Babajanov Akhmadjon Sultanboyevich, Saidov Shuxrat Abdunasimovich
Samarkand State Medical University, Uzbekistan
Correspondence to: Babajanov Akhmadjon Sultanboyevich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The study is based on the results of a comprehensive examination and treatment oMGD and its causes is based on the principle from simple to complex (from non-invasive methods to invasive ones). Diagnosis of MRCG using a developed diagnostic algorithm, including modern non-invasive non-radiation methods (ultrasound, MRCP) diagnostics, as well as invasive puncture and endoscopic diagnostics (RPCG, PCCG) with a transition to decompression of the biliary tract (73.64% of patients in the main group were performed).
Keywords:
Obstructive jaundice of benign origin, Radiation diagnostic methods
Cite this paper: Babajanov Akhmadjon Sultanboyevich, Saidov Shuxrat Abdunasimovich, Aspects of X-Ray Endobiliary Surgery for Mechanical Jaundice of Benign Genesis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 1, 2024, pp. 147-152. doi: 10.5923/j.ajmms.20241401.33.
1. Relevance of the Problem
Pathology of the organs of the hepatopancreatobiliary zone occupies one of the leading places among the causes of benign obstructive jaundice (OBJ) [1,3,7,9]. MRDH progresses intensively and leads mainly to the progression of liver and multiple organ failure [2,4,10,12]. Its social significance is growing everywhere in all countries of the world, including the Republic of Uzbekistan, and is primarily associated with an increase in the incidence of cholelithiasis, choledocholithiasis, diseases of the major duodenal papilla, liver echinococcosis, as well as bile duct strictures [5,8,11].The problem of an optimized algorithm for early diagnosis, pathogenetically based treatment regimens and predicting the course of liver failure in MGD remains incompletely studied. The difficulties of early diagnosis of MGD are due to the polyetiological nature of the disease, the absence of pathognomy symptoms and laboratory indicators characteristic of various causes of bile duct obstruction. Of course, the development and improvement of new methods for complex diagnosis of the causes of MFDH are relevant [5,10,13].
2. The Purpose of the Study
The purpose of the study is to evaluate the role of modern instrumental research methods in diagnosing the etiology of obstructive benign jaundice and, based on this, to develop a diagnostic and treatment algorithm.
3. Material and Research Methods
The study is based on the results of a comprehensive examination and treatment of 212 patients with MGD who were in the clinic from 2016 to 2023. The cause of the main bile duct occlusion in 102 (48.1%) cases was cholelithiasis complicated by choledocholithiasis, in 39 (18.4%) the causes of the disease were pathologies of the duodenal stenosis and its stenosis, and in 8 (3.8%) - Mirizzi syndrome.There were 15 patients (7.1%) with the main bile duct occlusion caused by cicatricial strictures of the biliary tract. A separate group consisted of 24 (11.3%) patients with mechanical parasitic (echinococcal) jaundice caused by secondary (breakthrough) and primary lesions of segmental, lobar and extrahepatic bile ducts. The main bile duct occlusion developed in 9 (4.2%) cases with biliary pancreatitis, and in 3 (1.4%) with pseudotumor pancreatitis. In 5 (2.3%) cases, congenital diseases of the bile ducts were represented by common bile duct cysts complicated by bile ducts. Rare causes of the main bile duct occlusion in 3 (1.4%) cases were penetration of a low post bulbar ulcer into the duodenum and common bile duct, as well as early postoperative jaundice (n=5), caused by clipping of the common bile duct during laparoscopic cholecystectomy.
4. Results and Its Discussion
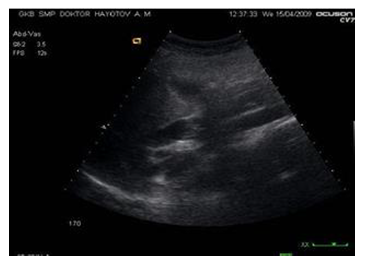
A comprehensive traditional ultrasound examination was performed in all patients with MGD. The objectives of ultrasound in patients with main bile duct occlusion were: determining the cause of biliary obstruction, biliary hypertension, the diameter of the bile ducts, the level and localization of the obstruction zone, the condition of the hepatoduodenal ligament, the BSD and the head of the pancreas and liver. The presence of choledocholithiasis, as a cause of the main bile duct occlusion, was characterized by the presence of various sizes of stones in the gallbladder and bile duct and dilation of the intrahepatic bile ducts. | Figure 1. Ultrasound. Choledocholithiasis |
 | Figure 2. Ultrasound. Dilatation of intrahepatic bile ducts |
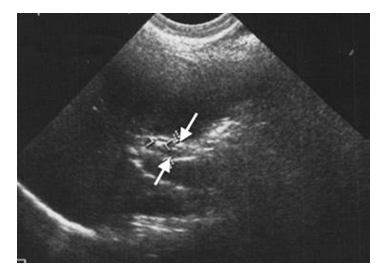
When performing ultrasound, it was possible to visualize the common bile duct in almost all patients with bile duct, but only in 42 patients it was possible to examine its entire length. Its diameter averaged 8.1 ± 3.9 cm (from 3.7 to 25 mm).Main bile duct occlusion was accompanied by biliary hypertension with the presence of sonographic signs - an increase in the diameters of the intrahepatic and extrahepatic bile ducts. Comprehensive ultrasound allowed us to diagnose and determine the level of obstruction of the biliary tree. Obstruction at the level of segmental ducts, lobar ducts, and at the level of confluence was characterized by various ultrasound signs. The most demonstrative ultrasound picture was observed with low biliary obstruction, while in 89% of cases dilation of the hepaticcholedochus, lobar and segmental ducts was detected. Diagnosis of high biliary obstruction turned out to be somewhat difficult, in which in 87% of cases dilation of the hepaticocholedochus, lobar and segmental ducts was observed.The nature of the pathology of the liver and biliary tract had a direct impact on the frequency of manifestation of ultrasound signs of MGD.Thus, when performing ultrasound in patients with liver echinococcosis, complicated by mechanical parasitic jaundice, in 19 (12.8%) cases, a breakthrough of the hydatid cyst into the bile ducts was diagnosed (Fig. 3).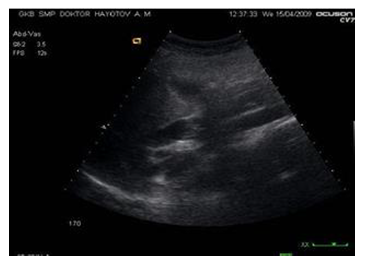 | Figure 3. Ultrasound. Breakthrough of an echinococcal cyst into the bile ducts |
In patients with the main bile duct occlusion caused by stricture of the main bile ducts, ultrasound made it possible to identify the causes of their occurrence (Fig. 4) and the level of obstruction.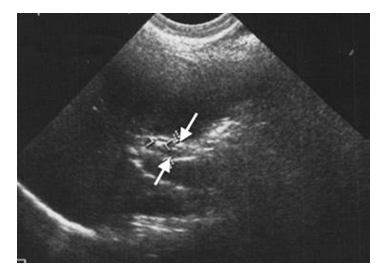 | Figure 4. Ultrasound. Extension of the upper third of the AKI, stone in the area of suprastenotic extension |
According to abdominal ultrasound, signs of Mirizzi syndrome were suspected in 5 patients with the main bile duct occlusion. These were patients with Mirizzi syndrome type II (Fig. 5). | Figure 5. Ultrasound. SM type II. Dilated common hepatic and lobar ducts and a large calculus is detected in the proximal parts of the common bile duct |
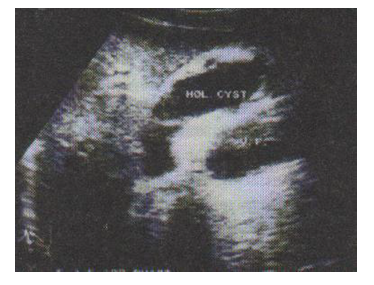
In case of cystic lesions of the liver and bile ducts, ultrasound allowed us to effectively diagnose the disease in 5 cases. In the projection of the anatomical course of the common bile duct, a cystic formation was identified, part of which were the walls of the duct (Fig. 6).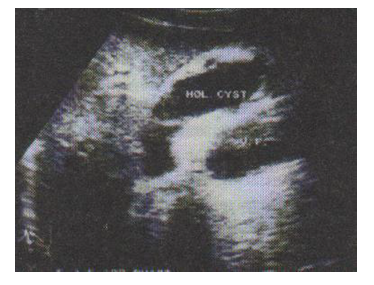 | Figure 6. Ultrasound. Common bile duct cyst |
Cystic dilation of the extrahepatic bile ducts ranged from 1.5 cm to 10 cm in diameter (average diameter 48 mm). Intrahepatic and/or extrahepatic choledocholithiasis was noted in 2 patients.Characteristic ultrasound signs of biliary pancreatitis were heterogeneity of the echostructure of the pancreas and parapancreatic tissue, changes in the contours and size of the pancreas, the presence of fluid accumulations in its structure, an increase in the diameter of the common bile duct more than 8 mm, and choledocholithiasis. Chronic indurative pancreatitis in 3 cases was the cause of the main bile duct occlusion in the patients we observed (Fig. 7). | Figure 7. Ultrasound. Choledocholithiasis. Biliary pancreatitis. Changes in echogenicity and the presence of microliths in the pancreatic parenchyma (A). Dilatation of the main pancreatic duct against the background of an enlarged head of the gland - indurative pancreatitis (B) |
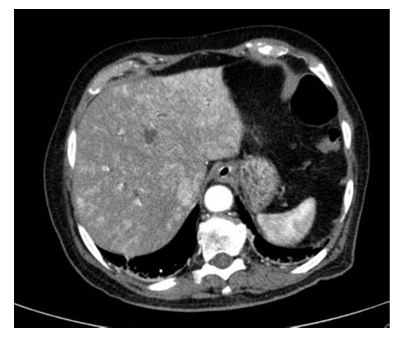
Currently, a highly informative way to verify the causes of biliary duct obstruction and interstitial bile duct is CT, multislice computed tomography using bolus contrast enhancement, as well as magnetic resonance imaging (MRI) and magnetic resonance cholangiopankeatography (MRCP).Computed tomography (CT) for complex diagnosis of the main bile duct occlusion was performed in 25 patients. Computed tomography allowed not only to determine the cause of obstructive jaundice and its localization, but also made it possible, especially with parasitic jaundice and cystic lesions, to identify the topography of cysts, the adjacency of large vascular and biliary structures, as well as clarify the condition and volume of functioning parenchyma and preliminarily determine the methods of treatment and surgical access (Fig. 8).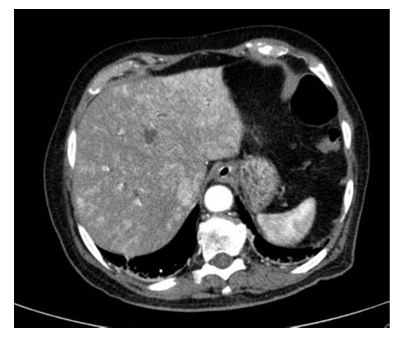 | Figure 8. CT scan. Choledocholithiasis, Purulent cholangitis |
When echinococcal cysts break through into the main bile ducts with the development of mechanical parasitic jaundice and parasitic cholangitis, along with dilation of the extrahepatic bile ducts, a decrease in the tension of echinococcal cysts in the liver was diagnosed according to ultrasound and CT in 12 cases. CT allowed in 7 cases to effectively diagnose cystic lesions of the bile ducts (Fig. 9). | Figure 9. CT scan. Formation of the wall of the dilated common bile duct in a common bile duct cyst |
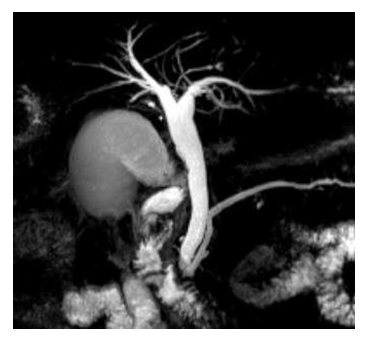
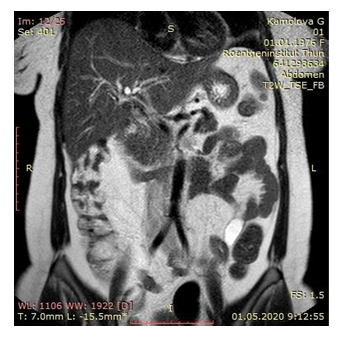
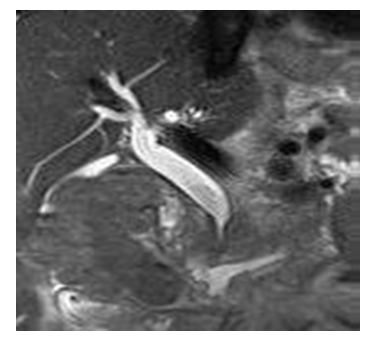
MSCT is a highly effective non-invasive method for diagnosing the main bile duct occlusion and its etiology. It allows you to accurately assess the condition of the extrahepatic bile ducts, organs and great vessels of the hepatopancreatobiliary zone. However, the effectiveness of MSCT in diagnosing cholangitolithiasis is not so high, since only in 20% of cases the stones in the ducts have intense homogeneous enhancement, and in 50% they have a strength similar to the strength of soft tissues, making it difficult to identify them.MRCP was effectively used in 68 patients with various etiological origins of MRCP. This research method makes it possible to obtain a separate image of the bile ducts and pancreatic ducts during MRCP in combination with the standard MRI protocol; the accuracy of diagnosing biliary block of non-tumor origin is up to 98%, and therefore MRCP is a safe, non-invasive alternative to ERCP. A significant advantage of MRCP over ERCP is the ability to visualize the ducts before and after the site of their obstruction, as well as the ability to assess the structure of the organs of the hepatopancreatoduodenal zone.In case of multiple choledocholithiasis, which occurred in 18 patients (2 or more), stones were identified in the lumen of the common bile duct (Fig. 10, 11). | Figure 10. MRCP. Dilated common bile duct with many stones. Gallbladder stones |
 | Figure 11. MRCP. Concretion of the distal common bile duct |
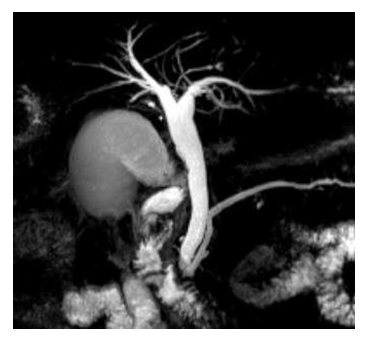
The use of three-dimensional MRI and MRCP made it possible not only to identify stones in the biliary tract, to assess their number and probable composition, but also to recreate a three-dimensional virtual image of the biliary tree, to identify the features of its structure and relationships with neighboring anatomical structures in 12 cases.MRCP made it possible in 14 cases to diagnose a complex of stones in the distal common bile duct, as well as the presence of a cicatricial stricture of the BSD (Fig. 12).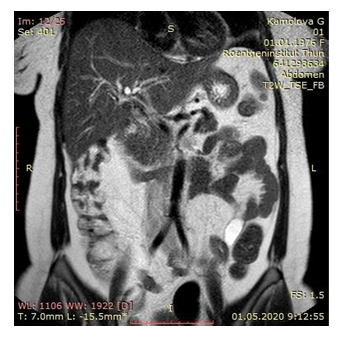 | Figure 12. MRCP. Stones in the lumen of the hepatic duct (hepatolithiasis) |
The reasons for the development of the bile ducts obstruction can be very diverse, including cicatricial strictures of the bile ducts. In our studies, to identify the extent of strictures and their causes, a special place was given to MRCP, which was performed in 12 patients (Fig. 13, 14).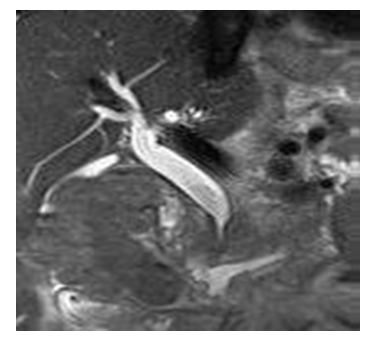 | Figure 13. MRCP. Stenosis of the terminal bile duct. Dilatation of intra- and extrahepatic bile ducts. Main bile duct occlusion |
 | Figure 14. MRCP. Extended stricture of the terminal part of the common bile duct. Chronic indurative pancreatitis |
A special group consisted of patients with postoperative jaundice, the main causes of which in all observations were technical and tactical medical errors. To diagnose them, MRCP was performed in 4 cases (Fig. 15).  | Figure 15. MRPHG. Postoperative jaundice. Block of the common bile duct. Damage to the common hepatic duct |
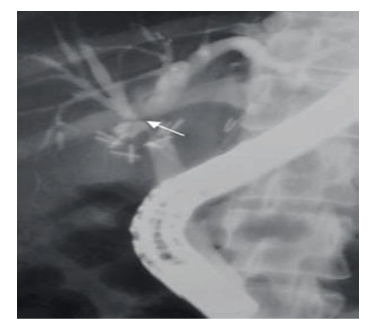
Thus, modern non-invasive no radiation methods for diagnosing main bile duct occlusion are a highly informative method for diagnosing the causes of its occurrence.ERCP in the present study was performed in 102 patients with MGD in the main group.Dilatation of the common bile duct was detected in 92 (90.1%) patients, intrahepatic ducts in 89 (87.2%).In 59.6% of cases, according to ERCP, the diameter of the common bile duct was from 1.1 to 2.0 cm, in 26.9% it was more than 2.0 cm and in 13.5% up to 1 cm.During ERCP, in 82.4% of cases, stones of various sizes were identified in the lumen of the bile ducts.In 44.6% of cases, 1 stone was found in the lumen of the common bile duct, in 57.7% - from 1 to 3 stones, and in 61.5% - multiple choledocholithiasis. (Fig. 16, 17). | Figure 16. ERCP. Multiple choledocholithiasis |
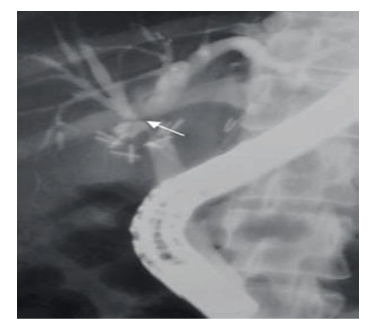 | Figure 17. ERCP. Postoperative jaundice. Presence of a metal clip in the common bile duct |
ERCP allowed us to diagnose cicatricial narrowing of the bile ducts in 10 cases, which were complicated by intravenous bile ducts (Fig. 18). | Figure 18. ERCP. Cicatricial stricture of the bihepaticojejunal anastomosis |
If it was impossible to perform ERCP (disturbance of the anatomy of the digestive tract after surgery, stenosis and diverticulum of the esophagus), as well as secondary changes in the area of the esophagus (paraesophageal diverticula), preference was given to the PCCG technique, which was performed in 11 patients with various pathological conditions of the biliary tract, contributing to the development of thebmain bile duct occlusion. PCCG - allows you to identify the cause and level of benign obstruction of the biliary tract. The main disadvantage of this method is the impossibility of cannulating the biliary tract if the bile ducts are insufficiently dilated. Also, the disadvantage of the method is its invasiveness and the risk of complications associated with transhepatic puncture of the bile ducts (bleeding, bile leakage, bile peritonitis, fistula formation), as well as intolerance to the contrast agent, disruption of the blood coagulation system.It should be noted that PCCG was performed to diagnose the causes of the main bile duct occlusion caused by choledocholithiasis, cicatricial strictures of the bile ducts, as well as in cystic diseases of the liver and biliary tract (Fig. 19, 20). | Figure 19. HCHG. Stricture of the common bile duct “0” |
 | Figure 20. FCHG. Stricture of the common bile duct “-1” |
Carrying out a complex multifactorial differentiated diagnosis of the main bile duct occlusion and its causes using radiation and instrumental research methods made it possible to develop a diagnostic algorithm for the main bile duct occlusion, which allows one to quickly establish the cause, level and localization of benign mechanical obstruction and choose a pathogenetically substantiated method of treatment.According to the developed diagnostic algorithm, all patients undergo transabdominal ultrasound. Regardless of the presence or absence of biliary hypertension, patients undergo non-invasive radiological examination methods depending on the level of obstruction (CT, MRI, MRCP). If non-invasive radiological diagnostic methods are ineffective, an invasive study of PCCG and ERCP is performed.
5. Conclusions
The main reasons for the development of MGD in 48.11% of cases are cholelithiasis in combination with choledocholithiasis and in 3.7% - cholelithiasis complicated by the development of Mirizzi syndrome, in 18.39% - stenosis of the duodenum, in 7.07% of cases - cicatricial strictures of the bile ducts, in 11.32% - parasitic (echinococcal) jaundice, in 5.66% of cases - biliary and pseudotumorous pancreatitis, in 2.35% - common bile duct cysts, and in 0.94% of cases - duodenal ulcer with penetration into the BDS and common bile duct, as well as postoperative jaundice - in 2.35% of cases. Diagnosis of MGD should be comprehensive using a developed diagnostic algorithm, including modern non-invasive radiation methods (ultrasound, MRCP) diagnostics, as well as invasive puncture and endoscopic diagnostics (RPCG, PCCG) with a transition to decompression of the biliary tract (73.64% of patients with the main groups).Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
References
| [1] | Abdurakhmanov D. S. et al. Analysis of surgical treatment options for different types of mirizzi syndrome // Bulletin of Science and Education. – 2021. – №. 5-1. – С. 71-76. |
| [2] | Abdurakhmanov D. S., Rakhmanov Q. E., Davlatov S. S. Clinical questions extreme currents syndrome Mirizzi // Electronic Innovation Bulletin. – 2021. – №. 6. – С. 37-40. |
| [3] | Babajanov A. S. et al. Results of surgical treatment of acute cholangitis and its Consequences // Journal of Problems of Biology and Medicine. – 2018. – No. 1 (99). – P. 23-26. |
| [4] | Babajanov A. S. et al. Surgical tactics for cholelithiasis with complications of obstructive jaundice // Journal of Problems of Biology and Medicine. – 2017. – No. 2 (94). – P. 22-24. |
| [5] | Davlatov S. S. et al. Plasmopheresis in the treatment of cholemic endotoxicosis // Academic journal of Western Siberia. – 2013. – Т. 9. – №. 1. – P. 30-31. |
| [6] | Davlatov S.S., Kasymov Sh.Z., Kurbaniyazov Z.B., Azimov R.R. A new method of detoxification plasma by plasmapheresis in the treatment of endotoxemia with purulent cholangitis// “The Academic Journal of Western Siberia” - 2013. - No. 2(45). - Volume 9. - Р. 19-20. |
| [7] | Davlatov S.S., Kurbaniyazov Z.B. New method plasmapheresis in the treatment of cholemic endotoxicosis// Problems of biology and medicine. – 2015. - № 4. (85). - P. 175-176. |
| [8] | Gafurovich N. F., Babajanovich K. Z., Salim D. Modified method of plasmapheresis in the treatment of patients with purulent cholangitis //European science review. – 2018. – №. 7-8. – P. 142-147. |
| [9] | Kasymov S. Z., Davlatov S. S. Hemoperfusion as a method of homeostasis protection in multiple organ failure syndrome // Academic journal of Western Siberia. – 2013. – Т. 9. – №. 1. – P. 31-32. |
| [10] | Nazirov F. G., Kurbaniyazov Z. B., Davlatov S. S. Modified method of plasmapheresis in the treatment of patients with purulent cholangitis// European Sciences review Scientific journal. – 2018. - № 7–8. (July–August) - P. 142-147. |
| [11] | Rakhmanov K. E., Davlatov S. S., Abdurakhmanov D. S. Diagnosis and treatment of Mirizzi syndrome // Questions of science and education. – 2020. – №. 13. – С. 97. |
| [12] | Sulaymonovich D. S., Yormonovich K. N., Babajanovich K. Z. Complex treatment of purulent cholangitis //British Journal of Science, Education and Culture. – 2014. – С. 214. |
| [13] | Toirov A. S., Babajanov, A. S., Bobomuradov, B. M., Axmedov, G. K. Tactics for cholelithis disease with complications of obstructional jaundice // Science and World. – 2019. – T. 3. – No. 5. – P. 62-64. |














 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML