K. F. Erkinova1, F. B. Nurmukhamedova2
1Samarkand State Medical University, Samarkand, Uzbekistan
2Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: Allergic rhinitis (AR) and rhinosinusitis in children are commonly associated with inflammatory processes in the nasal passages, leading to varying degrees of respiratory dysfunction. This study aimed to compare traditional and comprehensive treatments for allergic rhinitis in children with sinusitis. Methods: Patients were divided into two groups for a comparative analysis. Group 1 (n=20) received traditional conservative therapy, while Group 2 (n=20) underwent additional inhalation therapy using the PARI-SINUS inhaler. Results: It is evident that Group 2, which received both traditional conservative therapy and inhalation therapy using the PARI-SINUS inhaler with the corticosteroid budesonide delivered through pulsating aerosol, demonstrated superior dynamics in the parameters. This indicates the effectiveness of comprehensive treatment, highlighting its favorable outcomes. Conclusion: We have concluded that a comprehensive examination and treatment of children with rhinosinusitis and allergic rhinitis is reasonable and effective to include the Pari-sinus method in traditional therapy.
Keywords:
Allergic rhinitis, Rhinosinusitis, Children, Inhalation therapy
Cite this paper: K. F. Erkinova, F. B. Nurmukhamedova, A Comparative Analysis of Treatment for Allergic Rhinitis Combined with Rhinosinusitis in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 1, 2024, pp. 163-167. doi: 10.5923/j.ajmms.20241401.35.
1. Introduction
Allergic rhinitis (AR) significantly impacts the lives of children worldwide, affecting academic performance, sleep, and emotional well-being [1]. This form of inflammation is triggered by exposure to environmental allergens interacting with immunoglobulin (Ig) E in sensitized individuals. Repeated exposures lead to systemic and local changes, including the activation of nasal eosinophils, increased adhesion molecule levels in the respiratory pathways, and an intensified systemic response to allergens [2]. AR has historically been associated with comorbid upper respiratory tract conditions [3] [4].Allergy should be considered not only as an etiological factor but also as an exacerbating factor that can contribute to exacerbations, and thus, its adequate treatment can improve disease outcomes [5]. From a clinical perspective, the results are more conflicting than laboratory findings. Literature studies comparing the incidence of upper respiratory tract infections in individuals with and without allergies are relatively scarce. Karevold et al. argue that patients with atopy/allergy had increased susceptibility to upper respiratory tract infections [6], and atopy increases the risk of bronchopulmonary pathologies in children. Notably, the most significant risk factor was atopy, especially in domestic settings (humidity). Accordingly, Ciprandi et al. found that allergic children more frequently experience upper respiratory tract diseases, which are more severe in duration and severity compared to non-allergic children [8]. Other authors disagree with these statements [7] and consider the correlation between upper respiratory tract infection and atopic diseases weak and inconclusive. Sütçü et al. confirmed that the number of yearly episodes did not significantly differ between atopic and healthy children, even though atopic children had longer recurrent episodes of viral-induced wheezing compared to the control group [8].The association between allergy and chronic rhinosinusitis (CRS) in adults has been discussed for many years, but research on CRS in children is less common [9]. The findings of studies do not unequivocally link allergy to chronic rhinosinusitis. Some studies confirm a positive clinical connection between allergic rhinitis (AR) and CRS, describing prevalence ranging from 27 to 59% of patients [10], suggesting a clinically significant association, especially in older children.Authors argue that a specific assessment of allergic diseases should be considered when treating chronic or recurrent CRS. Anamika et al. [11] noted a positive skin test in 53% of cases in children with CRS. Some studies have shown that antibiotic treatment alone did not help alleviate rhinosinusitis symptoms in children with allergies [12].Despite growing knowledge about allergy and CRS in children, it is still unclear whether AR can contribute to CRS or if they share only a common pathogenesis. Although AR has been positively linked to CRS in several experimental and clinical studies in children, contradictory results exist. The aforementioned underscores the need for further research to confirm whether anti-allergic treatment can improve CRS outcomes in children.Thus, the societal significance of AR can be considered one of the most pressing issues in medicine, requiring a deeper exploration of its etiology and pathogenesis and the development of new and effective therapeutic methods.Research Objective: To compare traditional and comprehensive treatments for allergic rhinitis in children with sinusitis.
2. Materials and Methods
From 2021 to 2023, we examined 40 children with allergic rhinitis and concurrent rhinosinusitis at the Tashkent Pediatric Medical Institute. The diagnosis was determined through a comprehensive assessment, including patients' complaints, medical history, and clinical, laboratory, and instrumental studies.Patients diagnosed with allergic rhinitis and rhinosinusitis were divided into two groups for a comparative analysis. Group 1 (n=20) received traditional conservative therapy, while Group 2 (n=20) underwent additional inhalation therapy using the PARI-SINUS inhaler. This group was administered the corticosteroid budesonide (Pulmicort) through pulsating aerosol delivery via the device. The conservative treatment protocol comprised antibacterial and antihistamine therapies, nasal vasoconstrictor drops, the Proetz maneuver, and maxillary sinus puncture. Antibiotic therapy (cefotaxime 50 mg/kg body weight intramuscularly twice daily or amoxiclav orally 40 mg/kg body weight three times a day, depending on the patient's age) lasted for 7 days. Endonasal sinus and nasal cavity sanitation according to Proetz (150 ml 0.9% NaCl solution twice daily) were performed for 7 days when indicated.After the completion of conservative therapy, we compared the results of complaints using the SNOT 22 questionnaire before treatment in groups receiving traditional and comprehensive therapy.
3. Results and Discussion
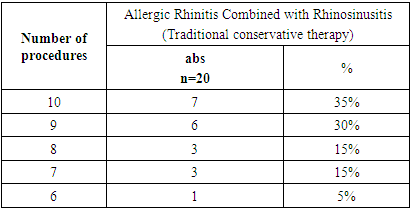
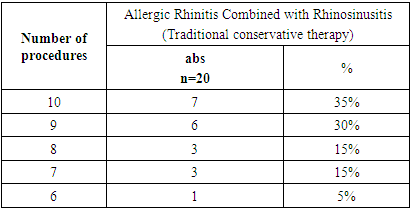
Twenty children received traditional therapy, with most undergoing procedures such as the Proetz method for nasal sinus accessory cavity sanitation and maxillary sinus puncture. The average number of performed procedures reached up to 12 times throughout the entire treatment period, as some patients underwent sanitation twice a day. In total, 7 (35%) children received 12 procedures, 6 (30%) underwent 9 procedures, 3 (15%) had 8 procedures, and an additional 3 (15%) underwent 7 procedures, while only 1 (5%) child received 6 procedures. We did not identify any cases where a child underwent only 4-5 procedures during inpatient treatment (see Table 1). Additionally, one-third of children in this group, in addition to the Proetz maneuver, required maxillary sinus puncture. Depending on the treatment effectiveness, the physician applied either Proetz maneuver alone or in combination with Posterior Nasal Pack (PNP) sanitation and maxillary sinus puncture using the Kulikovsky needle. Consequently, 3 (15%) patients underwent 4, 5, or 6 maxillary sinus punctures, 2 children (10%) had 3 punctures, and 1 child received 1 puncture (5%).Table 1. Frequency of Nasal Sinus Accessory Cavity Sanitation in Children Undergoing Traditional Treatment
 |
| |
|
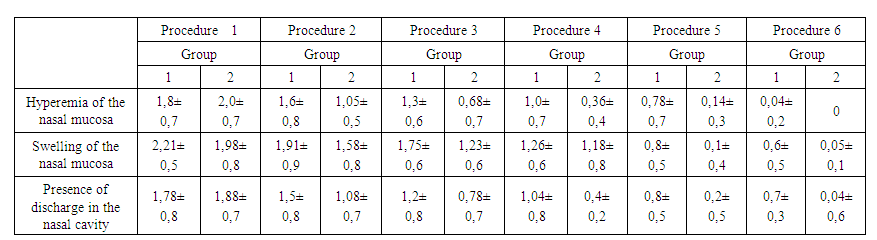
After receiving traditional treatment, on the first day following maxillary sinus puncture, blockage of the natural ostium of the maxillary sinus was observed in 2 children, while 3 children exhibited a significant amount of thick purulent discharge. Seven children had a moderate amount of pus, and 2 had mucous-like pus. Repeat puncture of the maxillary sinus on the next day showed no significant improvement compared to the previous day, with no notable change in dynamics between the first and second procedures (p=0.55).By the third day of maxillary sinus punctures, a considerable improvement in sinus content was noted. Patients who initially had a significant amount of purulent discharge experienced a drastic reduction, with most now showing mucopurulent secretions. Comparing the results of the first and second procedures revealed significant improvements (p=0.001). The positive trend observed on the third day continued throughout the entire therapy, but the average score reduction did not exceed 7% daily until the 7th procedure. Subsequently, there was progressive improvement after each procedure, almost doubling the results after each session, reaching a score of 0.06±0.37 by the 10th procedure and 0.02±0.2 by the 12th procedure. This corresponded to the results achieved after the 5th procedure when using the PARI-SINUS inhalation.In contrast, the situation in the comparative group using the PARI-SINUS inhaler with budesonide via pulsating aerosol showed that, on average, 4 inhalation procedures with PARI-SINUS (30.7%) or 5 procedures (53.8%) were required for complete sanitation. Six patients underwent Posterior Nasal Pack (PNP) sanitation (15.4%), and 1 patient each underwent 7 and 8 procedures (7.6%).Blockage was detected in 1 patient (7.6%) during the 1st procedure, abundant pus was observed in 3 patients (23.0%), moderate purulent discharge in 3 patients (23.0%), mucopurulent discharge in 4 patients (30.7%), and mucous discharge in 2 patients (13.3%). By the 2nd procedure, a sharp change in the clinical picture was observed: no natural ostium blockage was recorded, the number of patients with abundant purulent discharge immediately decreased to 1, with moderate pus in 2, and 4 patients had mucous-like discharge, along with 1 child showing a complete absence of discharge. The difference in results from the initial examination was statistically significant (p=0.0000).By the third day, a reduction in discharge was observed, resulting in a significant difference in the mean scores of 12 affected children between the second and third visits to the doctor, leading to statistically significant results (p=0.0000). Only 7 patients underwent the fourth treatment procedure. Among them, three children predominantly had mucous discharge, while four had a mixture of pus. By the 5th procedure, only 4 affected children remained. Two had a minimal amount of mucous discharge, and two had mucopurulent discharge. All of them underwent the 6th procedure.The alleviation of symptoms and improvement in clinical course for those receiving inhalation therapy occurred in 6.8±2.35 days, whereas for those undergoing traditional therapy, it was 10.9±2.7 days with incomplete symptom resolution. Applying inhalation therapy significantly improved treatment outcomes for affected children, reducing the therapy duration by 40% and increasing the recovery rate by 2.5 times.The resolution of symptoms and improvement in the clinical course for those receiving inhalation therapy took 6.8±2.35 days, while for those undergoing traditional therapy, it was 10.9±2.7 days with incomplete symptom resolution. The application of inhalation therapy significantly enhanced treatment outcomes in affected children, reducing the duration of therapy by 40% and increasing the recovery rate by 2.5 times. According to objective symptom data after the administered treatment, symptoms of Allergic Rhinitis decreased in both subgroups, with the best dynamic indicators observed in Group 2 (see Table 2).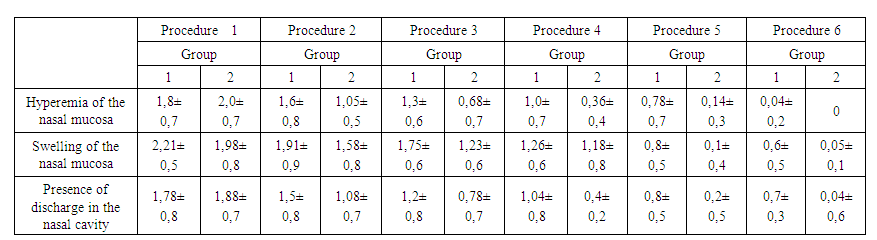 | Table 2. Dynamics of Objective Symptoms of Allergic Rhinitis Combined with Rhinosinusitis during Treatment by Groups in Scores |
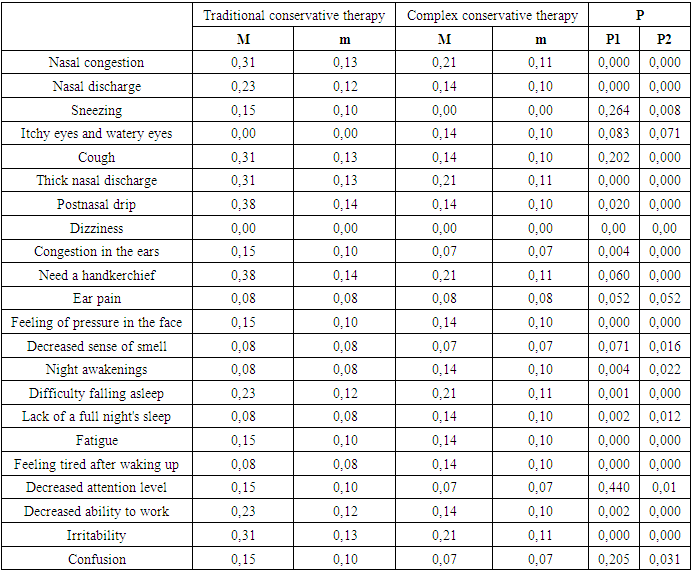
The results of our data analysis revealed that children with allergic rhinitis combined with rhinosinusitis in both comparison groups exhibited positive outcomes across a range of parameters. However, in certain cases, statistically significant changes were not observed. Notably, complaints related to nasal congestion, thick nasal discharge, facial discomfort, difficulty falling asleep, fatigue, and irritability achieved a significance level of P<0.001 in both comparative groups. Conversely, specific complaints, such as sneezing, tearing, itching in the eyes, coughing, the need for a nasal tissue, decreased sense of smell, and reduced attention levels, demonstrated a statistically significant improvement in Group 2 (P<0.05), a result not observed following traditional therapy in patients of Group 1 (Table 3).Table 3. Frequency of Complaints after Treatment in Children with Allergic Rhinitis Combined with Rhinosinusitis
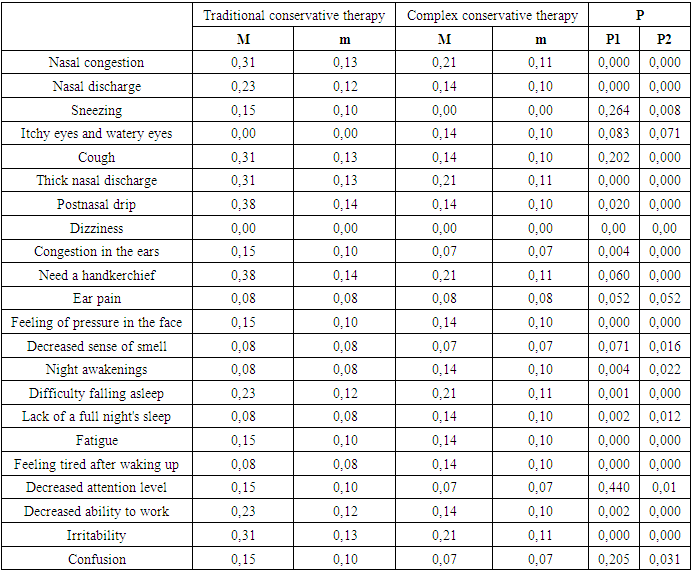 |
| |
|
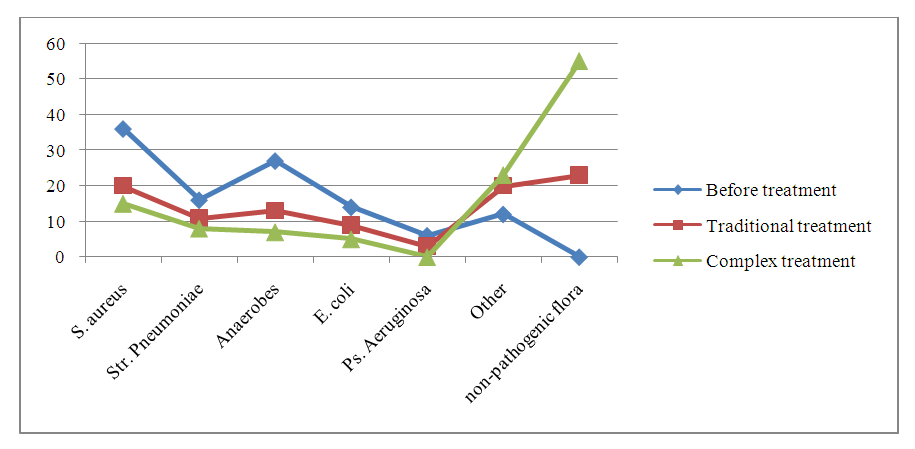
Based on the presented results, it is evident that Group 2, which received both traditional conservative therapy and inhalation therapy using the PARI-SINUS inhaler with the corticosteroid budesonide delivered through pulsating aerosol, demonstrated superior dynamics in the parameters. This indicates the effectiveness of comprehensive therapy, highlighting its favorable outcomes.The prescribed treatment, incorporating anti-inflammatory and antiallergic therapy, not only led to the improvement of the overall condition of the children, as evidenced by the complaints and objective examination data, but also normalized the cellular composition of the nasal cavity.A reduction in the number of pathobionts was observed in children with allergic rhinitis after therapy in both groups. In children from Group 2, immediately after PARI-SINUS therapy with beclomethasone aerosol pulsatile delivery, the number of anaerobes decreased to isolated cases.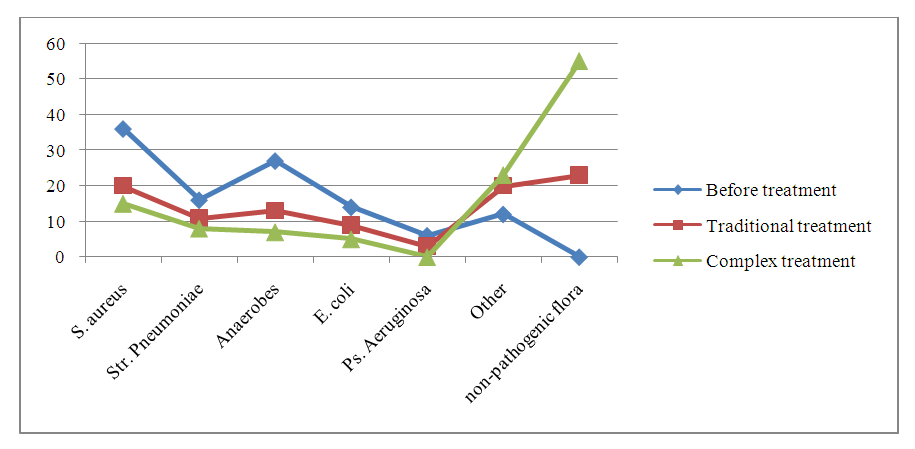 | Diagram 1. Indicators of nasal microbiota after different therapies in children with allergic rhinitis combined with rhinosinusitis |
The inflammatory process of the nasal passages and nasal cavities in allergic rhinitis was accompanied by respiratory dysfunction of varying degrees of severity. A relatively moderate obstructive nature was detected in the majority of patients, but half of the children with allergic rhinitis and rhinosinusitis still had total nasal airflow rates below 90 cm^3/s. The manifestation of pathological changes correlated with age; it should be noted that children under 7 years old exhibited more pronounced clinical symptoms.An objective assessment of nasal function using anterior rhinomanometry in children with allergic rhinitis combined with rhinosinusitis revealed a significant reduction in air flow (12.51±3.65). The rhinomanometry data indicated difficulty in nasal breathing, corresponding to a marked degree of nasal obstruction. Analysis of average values of anterior rhinomanometry for the right and left nasal cavities during inhalation and exhalation phases did not show statistically significant differences (p < 0.05) between nasal resistance values and nasal airflow volume.
4. Conclusions
In conclusion, a thorough assessment and management of pediatric rhinosinusitis and allergic rhinitis prove both rational and efficacious. Incorporating the Pari-sinus method into conventional treatments enhances overall effectiveness, underscoring the significance of a comprehensive approach in optimizing care for children with these conditions.
References
| [1] | Samojlik I, Mijatović V, Petković S, Skrbić B, Božin B. The influence of essential oil of aniseed (Pimpinella anisum, L.) on drug effects on the central nervous system. Fitoterapia. 2012; 83(8): 1466-1473. |
| [2] | Sethi RK, Kozin ED, Naunheim MR, Rosen M, Shrime MG, Sedaghat AR, Gray ST. Variable utilization patterns of computed tomography for rhinosinusitis in emergency departments. Laryngoscope. 2017; 127(3): 537-543. doi: 10.1002/lary.26217. Epub 2016 Aug 22. PMID: 27546301. |
| [3] | Revonta M, Kuuliala I. The diagnosis and follow-up of pediatric sinusitis: Water's view radiography versus ultrasonography. Laryngoscope. 1989; 99(3): 321-4. doi: 10.1288/00005537-198903000-00016. PMID: 2645496. |
| [4] | Amonov SE, Erkinova KF, Nurmuxamedova FB, Khamrakulova NO. Clinical course of allergic rhinitis combined with adenoid vegetation and rhinosinusitis in children. J Biomed Pract. 2023; 8(2). |
| [5] | Picon PC, Picon RV, Costa AF, Sander GB, Amaral KM, Aboy AL, Henriques AT. Randomized clinical trial of a phytotherapic compound containing Pimpinella anisum, Foeniculum vulgare, Sambucus nigra, and Cassia augustifolia for chronic constipation. BMC Complement Altern Med. 2010; 10: 17. |
| [6] | Farneti P, Sciarretta V, Macrì G, Piccin O, Pasquini E. Silent sinus syndrome and maxillary sinus atelectasis in children. Int J Pediatr Otorhinolaryngol. 2017 Jul; 98: 150-157. doi: 10.1016/j.ijporl.2017.05.005. |
| [7] | Mendiratta V, Baisakhiya N, Singh D, Datta G, Mittal A, Mendiratta P. Sinonasal anatomical variants: CT and endoscopy study and its correlation with extent of disease. Indian J Otolaryngol Head Neck Surg. 2016; 68(3): 352-358. doi:10.1007/s12070-015-0920-x. |
| [8] | Song WY, Ma YB, Bai X, Zhang XM, Gu Q, Zheng YT, Zhou J, Chen JJ. Two new compounds and anti-HIV active constituents from Illicium verum. Planta Med. 2007; 73(4): 372-375. doi: 10.1055/s-2007-967162. |
| [9] | Kaya M, Çankal F, Gumusok M, Apaydin N, Tekdemir I. Role of anatomic variations of paranasal sinuses on the prevalence of sinusitis: Computed tomography findings of 350 patients. Niger J Clin Pract. 2017; 20(11): 1481-1488. |
| [10] | Ciofalo A, Pasquariello B, Iannella G, et al. The role of nasal cytology in the diagnosis of allergic and non-allergic rhinitis in adults and children. Eur Rev Med Pharmacol Sci. 2019; 23(12): 5065-5073. doi: 10.26355/eurrev_201906_18170. PMID: 31298361. |
| [11] | Anamika A, Chakravarti A, Kumar R. Atopy and quality of life in pediatric chronic rhinosinusitis. Am J Rhinol Allergy. 2019; 33(5): 586–90. |
| [12] | Nurmuxamedova FB. Adenoid vegetation in children with allergic rhinitis. Scientific Ideas of Young Scientists. 30, 2021. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML