-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(2): 189-193
doi:10.5923/j.ajmms.20241402.04
Received: Jan. 2, 2024; Accepted: Jan. 29, 2024; Published: Feb. 4, 2024

Minimally Invasive Methods for the Diagnosis of Destructive Lesions of the Spine
Zulfiya Makhmudova
Republican Specialized Scientific and Practical Medical Center of Tuberculosis and Pulmonology, Tashkent, Uzbekistan
Correspondence to: Zulfiya Makhmudova, Republican Specialized Scientific and Practical Medical Center of Tuberculosis and Pulmonology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objectives: To evaluate the usefulness of diagnostic trepan-biopsy in the differential diagnosis of spine patients with confined estructive lesions of various ages. Material and Methods: 55 patients were treated for destructive lesions restricted to a single spinal motion segment with percutaneous vertebral body trepan biopsy, followed by cytological and histological examinations of bioptates. These patients were brought with a suspicion of tuberculous spondylitis. The pathology's structure and potential complications were established. Results: In 75% of patients, the results of cytological and histological examination of bioptates supported the diagnosis. Conclusions: If manipulation is carried out earlier, before indication of antibacterial or tuberculostatic therapy, the informative value of cytological and histological study of trepan biopsy sample may be higher. If there is a paravertebral soft-tissue component, an aspiration biopsy should be added to the trepan biopsy along with extra bacteriologic and cytological examination.
Keywords: Extrapulmonary tuberculosis, Spondylitis, Spinal tumor, Biopsy
Cite this paper: Zulfiya Makhmudova, Minimally Invasive Methods for the Diagnosis of Destructive Lesions of the Spine, American Journal of Medicine and Medical Sciences, Vol. 14 No. 2, 2024, pp. 189-193. doi: 10.5923/j.ajmms.20241402.04.
1. Introduction
- Identification of a destructive process in the spine and its nosological verification in case of limited vertebral fractures present specific difficulties due to polymorphism and non-specificity of radiation manifestations of destruction with the low information content of unique methods used in the diagnosis of specific inflammatory processes, such as chest radiography and skin tuberculin tests [1]. Such signs as a pathological fracture and destruction of the vertebral body, as well as paravertebral formations, are found in spondylitis (tuberculous and nonspecific) and tumors of the vertebrae. In this case, accurate disease diagnosis is critical for timely appointment of appropriate treatment. Refusing morphological verification of the diagnosis with a seemingly typical radiation picture in oncological diseases and compression fractures in osteoporosis results in a high (up to 84%) detection of diagnostic and therapeutic errors, which in some cases are critical to the patient's life [2,3]. Dissatisfaction with the results of non-invasive diagnostics of inflammatory diseases of the spine requires a wider introduction of interventional methods with further analysis of their results. The positive data obtained by the authors of this article during a blinded prospective study of a limited group of children have already been published previously [4]. Despite the minimal number of complications of vertebral trepanobiopsy [5,6], the number of publications on its use in the differential diagnosis of spondylitis is extremely small [7-10].Surgical excision and anterior column reconstruction have traditionally been the recommended treatments, but they are occasionally not advised for patients who have serious medical issues. For pyogenic spondylodiscitis, recent papers have detailed posterior fixation methods using an open approach [11,12]. Additionally, for patients with many comorbidities, minimally invasive spine stabilization (MISt) with a percutaneous pedicle screw (PPS) may be a less invasive option.With the description of tubular retractors for access to the lumbar spine and the report of the first lumbar microendoscopic discectomy, modern minimally invasive spine surgery (MIS) was first performed in the 1990s. Since then, improvements in medical technology and surgical instruments have caused MIS to become a significant and quickly expanding area of spine surgery. Today, a range of spinal pathologies, including degenerative disc disease, disc herniation, instability, deformity, fracture, infection, and malignancies, are treated using MIS techniques and methods [13,14]. MIS was pursued as a way to lessen iatrogenic tissue injuries during surgery as opposed to the standard open spine surgery [15,16]. Smaller incisions, less soft tissue damage, decreased estimated blood loss (EBL), decreased postoperative pain and narcotic use, shorter hospital length of stay (LOS), quicker recovery, and quicker return to work and normal activity are some of the theoretical advantages of MIS over traditional open surgery [17]. Traditional open spine surgery techniques frequently necessitate significant muscle and ligamentous disturbance during the surgical approach to the spine, decreasing spinal stability and causing eventual morbidities [18]. By using self-retaining retractor devices to prevent muscle crush injury, known anatomic neurovascular and muscle planes, avoiding disruption of the tendon attachment sites of critical muscles at the spinous processes, and limiting the surgical corridor's width, MIS reduces approach-related morbidity. Important benefits of MIS over open spine surgery include the reduction in approach-related morbidity and indirect iatrogenic instability of the spine [19-21].This study aims to evaluate the accuracy of diagnostic puncture-trepanation biopsies for the differential diagnosis of limited destructive lesions of the spine in patients of different age groups.
2. Materials and Methods
- In 2018–2021 55 patients aged 20 to 77 years old, hospitalized in the osteoarticular department of the RSSPMC F and P with suspected tuberculous spondylitis, underwent closed percutaneous trepanobiopsies of the vertebral bodies at the stage of preoperative examination using a unified technique. Inclusion in the study was determined by the presence of the destruction of the vertebral bodies, detected by radiation methods, limited to one spinal motion segment. The leading complaint in all patients was pain at the level of the affected vertebrae and also the majority of them suffered from neurological disorders of varying severity. In most patients, the duration of the disease by the time of admission to the clinics exceeded from 3 months to 5 years. At the stages of examination in the general medical network, patients underwent a complex of radiological studies: X-ray spondylography, MRI, CT of the spine, and 15 patients underwent PET diagnostics. In addition to the general clinical examination, all of them underwent chest radiography in order to possibly identify a pulmonary process;Additionally, skin tuberculin and Diaskin tests were performed. The pathological process was localized in the cervical region in 5 patients, in the thoracic region in 17 cases, in the thoracolumbar region in 11 patients, in the lumbar region in 13 patients, and in the lumbosacral spine in 9 patients.Patients were administered sedative and analgesic drugs 30 minutes before the study, and infiltration anesthesia was used directly during the manipulation while maintaining consciousness and speech contacts. Biopsies were performed under aseptic operating room conditions, using special bone biopsy needles (so-called Yamshidi needles, 9G and 11G), with radiation control on a C-arm X-ray unit. Manipulations were performed in the patient’s prone position, with the exception of cervical localization (done in the supine position with finger control of the median structures of the neck and blood vessels). The position of the needle was controlled by fluoroscopy. In 3 adults in the thoracic region, a biopsy was performed from a transpedicular approach by marking the projection of the root of the arch and inserting a needle closer to the lateral bone wall; in other cases, a posterolateral extrapedicular approach was used (the disadvantage of the transpedicular approach is the difficulty of changing if it is necessary to angulate the needle for targeted sampling in the area of interest, which is possible with a more mobile extrapedicular approach. The obtained column of bone tissue was sent for histological examination, additionally, a cytological examination of smears was analyzed (a cytological examination was examined in the case of obtaining a soft tissue substrate); the liquid contents were sent for bacteriological examination.
3. Results
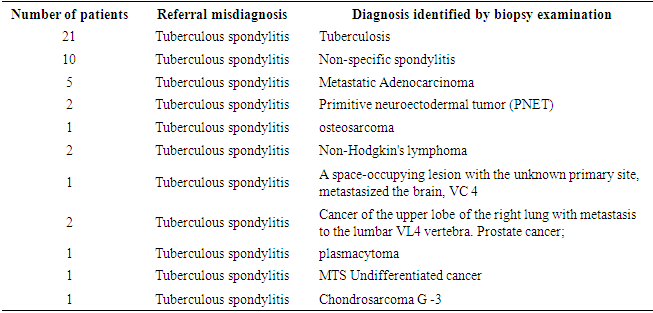
- Biopsy data made it possible to determine the diagnosis in 47 of 55 cases in adults (Table 1). Biopsy data made it possible to determine the diagnosis in 47 of 55 cases in adults. Only eight materials of biopsies gave non -informative data. Out of 55 patients with suspected tuberculous spondylitis, only 21 had the disease confirmed (in these acid-resistant bacteria were present in analysis during bacterioscopy of the punctate), and non-specific inflammation was found in 10. The tumor process was histological and immunohistochemical verified in the remaining 16 cases.
|
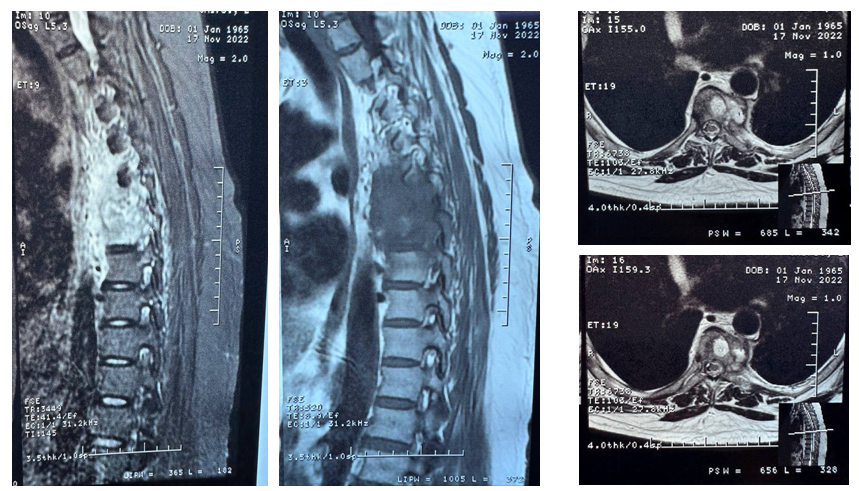 | Figure 1. MRI images of the thoracic vertebrae |
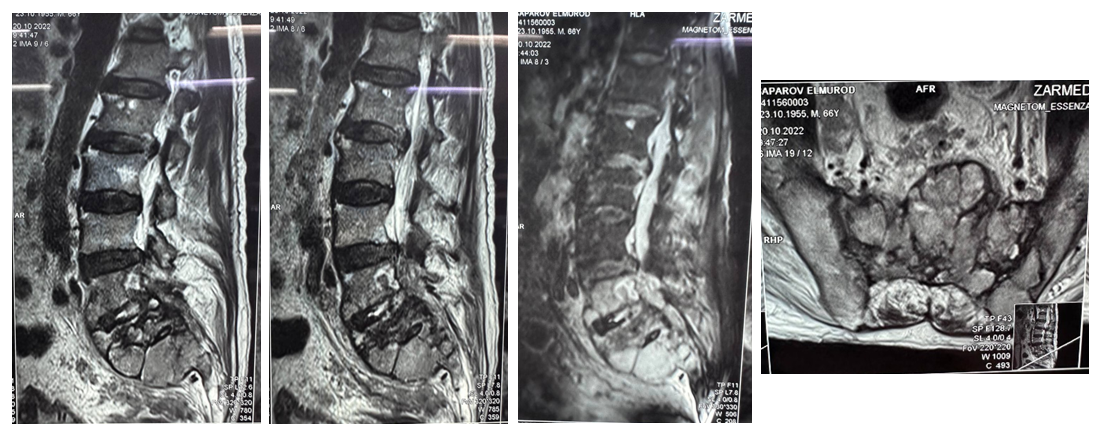 | Figure 2. MRI images of the lumbosacral vertebrae |
4. Conclusions
- Percutaneous Trepan Biops of the vertebrae is one of the informative and relatively safe methods of interventional diagnosis of spinal lesions. This method should be applying for preoperative differentiation of inflammatory (tuberculous and nonspecific spondylitis), traumatic and neoplastic diseases accompanied by the destruction of one spinal motion segment. The method's diagnostic accuracy in the case of limited destructive processes is quite high, and according to our data, it is 75.0 percent in adults. In the structure of mono-segmental degradation of the spine with suspected tuberculous spondylitis, nonspecific spondylitis in adults and tumor lesions, including malignant ones, predominate. The severest complications of percutaneous trepanobiopsy of the vertebrae that we observed were due not to technical reasons, but the progression of a nonspecific inflammatory process (epiduritis) against the background of osteomyelitis of the spine. Transient complications in the form of radiculopathy and pneumothorax, with their timely recognition and adequate treatment, were not accompanied by clinical consequences. Perhaps, the information content of cytological and histological studies of punctate obtained during trephine biopsy may be higher if this manipulation is performed as early as possible, before the appointment of antibacterial or tuberculostatic therapy to the patient, combined with aspiration biopsy of the material with additional bacteriological and cytological studies in the presence of soft tissue paravertebral component.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML