-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(1): 94-98
doi:10.5923/j.ajmms.20241401.22
Received: Dec. 6, 2023; Accepted: Dec. 22, 2023; Published: Jan. 17, 2024

Analyses of the Path of a Somatic Patient with Mental Disorders
Shakhnoza Sh. Magzumova1, Nigina B. Mukhamadieva1, 2
1Department of Psychiatry and Narcology, Tashkent Medical Academy, Tashkent, Republic of Uzbekistan
2Department of Psychiatry, Narcology and Medical Psychology, Bukhara State Medical University, Bukhara, Republic of Uzbekistan
Correspondence to: Nigina B. Mukhamadieva, Department of Psychiatry and Narcology, Tashkent Medical Academy, Tashkent, Republic of Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Improving the training of internists, as well as specialists in the primary medical network in the field of diagnosis and treatment of mental disorders, can help increase the availability of quality psychiatric care by receiving care in a non-psychiatric medical institution. An internist faces an acute question about the effective management of a patient who has complaints not only of a somatic nature. Also of interest are the reasons why patients do not turn to a psychiatrist/psychotherapist, or why they turn to them in the later stages of the disease. This article highlights part of the authors’ scientific work on improving medical care for patients with somatopsychic disorders. The purpose of our study was to study the characteristics of the routes of movement of the examined patients in search of help. The frequency of visits and hospitalizations of patients to medical institutions, the duration of visits and treatment activities outside the hospital of the somatic clinic (before admission to the somatic hospital) were analyzed.
Keywords: Somatic patient, Psychopathological disorders, Referral route, Therapeutic measures
Cite this paper: Shakhnoza Sh. Magzumova, Nigina B. Mukhamadieva, Analyses of the Path of a Somatic Patient with Mental Disorders, American Journal of Medicine and Medical Sciences, Vol. 14 No. 1, 2024, pp. 94-98. doi: 10.5923/j.ajmms.20241401.22.
1. Introduction
- A significant increase in the number of mentally ill people in general somatic institutions indicates the relevance of creating a system of specialized care for these populations. At the same time, at present we can talk not only about a serious lag in this form of medical care, not only about low quality, but in a number of issues – about its absence at all [1,2]. The current situation is fraught with the danger of untimely identification of numerous mental disorders, which is reflected in an increase in the number of cases “neglected” in terms of diagnosis and treatment, decreased ability to work, deterioration in quality of life, and unjustified economic costs of the health service [3,4].Despite numerous attempts to develop and implement various organizational models of psychiatric care in a general somatic network, undertaken in Western countries, there is currently no common understanding of the ways and forms of implementing this task [5]. At the same time, when using foreign experience in improving mental health services, it is necessary to exercise some caution, having a good understanding of the relativity of numerical indicators, calculations and organizational charts, which, as a rule, are not comparable with the specific health conditions of countries [6,7].Difficulties in organizing specialized care for patients with mental disorders in the general somatic network are caused by a number of circumstances. The most common, “classical” models of psychiatric institutions - a psychiatric hospital and a psychoneurological dispensary - do not create favorable conditions for solving diagnostic and treatment problems for patients with erased, somatized, masked mental disorders. At the same time, models for integrating psychiatric services with various branches of medicine in healthcare have not been developed. The consequence of this is the limited information and professional contacts between doctors of general somatic institutions (territorial clinics, medical units, multidisciplinary hospitals, etc.) and specialists of psychiatric clinics, dispensaries and hospitals. The lack of integration of psychiatric and general medical services is also manifested by the increasing lack of demand for psychiatric care in its official, normative forms [8,9,10].The purpose of our study was to study the characteristics of the routes of movement of the examined patients in search of help. The frequency of visits and hospitalizations of patients to medical institutions, the duration of visits and treatment activities outside the hospital of the somatic clinic (before admission to the somatic hospital) were analyzed.
2. Materials and Methods
- To find out the reasons for late visits of patients to a psychiatrist/psychotherapist for mental disorders against the background of somatic diseases, it was undertaken to examine patients at a regional multidisciplinary hospital. The study group included 1066 patients (815 men, 851 women) with various somatic diseases, against the background of whose somatic pathology mental disorders developed. The average age of the examined patients was 50.3±15.7. During the study, the following methods were used: clinical interviewing, questioning using a special questionnaire compiled by us. The choice of research methods implied the possibility of conducting a comprehensive study of all factors that cause or contribute to the formation of mental disorders and interdependencies with somatic pathology, and therefore, first of all, clinical and epidemiological approaches were used for interdisciplinary research. All types of examination, diagnosis and treatment of patients were carried out personally by the author, in close cooperation with internists. The clinical method involved examining each patient to obtain a qualified psychopathological assessment of the patient's health status.In addition to analyzing the data obtained during interviews with patients and collecting anamnestic information, clinical observation of the subjects was carried out and a description of their mental status was carried out. The clinical examination included anamnestic data, patient complaints, and questionnaires. The main attention was paid to the timeliness of detection of mental disorders in patients with somatic pathology, the quality and effectiveness of treatment, both the underlying disease and the mental state of the patient himself.
3. Results and Discussions
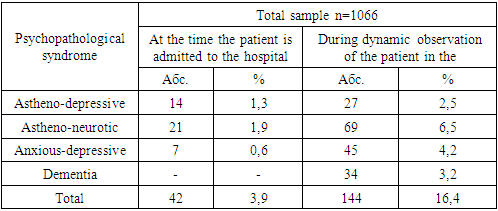
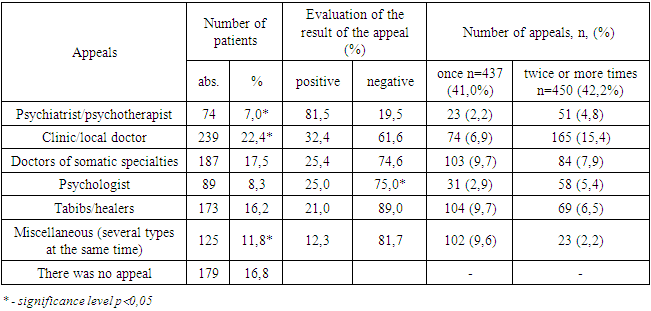
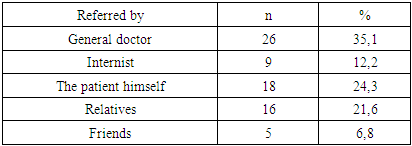
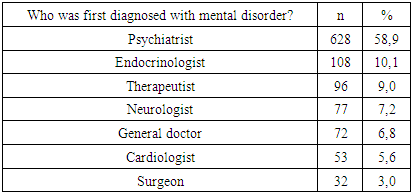
- Until now, the problem of psychological competence of somatic doctors and their awareness of the issues of diagnosis and treatment of mental disorders have not been studied in domestic medicine. In connection with the above, a study was undertaken of the professional competencies of doctors of the general somatic network in assessing the mental health of patients with various forms of somatic pathology and concomitant mental disorders.The information obtained upon admission was supplemented by observation during hospitalization, which made it possible to trace the dynamics of the mental state. Indicators of direct examination of patients were considered taking into account the entire complex of data obtained according to medical documentation. During the clinical examination, a comparison was made between the qualification of mental pathology established by the internists with the diagnosis established as a result of a subsequent psychopathological examination by a psychiatrist; Accordingly, the timeliness, adequacy, and completeness of diagnosis of mental disorders by interns in the absence of qualified psychiatric care were comparatively assessed. A comprehensive assessment of the effectiveness of prescribed psychotropic therapy was carried out. In order to verify the characteristics of the somatic condition, a full clinical and instrumental examination was carried out by an internist in accordance with modern standards to confirm the presence of a somatic disease (with an assessment of syndromes, degree/stage) or its absence.The study examined the ability of internists to recognize mental disorders in a somatic patient (table 1); assessment of doctors’ attitude towards additional study of psychiatry and possible forms of training, their readiness for it; a study of the level of doctors’ ideas about the spectrum of mental disorders in patients with somatic diseases and about methods of their treatment; studying problematic situations in the work of internists that arise when caring for patients with mental disorders.
|
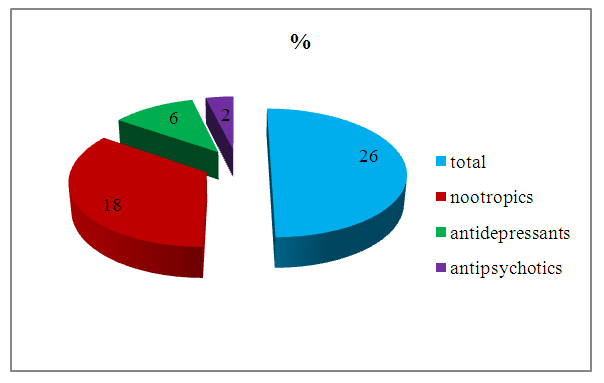 | Figure 1. Group of psychopharmacological drugs according to the list of prescriptions prescribed by attending physicians |
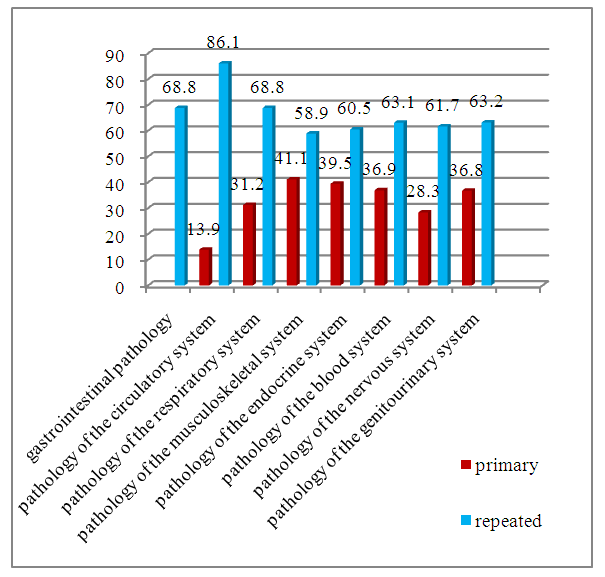 | Figure 2. Primary/repeated hospitalization rates among the examined patients |
|
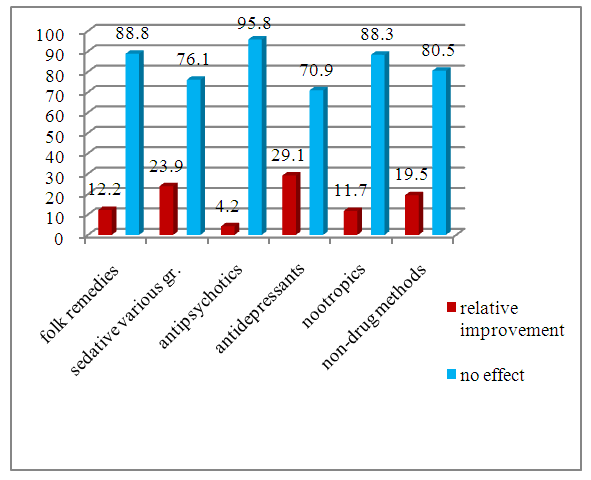 | Figure 3. Effectiveness of previous treatments as assessed by patients (%) |
|
|
4. Conclusions
- 1. Thus, an analysis of the practical activities of somatic doctors who provide medical care to somatic patients with mental disorders shows that the greatest difficulties arise when qualifying combined (mental and somatic) pathology; assessing the patient’s condition and establishing a verified diagnosis with the appropriate criteria according to ICD-10. At the same time, the choice (if psychopharmacotherapy is necessary) of psychotropic drugs adequate to the mental state, taking into account their effect on the somatic state, and their compatibility with somatotropic drugs, requires high professional competence and training from a specialist in a general somatic clinic.2. Thus, the presence of the above-mentioned problems indicates the need to change the methodology, organization, and structure of psychiatric (psychotherapeutic) care in primary health care. This circumstance indicates the need to increase the competence of clinic doctors in the field of diagnosing mental disorders, the advisability of earlier referral of patients for consultation with a psychiatrist (psychotherapist).3. It is necessary to provide primary care doctors with knowledge and skills in diagnosing psychopathological syndromes and the basics of psychopharmacotherapy. The independent professional competencies of a primary care physician should also include communication skills.4. It is advisable to empower doctors who are not psychiatrists, after special training, for example, as part of advanced training, to make a preliminary medical opinion on the state of mental health of the patients they supervise (syndromic diagnosis), and, if necessary, prescribe them psychopharmacological treatment.5. The low level of provision of psychiatric/psychotherapeutic care to patients in the primary and general medical networks is largely due to the insufficient number of psychotherapeutic rooms and psychiatrists working in them, as well as the low level of interaction between internists and psychiatrists / psychotherapists.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML