-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(1): 133-138
doi:10.5923/j.ajmms.20241401.30
Received: Dec. 12, 2023; Accepted: Jan. 5, 2024; Published: Jan. 26, 2024

Intraoperative Determination of Muscle Vitality at the Level of Amputation in Patients with Diabetic Foot Syndrome
Khamdamov Bakhtiyor Zarifovich1, Davlatov Salim Sulaymonovich1, Rakhmanov Kosim Erdanovich2, Tulezhanov Nurpeis Kudaibergenovich3
1Bukhara State Medical Institute, Bukhara, Republic of Uzbekistan
2Samarkand State Medical University, Samarkand, Republic of Uzbekistan
3International Kazakh-Turkish University named after Khoja Ahmed Yasawi
Correspondence to: Davlatov Salim Sulaymonovich, Bukhara State Medical Institute, Bukhara, Republic of Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The work analyzes the results of a comprehensive examination and treatment of 137 patients with diabetic foot syndrome who were hospitalized in the department of purulent surgery of the Bukhara Regional Multidisciplinary Medical Center in the period from 2020 to 2023. In order to assess the viability of muscle tissue at the level of amputation, the use of a rapid method of intraoperative macroscopic histochemical determination of the activity of muscle tissue dehydrogenases was proposed. Based on the study, we can conclude that there is a decrease in the activity of metabolic processes in muscle tissue during chronic ischemia in patients with diabetic foot syndrome, which is indicated by a slowdown in the formation of formazans during an intraoperative histochemical study for more than 5 minutes. It can be assumed that dystrophic, necrobiotic and inflammatory changes in the conditions of diabetic angiopathy predetermine disruption of regeneration processes and in some cases lead to the development of massive muscle necrosis in the postoperative period. The identified indicators of correlation between the results of intraoperative histochemical examination and histological signs of impaired muscle tissue viability confirm the objective nature of the intraoperative rapid test.
Keywords: Diabetic angiopathy of the lower extremities, Lactate dehydrogenase, Intraoperative histochemical study
Cite this paper: Khamdamov Bakhtiyor Zarifovich, Davlatov Salim Sulaymonovich, Rakhmanov Kosim Erdanovich, Tulezhanov Nurpeis Kudaibergenovich, Intraoperative Determination of Muscle Vitality at the Level of Amputation in Patients with Diabetic Foot Syndrome, American Journal of Medicine and Medical Sciences, Vol. 14 No. 1, 2024, pp. 133-138. doi: 10.5923/j.ajmms.20241401.30.
Article Outline
1. Introduction
- One of the most common endocrine diseases is diabetes mellitus: on average, 4-5% of the world's population suffers from it, in Russia - up to 6%, in the USA - up to 20%. More than 70% of diabetic patients develop diabetic foot syndrome. In 1987, at the Geneva International Conference on Diabetes Mellitus, "diabetic foot" was identified as an independent complication along with diabetic nephro-, ophthalmo-, neuro- and angiopathy. Much has been achieved in the field of treatment of diabetic foot lesions, but as regards the use of vasoactive drugs, there is not yet a sufficient number of studies justifying the expediency of their widespread use in practice. Nowadays there are no drugs that significantly and permanently improve the state of microcirculation and the number of patients undergoing high ampu-tations of the lower extremities due to diabetic le-sions continues to increase steadily. Trental, tradi-tionally used in such practice, can cause some un-desirable consequences ("stealing syndrome") and carries a potential risk of developing hemorrhages on the fundus in patients with diabetic retinopathy. Currently used methods of surgical and conservative treatment of such complications of diabetes mellitus as diabetic foot with necrotic lesion of the lower extremities at various levels do not always allow to achieve stabilization of the process, are quite expensive and often difficult to perform. The drugs used for topical treatment mainly have a narrowly targeted effect: antimicrobial, dehydrating, non-political, improving the regulatory process. However, they do not provide a comprehensive effect on the wound process as a whole.The increase in the incidence of diabetes mellitus predicted by WHO experts worldwide makes it urgent to search for new, effective and cost-effective methods of treating patients with diabetic foot syndrome. In recent years, the method of ozone therapy has been successfully used in various fields of medicine. Ozone has a positive effect on carbohydrate and lipid metabolism, improves the oxygen transport function of blood, eliminates microcirculatory disorders, including due to its positive effect on the rheological properties of blood, and also actively affects the processes of lipid peroxidation and the antioxidant protection system, optimizes reparative processes in wounds. Recently, methods of topical application of ozone and ozone-saturated sodium chloride saline solution for active drainage of wounds, in which only low concentrations of ozone were used, have become increasingly important in the local treatment of patients with diabetic feet. The intraosseous route of drug administration has long been recognized as one of the most effective. However, there are isolated publications on the intraosseous administration of ozonated saline solution. Currently, almost the entire frequency range of electromagnetic oscillations is used in the diagnosis, treatment and prevention of various diseases. Simultaneous exposure to magnetic, infrared and laser radiation as therapeutic factors improves reparative processes in wound tissues and increases the effectiveness of treatment by about 1.5 times. At present, technologies for the integrated use of ozone, both local and intraosseous in the form of ozonized solutions, magneto-infrared laser radiation, with combined topical application of complex ozone therapy and magneto-infrared laser radiation in various phases of the wound process in patients with purulent necrotic form of diabetic foot syndrome have not been fully developed.Thus, there is every reason to turn to the scientific study of this issue.
2. The Purpose of the Study
- To determine intraoperatively the viability of muscles at the amputation level in patients with diabetic foot syndrome.
3. Materials and Methods of Research
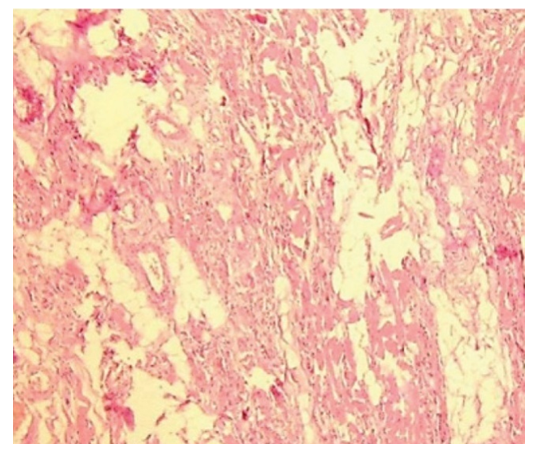
- The paper analyzes the results of a comprehensive examination and treatment of 137 patients with diabetic foot syndrome (DFS) who were hospitalized in the department of purulent surgery of the Bukhara Regional Multidisciplinary Medical Center in the period from 2020 to 2023.Patients underwent ultrasound Dopplerography and color duplex vascular mapping of the lower extremities, X-ray of the foot. The state of carbohydrate metabolism was monitored in the laboratory. Wound healing was assessed according to laser Doppler flowmetry.In order to assess the viability of muscle tissue at the amputation level, we proposed the use of an express method of intraoperative macroscopic histochemical determination of the activity of dehydrogenases of muscle tissue.In the operating room, according to the standard procedure described above, the limb was amputated at the initially selected, as high as possible, level. After crossing the muscle arrays with a scalpel, muscle biopsy was performed at the expected amputation level, the thickness of the sections was about 3-6 mm.During amputation at the hip level, the external broad and semimembranous muscles were examined, during surgery below the knee joint - the calf, flounder and anterior tibial muscles. After manufacturing a suitable biopsy with a cross-section of muscle fibers, it was incubated in a mixture of 0.02% solutions of nitrosine tetrazolium and 1M lactate solution at a temperature of 43°C. At this stage, the temperature regime was strictly observed. The acidity required for the reaction (pH=7.2-7.4) was achieved by using a phosphate buffer. Accordingly, the time for which the first and second stages of the reaction were manifested was taken into account. V1 corresponded to the time of the first reaction, V2 – the time of the end of the reaction. The initial changes began to occur in the first or second minute in the form of staining of individual fibers, then in the period from 3 to 10 minutes, depending on the degree of ischemia. This process can take up to 10 minutes. The course of the reaction was recorded in photographs. The initial stage of the reaction is presented – the formation of formazane in individual muscle fibers in the second minute of the study (Fig. 1).
 | Figure 1. The type of muscle biopsies in the course of IHCE (initial stage): 1. m. gastrocnemius: 2. m. tibialis anterior |
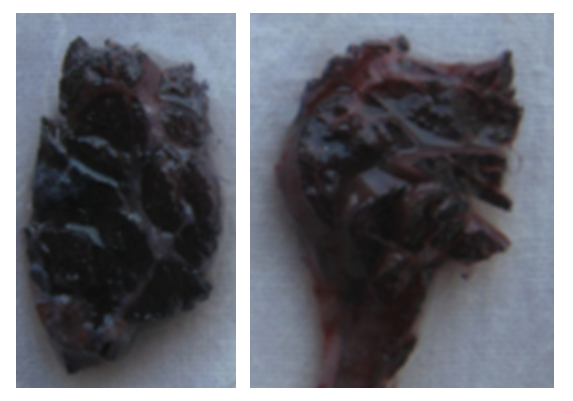 | Figure 2. The type of muscle biopsies in the course of IHCE (the final stage): 1. m. gastrocnemius: 2. m. tibialis anterior |
 | Figure 3. Karyorexis (karyolysis) |
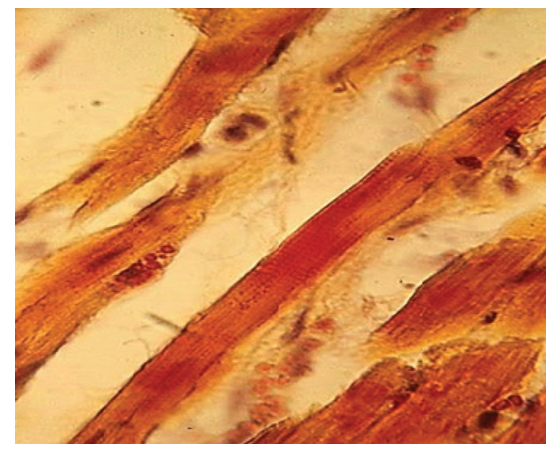 | Figure 4. Contractural damage |
 | Figure 5. Necrosis and edema |
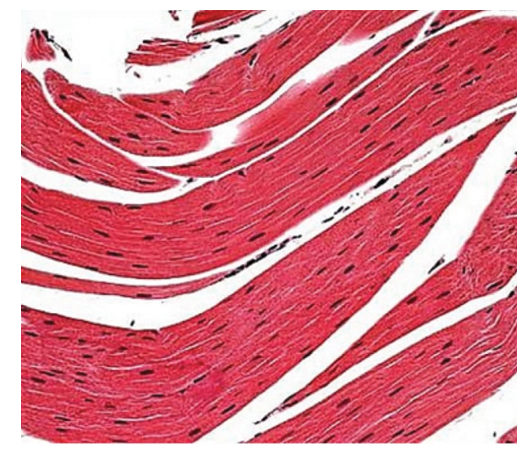 | Figure 6. Normal |
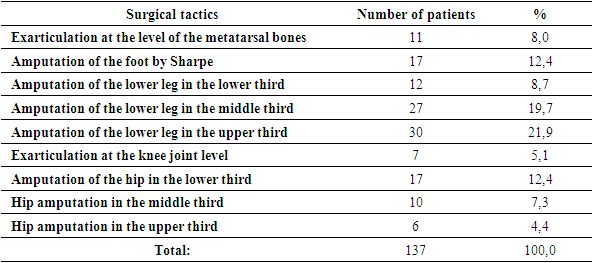
4. The Results of the Study
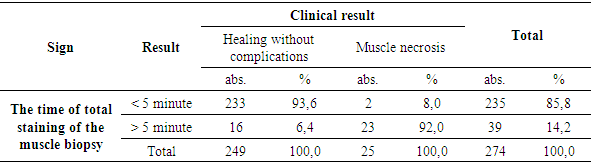
- Intraoperative histochemical examination of the activity of lactate dehydrogenase in muscle tissue was used by us as an objective criterion of tissue viability for the final determination of the level of limb amputation and the method of stump formation in 137 patients with SDS.When the lower limb was truncated, the tissue condition was determined using both traditional tissue viability criteria and an intraoperative macroscopic histochemical rapid test. Based on this assessment, in 28 (20.4%) of the observed cases, a decision was made on the possibility of preserving the ankle joint, in 69 (50.4%) amputation was performed at the knee level, in 7 (5.1%) exarticulation was performed at the knee level and in 33 (24.1%) amputation at the hip level is complete.The informativeness of intraoperative methods for assessing tissue viability was assessed by the clinical result - the presence of necrosis of the stump muscles in the early postoperative period, leading to impaired healing of the surgical wound. It should be emphasized that in this study we did not take into account early postoperative complications unrelated to ischemic necrosis of the stump muscles, such as postoperative hematomas, marginal necrosis of the skin, superficial suppuration of the postoperative stump wound, unrelated to muscle necrosis, etc.The healing of the postoperative wound of the stump by the type of primary tension, as we believed, indicated the absence of significant necrosis of the stump muscles.We studied the results of the assessment of the intraoperative condition of 206 muscles.With the development of postoperative necrosis, in most cases, during ligation, it was not possible to determine the anatomical affiliation of the altered stump muscle. Therefore, when establishing the fact of postoperative necrosis, we limited ourselves to stating the localization of necrotic changes in the anterior or posterior muscle groups.As an intraoperative criterion for the viability of muscle tissue in patients with DFS, we used the method of rapid assessment of the activity of lactate dehydrogenase of muscle tissue by reaction with nitrosine tetrazolium developed at the Department of Faculty and Hospital Surgery of the Bukhara State Medical Institute.To determine the effectiveness of this technique, we studied its informative value for predicting the development of early local postoperative complications, in particular postoperative necrosis of the stump muscles.According to our data, the total staining time of a fragment of a viable muscle was < 5 minutes. Slower formation of formazanes indicated a marked decrease in redox processes in muscle tissue, which led to impaired regeneration processes and caused the development of clinically significant necrosis of the stump muscles.In this study, the informativeness of intraoperative histochemical examination (IHC) was studied and compared with traditional criteria for intraoperative assessment of the viability of muscle tissue.The dependence of the clinical outcome of the operation on the intraoperatively determined activity of lactate dehydrogenase of muscle tissue is presented in Table 1.
|
|
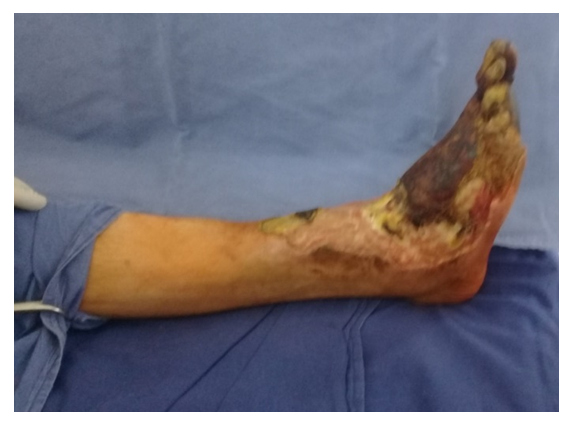 | Figure 7. Type of limb of patient K. Diabetic foot syndrome, extensive trophic ulcer of the right shin. IHCE: m. gastrocnemius – 4,5 min, m. soleus – 6,5 min., m. tibialis ant. – 5 min |
5. Conclusions
- The intraoperative histochemical express method for determining the activity of lactic acid dehydrogenase of muscle tissue at the amputation level in patients with diabetic foot syndrome is a highly informative method for assessing tissue viability, demonstrating sensitivity of 94.7% and specificity of 94.1%. The revealed correlation indicators of the results of IHC and with histological signs of impaired viability of muscle tissue confirm the objective nature of the intraoperative express study of the activity of lactate dehydrogenase of muscle tissue.An intraoperative rapid study of the activity of lactate dehydrogenase of muscle tissue at the amputation level (IHCE) is an informative objective criterion for the final choice of the amputation level and the method of stump formation in patients with DFS. The use of IHCE made it possible to perform amputation at a more distal level in 29.1% of patients and reduce the number of early postoperative complications due to necrosis of the stump muscles.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML