2 points each.- intense itching, burning, pain - 3 points each.2. Symptoms of intoxication:- not pronounced weakness (adynamia) -1 point;- constant weakness for several days (adynamia) - 2 points;- marked weakness (adynamia) - 3 points.- increase in body temperature to subfebrile levels - 1 point; -increase in body temperature to 38°C - 2 points;- increase in body temperature over 38°C - 3 points.3. Clinical symptoms:- number of lesions (1-5 lesions - 1 point, 5-10 - 2 points, over 10 lesions -3 points).- area of affected skin and mucous membranes (up to 10 cm - 1 point, 10-20 cm - 2 points, over 20 cm - 3 points).Hyperemia:- weak -1 point,- distinct -2 points,- acute inflammatory erythema - 3 points.Vesicles (single - 1 point, 10-20 elements - 2 points, more than 20 - 3 points).Bubbles (single - 1 point, 10-20 elements - 2 points, more than 20 - 3 points).Erosion (single - 1 point, 10-20 elements - 2 points, more than 20 - 3 points).Ulcers (one - 1 point, two - 2 points, more than 2 - 3 points).Crusts (single - 1 point, 10-20 elements - 2 points, more than 20 - 3 points). According to the summary data for the groups, analysis and mathematical processing of the data obtained was carried out.
|
|
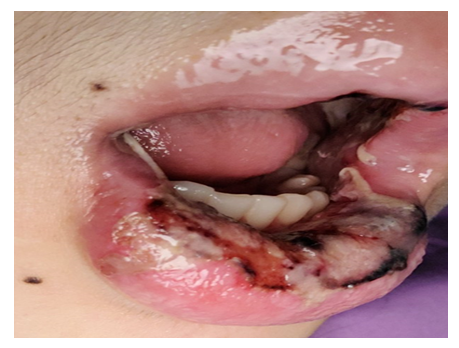 | Figure 1. Patient M., 22 years old, before treatment |
 | Figure 2. Patient M., 22 years old, after treatment |
5. Conclusions
- Thus, based on the studies conducted, we can come to the conclusion that complex treatment contributed to the rapid regression of clinical manifestations of erythema multiforme and a marked reduction in the frequency and duration of relapses of the disease. Complex, pathogenetically based treatment, including the use of PDT, led to rapid relief of clinical signs of MEE (within 3-6 days) and a significant reduction in the frequency (up to 1-2 times a year) and duration of ME relapses.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML