-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(1): 110-114
doi:10.5923/j.ajmms.20241401.25
Received: Dec. 27, 2023; Accepted: Jan. 19, 2024; Published: Jan. 23, 2024

Intraoperative Surgical Hemostasis Tactics in Case of Combined Injuries of Parenchymal Organs Abdominal Cavity
Umedov Xushvaqt Alisherovich
Assistant of the Department of Surgical Diseases No. 2, Samarkand State Medical University, Uzbekistan
Correspondence to: Umedov Xushvaqt Alisherovich, Assistant of the Department of Surgical Diseases No. 2, Samarkand State Medical University, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In recent years, there has been a steady increase in injuries around the world. Man-made and natural disasters, local military conflicts, transport and industrial accidents in 50-60% of cases of all injuries lead to combined and multiple damage to the organs and systems of the human body, and, as a result, to high sanitary losses in the first hours and days. The main problem is the diagnosis and treatment of a combined closed abdominal injury, accompanied by shock against the background of massive intraperitoneal bleeding in case of liver and spleen injuries. Hospital mortality in this variant of pathology ranges from 17.3 to 72.7%. Currently, the issues of surgical treatment tactics of spleen and liver injuries are not fully resolved. The search for optimal options, as well as technical advancement of organpreserving operation techniques involving parenchymal organs, remains relevant. This depends on the structural features of these organs, availability of the methods of local hemostasis listed in this paper and surgeon's knowledge and manual skills. Moreover, at present, hemostatic application agents are widely introduced into clinical practice, parenchymal bleeding caused by superficial planar injuries of parenchymal organs being the main indication for the use of these agents.
Keywords: Liver injury, Modeling, Parenchymal organ, Abdominal surgery, Clinical surgery, Bleeding
Cite this paper: Umedov Xushvaqt Alisherovich, Intraoperative Surgical Hemostasis Tactics in Case of Combined Injuries of Parenchymal Organs Abdominal Cavity, American Journal of Medicine and Medical Sciences, Vol. 14 No. 1, 2024, pp. 110-114. doi: 10.5923/j.ajmms.20241401.25.
1. Introduction
- In recent years, there has been a steady increase in injuries worldwide. Man-made and natural disasters, local military conflicts, transport and industrial accidents in 50-60% of cases of all injuries lead to combined and multiple damage to organs and systems of the human body, and, as a result, to high sanitary losses in the first hours and days. [1,2]. The main problem is the diagnosis and treatment of combined closed abdominal trauma, accompanied by shock against the background of massive intra-abdominal bleeding with damage to the liver and spleen [3,4]. Hospital mortality in this variant of pathology ranges from 17.3 to 72.7% [6].The urgency of the problem, according to [5,7], is due to the continued growth of combined abdominal trauma, while a large number of complications (45.7-69.9%) and high mortality (16.2- 69.5%), according to the authors, are associated with the lack of rational generally accepted surgical tactics for damage to parenchymal organs [9,10].In blunt abdominal trauma, liver damage occurs in 10 to 17% [8,11].Among the closed injuries of the abdominal organs, ruptures of the spleen account for 16-30% [9,10,12].According to the literature, liver injury in abdominal injuries is observed in 56.0-66.8% of cases [10]. The complicated course of the postoperative period is noted in 37.0-45.0% of cases [12], and the level of postoperative mortality in isolated liver injuries is 30-36%, and in combined 39-44% [14]. In recent years, there has been a tendency to increase the frequency of liver damage, which is primarily due to an increase in the number of occupational injuries.
2. Methods and Materials
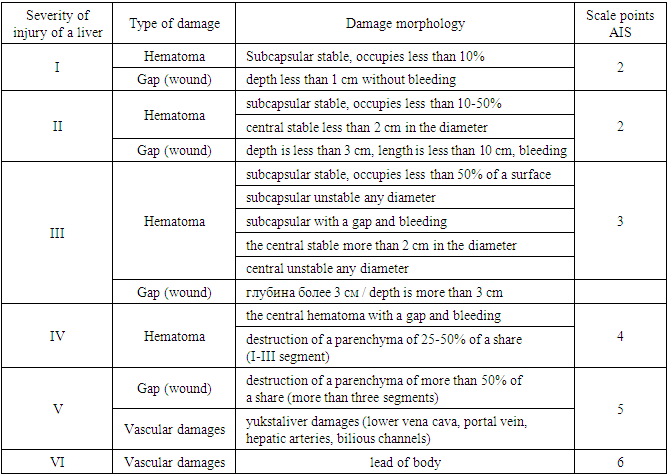
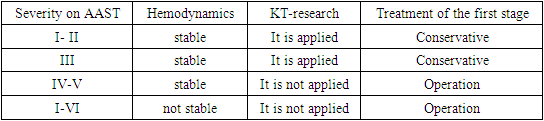
- The main cause of the unfavorable outcome of liver and spleen injuries is intra-abdominal bleeding, therefore, the choice of an adequate method of hemostasis and timely surgical intervention is of particular importance. The survival rate of patients operated on within 2 hours from the moment of injury to parenchymal organs is 85%; in those operated on within 6 to 12 hours is 23%, and in those operated on after 12 hours, the survival rate is random. The surgeon's tactics in case of damage to parenchymal organs is determined by the nature of their injuries and should be aimed primarily at ensuring effective hemostasis. Diagnosis of liver and spleen damage is difficult due to the polymorphism of the symptoms of parenchymal lesion and requires a large number of examination methods for a comprehensive assessment of the severity of the patient's condition. Thus, a FAST diagnostic protocol based on the assessment of the presence/absence of fluid in the abdominal cavity by ultrasound has been developed and introduced into clinical practice, computed tomography is also used, and the Moore formula and the Algover shock index are used to assess the volume of blood loss. In cases where contact with patients is difficult due to the severity of his condition, combined trauma (chest injury, severe fractures of the pelvic bones and / or spine, coma with traumatic brain injury, when clarification of complaints and anamnesis is impossible, and the mechanism of injury does not exclude the possibility of damage to the abdominal organs), the implementation of invasive diagnostic techniques such as diagnostic video laparoscopic (DVL) revision of the abdominal cavity. Of course, indications for DVL are not limited to the above list of conditions, they also include penetrating wounds of the anterior abdominal wall in the absence of indications for laparotomy; blood loss of less than 500 ml of blood, etc. [14,15]. Modern clinicians are guided by the classification of parenchymal organ injuries, adopted in 1994 by the American Association of Surgeons and Traumatologists - American Association for the Surgery of Trauma (AAST), supplemented by an abbreviated injury scale - Abbreviated Injury Scale (AIS), which was developed earlier (in 1971) as a method for quantifying and comparing various types damage to parenchymal organs (Table 1) [16].
|
|
3. Results
- In case of spleen injuries of I and II degrees of severity of damage on the AAST scale [20], he considers conservative management and angioembolization to be the most optimal ways to achieve hemostasis. According to the author, in case of damage to the spleen gate, more than three damage to peripheral vessels, damage to more than 50% of the organ parenchyma, proximal embolization should be resorted to, and in case of single damage to peripheral vessels, distal embolization is sufficient [19]. Performing splenoraphy for the purpose of hemostasis encounters significant difficulties due to the eruption of sutures with the development of even more bleeding. In this regard, various methods of strengthening the stitches were used. In particular, a strand of a large omentum, various plastic materials, including a hemostatic sponge, were used as a lining material for splenoraphy. In some cases, the wound was closed with a plastic material that was fixed to the surface of the damaged spleen with a catgut mesh. These methods of hemostasis in spleen injuries of 4 degrees of severity of liver and spleen injuries and for each degree offered its own version of hemostasis. The severity of the liver injury was determined taking into account the degree of damage: I – superficial wounds up to 2 cm deep, II – wounds from 2 cm deep to half the entire thickness, III – wounds more than half the thickness of the organ and through tears. In case of injuries of I-II degree, wounds were sutured with hemostatic U-shaped sutures made of absorbable material to the full depth. Hemostasis of injuries with grade II and III ruptures was performed by ligation of the right renal vessels and tamponade of the wound. The artery was ligated if its temporary compression led to cessation or a significant decrease in the intensity of bleeding. For grade I spleen injuries, the Tachocomb collagen sponge was used and reliable hemostasis was achieved, and for grade II and III injuries, splenectomy should be performed to achieve hemostasis, followed by autotransplantation of spleen tissue into the large omentum.With superficial tears of the liver of the I class of damage, according to the AAST classification, it is enough to apply a collagen sponge "Tachocomb", with deep ruptures with damage to the liver parenchyma, U- or Z-shaped suturing should be applied, only with absorbable suture material (catgut or vicryl), with extensive damage of the III class, the sutures described above can be applied and in addition you can apply a gauze tamponade of the "cigar" type. The collagen plate "Tachocomb" has proven itself in case of surface tears spleen of class I, and in case of extensive damage of class III, splenectomy is advisable [20]. The method of hemostasis in case of combined damage to the liver and spleen. The essence of the method is as follows. After laparotomy and evacuation of blood from the abdominal cavity, splenectomy is performed according to general surgical rules. The liver wound is preemptively tamponed with a hemostatic sponge, then a wedge-shaped graft, identical in size to the liver wound, is cut out of a less damaged fragment of the removed spleen. The peripheral part of the graft is not decapsulated. To achieve hemostasis in case of ruptures of the spleen, along with its suturing, ligation of segmental lobular arterial vessels is also possible, if necessary, with fixation (frenolyenopexy, gastrolienopexy). In case of deep ruptures, along with suturing, external compression of the organ can be used to achieve final hemostasis. In subcapsular hematomas with damage to the parenchyma of the organ, preference should be given to minimally invasive methods of treatment. In case of crushed wounds and ruptures located along the edge of the organ, in the area of the poles and occupying an entire lobe or segment, it is recommended to perform atypical resection of the corresponding area. Splenectomy with implantation of splenic fragments is indicated for deep wounds in the area of the gate, multiple ruptures of the spleen. Intraoperative methods of stopping bleeding in elective surgery of parenchymal abdominal organs.In case of planned organ-preserving operations on the liver for oncological diseases, one of the key methods of surgical treatment is extensive liver resection (ORP). However, ORP is a high-risk operation due to the occurrence of massive intraoperative bleeding. ORPS are usually divided into anatomical (typical) and atypical. In anatomical liver resection, an indispensable point of the surgery technique is the ligation of the main vessels and ducts in the portal and caval gates of the liver, and the separation of the liver parenchyma itself is performed in low-vascular zones (lobectomy, segmentectomy, hemihepatectomy). Atypical resections are performed without strict consideration of the intraorgan architectonics of vessels and ducts, without preliminary ligation of the vascular secretory pedicle and the main point is the hemostatic suture. Anatomical liver resection is currently considered the standard of liver surgery, as it reduces the risk of massive blood loss, damage to the main vascular structures of the opposite lobe of the liver, and also avoids sequestration of the liver parenchyma.In case of ruptures of the spleen along the diaphragmatic surface, it is necessary to pinch the vascular pedicle before application and hold it for the entire period of fixation. Splenectomy is recommended for hemostasis of central ruptures of the spleen. Separately, we will consider the use of such a method as electrocoagulation (diathermocoagulation), which is widely used by practicing surgeons for virtually any type of bleeding (especially parenchymal) due to its accessibility and effectiveness. However, the use of electrocoagulation has negative consequences for the injured organ, as it causes additional damage to the parenchyma and causes the development of inflammation in the area of contact of the coagulator branches and organ tissues, despite the pronounced hemostatic effect. In the postoperative period, the formed scab, due to its fragility, can collapse or deform due to the presence of peristalsis or contact with nearby organs, as well as become the basis for the formation of intra-abdominal / organ abscesses and, as a result, this can lead to a deterioration in the prognosis for the patient.
4. Conclusions
- The intraoperative stopping of bleeding from parenchymal organs of the abdominal cavity (liver, spleen) is a difficult task for a surgeon. This is due to the peculiarities of the structure of these organs, it depends largely on the availability of the methods of local hemostasis listed in this article and the degree of mastering the manual skills of the surgeon. Hemostatic applicative agents (implants) are also being widely introduced into clinical practice, the main indication for the use of which is mainly parenchymal bleeding caused by superficial planar injuries of parenchymal organs. In such cases, additional suturing of the organ tissue is not required, hemostasis is achieved by applying implants. In cases with operations that injure parenchymal organs (such as hemihepatectomy), when there is a significant area of bleeding parenchyma, the use of such drugs is also an important part of surgery, but rather refers to an additional technique, rather than the main method of stopping bleeding. In case of closed abdominal injuries and subsequent therapeutic measures aimed at providing effective surgical hemostasis, it remains important to have special local hemostasis agents in a medical institution, such as a collagen plate, a hemostatic sponge, etc. The choice of the technology of this hemostasis should be determined by the intraoperative situation and be strictly personalized.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML