Ganiev S. Z.1, Musabaev A. N.1, Abdurakhmanov Z. M.2
1Republican Specialized Scientific and Practical Medical Center of Urology, Tashkent, Uzbekistan
2Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Abdurakhmanov Z. M., Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
One of the factors in the progression of inflammation caused by traumatic injury is the dysfunction of the immune defense, which is regulated by inflammatory mediators. Objective. To study the possibility and effectiveness of using selective spinal anesthesia during percutaneous kidney surgery. Materials and methods. In a prospective clinical study were enrolled 63 patients, who underwent percutaneous nephrolithotripsy under unilateral spinal anesthesia. Temperature, sensory and motor blockade, hemodynamic and respiratory parameters were assessed. Results. The volume of sensory and motor blockade allows the effective use of unilateral spinal anesthesia in patients undergoing percutaneous kidney surgery. A smaller volume of sympathetic blockade leads to a reduction in adverse reactions such as arterial hypotension and muscle tremors. Conclusions. When performing percutaneous kidney operations, preference should be given to unilateral spinal anesthesia, which provides adequate sensory block, the required level of motor blockade and will increase safety due to more stable hemodynamics.
Keywords:
Selective spinal anesthesia, Percutaneous kidney surgery
Cite this paper: Ganiev S. Z., Musabaev A. N., Abdurakhmanov Z. M., Selective Spinal Anaesthesia for Percutaneous Nephrolithotripsy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 1, 2024, pp. 64-68. doi: 10.5923/j.ajmms.20241401.15.
1. Introduction
Percutaneous nephrolithotripsy (PCNL) is a recognized minimally invasive method for removing kidney stones in urolithiasis. The procedure can be performed both under general anaesthesia and under spinal anaesthesia. And although regional anaesthesia for PCNL was first described in 1988 [1], there are still debates regarding the ideal method.Many studies have noted comparable effectiveness of both general and regional anaesthesia and suggest that spinal anaesthesia may be a preferable alternative in older patients with comorbidities [2,3]. In addition, problems associated with positioning are resolved because patients are conscious and can position themselves according to their comfort. However, there are reasons that limit the use of spinal anaesthesia - the risk of arterial hypotension and muscle tremors associated with sympathetic blockade after placing the patient in a prone position [4,5]. The amount of blockade (sympathetic, motor and sensory) required for this operation is clearly excessive. Arterial hypotension is almost inevitable during percutaneous nephrolithotomy, since during the action of the sympathetic blockade the operating position changes from lithotomy to the prone position [6-8]. The high risk of developing unwanted hypotension and low controllability of the height of the spinal block led to modification of traditional spinal anaesthesia and the emergence of the concept of “selective” or “unilateral” spinal anaesthesia, which, while maintaining the quality of anaesthesia, can reduce the frequency of adverse reactions [9,10]. Theoretical assumptions about the use of unilateral anaesthesia during percutaneous kidney operations have not found their justification in the literature. In the available literature, all described options for selective spinal anaesthesia concerned its use during operations on the lower extremities, groin area, and perineum.
2. Materials and Methods
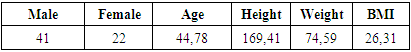
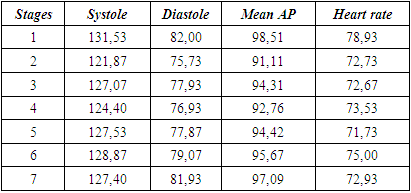
The study design is prospective.The work used clinical observations of the Department of Anaesthesiology and Intensive Care of the State Institution "Republican Specialized Scientific and Practical Medical Center of Urology". Study patient inclusion criteria:1. Surgical intervention – PCNL;2. Use of spinal anaesthesia during PCNL surgery;3. The patient’s consent to spinal anaesthesia;4. Age from 18 to 75 years;5. BMI from 18 to 40 kg/m2;6. ASA – no higher than class III.Exclusion criteria:1. Contraindications for spinal anaesthesia;2. Refusal of the patient from SA;3. BMI > 40 and < 18;4. ASA > Class III;5. Chronic renal failure terminal stage;6. Violation of the research protocol.The studies were performed in 63 patients who underwent PCNL under unilateral spinal anaesthesia. Patient characteristics are presented in Table 1. Table 1. Clinical characteristics of patients (n = 63)
 |
| |
|
Initial physical status was assessed according to the ASA classification.During the study, anthropometric data, type of intervention and duration of intervention, volume of infusion, need for vasopressors, frequency and nature of complications or adverse reactions were recorded. In the studied patients, after unilateral spinal anaesthesia, the development of temperature, sensory and motor blocks on both sides was studied. Temperature blockade was assessed using the ice test (“Cold” test), sensory blockade was performed using the “pin-prick” test (loss of pain sensitivity of the skin in response to irritation with a needle). The duration of sensory anaesthesia was determined by the occurrence of the first pain sensation of 3 or more points on a 10-point digital rating scale. The onset of development, maximum segmental level, duration, and reverse development were assessed. To assess motor blockade, the F.R. Bromage scale was used: 0 – ability to move in the hip, knee and ankle joints; 1 – ability to move only in the knee and ankle joints; 2 – ability to move only in the ankle joint; 3 – inability to move in all three joints (complete motor block). The characteristics of the motor block included determining the degree of maximum severity of the blockade, the time it was achieved and the time of restoration of motor activity. The level of pain in patients was assessed using a numerical rating scale, where 0 is no pain, 5 is moderate pain and 10 is the worst pain imaginable. Hemodynamic and respiratory parameters were recorded - heart rate, systolic blood pressure, diastolic blood pressure, mean blood pressure, saturation level (SpO2). All data was recorded from the moment the patient was placed on the operating table, at all stages of anaesthesia and surgery until the end of the surgical intervention. The stages of the study were the main points of anaesthesia and surgery: stage 1 – initial state (supine position); stage 2 – 20 minutes after puncture in the lateral position. Assessment of the sensory block began at this stage; stage 3 – supine position, retrograde ureteropyelography and ureteral stenting, stage 4 – the main stage of the operation (after turning the patient onto his stomach); stage 5 – 10 minutes after turning onto your stomach; stage 6 – 20 minutes after turning onto your stomach; stage 7 – end of the operation.Anaesthesia was administered in the lying position on the operated side. Puncture of the subarachnoid space was carried out in the midline, at the L2-3 level, with a Quincke 26G needle. After confirming that the needle was in the subarachnoid space (cerebrospinal fluid leakage), a cold hyperbaric 0,5% solution of Bupivacaine (Longocain Heavy, Yuria-Pharm), in the amount of 7,5 - 10 mg, was injected with a 2 ml syringe at a rate of 1 ml/min. An experimental study by Tomak Y [11] describing the dependence of the hydrodynamics of Bupivacaine on temperature suggested that at the temperature of the solution removed from the refrigerator (+4 - +6°C), the time from extraction to the moment of administration (5 minutes), the size of the needle (25G), needle immersion depth (7 cm) and injection rate of 1 ml/min, the temperature of the injected 0,5% Bupivacaine solution will not exceed 20°C. At a CSF temperature of 37°C and 0,5% bupivacaine at 20°C, the latter will demonstrate clear hyperbaric properties. In this regard, a cooled anaesthetic solution was used to enhance the hyperbaric effect during unilateral spinal anaesthesia. Ampoules with anaesthetic solution and syringes were kept in the refrigerator at a temperature from +4° to +6°C. After administration of the anaesthetic, the patient remained in a lateral flexed position (with legs adducted toward the abdomen) for 20 minutes. For cranial distribution of the anaesthetic from the puncture level (L2-3-4) to the Th8-10 level, after administration of the anaesthetic, the patient was positioned with the head end of the table lowered by 15°. The horizontal position of the table was returned after the spread of temperature paraesthesia to the level of Th 9-10. After 20 minutes, the patient was placed on his back in the lithotomy position for the first stage of the operation [12-14].
3. Results and Discussion
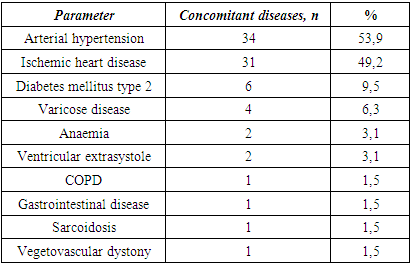
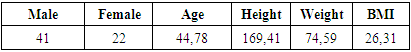
During anaesthesia, three patients were excluded from further study. One patient had technical difficulties in reaching the subarachnoid space, and therefore the operation was performed under general anaesthesia. Two patients had difficulty performing puncture of the subarachnoid space on the side. In the sitting position, the puncture was successful and they underwent conventional spinal anaesthesia. Thus, the study protocol was fully completed in 60 patients. The nature of concomitant pathology is presented in Table 2.Table 2. Concomitant pathologies (n = 63)
 |
| |
|
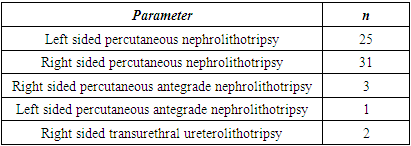
The type of surgical interventions carried out in the examined patients is presented in Table 3.Table 3. Operative characteristics (n = 63)
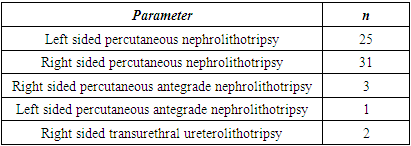 |
| |
|
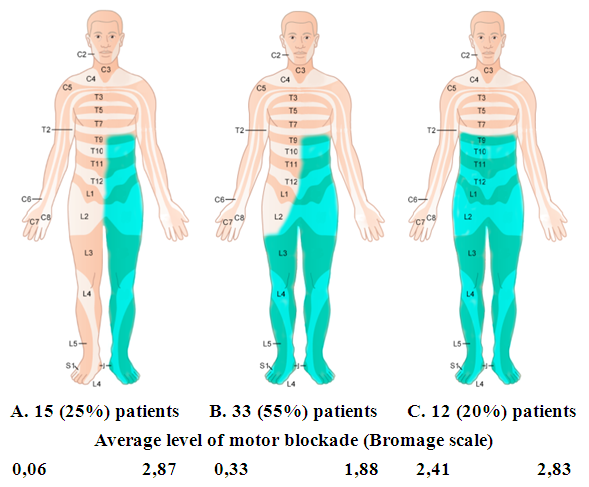
Moreover, the development of temperature paraesthesia occurred already during intrathecal administration of the anaesthetic (feeling of warmth). This feeling first affected the underlying region of the lumbar region, then spread to the entire half of the body and lower limb. A decrease in temperature sensitivity was a guideline for the spread of the blockade. During the puncture and administration of the anaesthetic, the operating table was with the head end lowered at an angle of 10 - 12 degrees. After achieving temperature anaesthesia to the level of Th 9-10, the operating table returned to a strictly horizontal position.The final level of development of temperature, sensory and motor blockade by the end of the 20-minute interval was assessed. By this time, the level of temperature anaesthesia had reached its maximum and was, as a rule, higher than the level of sensory blockade by one segment.Exclusive unilateral spinal anaesthesia was achieved in 15 (25%) patients (Figure 1A). Those. these patients showed no signs of sensory and motor blockade on the superior (“healthy”) side. The maximum level of sensory anaesthesia in these patients reached the Th 7 segment. Motor blockade also developed on the same side and reached a maximum level of 3 points in 93,3% of cases. On the opposite side, only in one case was a motor block corresponding to 1 point on the Bromage scale recorded.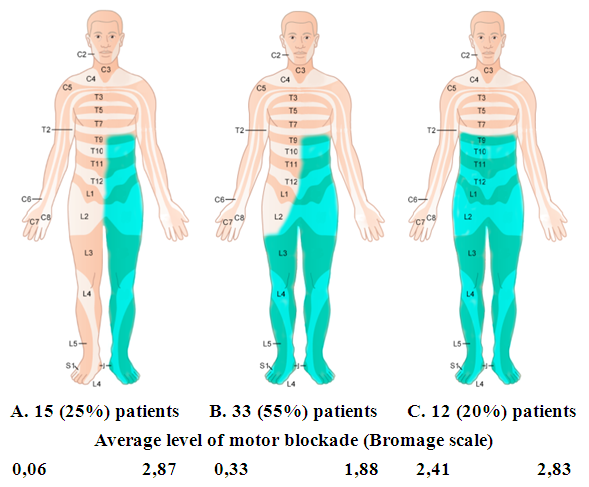 | Figure 1. Distribution of sensory anesthesia in patients of group 1 |
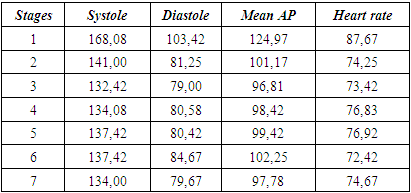
In 12 (20%) patients, anaesthesia developed according to a bilateral scenario, and although the level of sensory blockade was identical on both sides (Figure 1C), in two cases the motor block did not correspond to its level. In both described cases, on the independent (“healthy”) side it was significantly less pronounced: in one case, 0 points on the Bromage scale, in the other, 1 point.In the remaining 33 cases (55%), patients showed signs of anaesthesia on the opposite side (Figure 1B). At the same time, the maximum level of sensory blockade on the operated side reached the level of Th9 (on average Th11), and on the “healthy” side it did not exceed the level of L3-4. The motor block reached a maximum level of 3 points in 24,2% of cases, 2 points in 36,4% of cases, the average level of motor block was 1,82 points. On the healthy side, the average level of motor block corresponded to 0,33 points.Only in one case did an insufficient level of sensory blockade (Th12) force us to switch to another type of anaesthesia and complete the operation under general anaesthesia.Respiratory parameters such as respiratory rate and saturation remained stable during all stages of the study and indicated a minimal impact of surgery and anaesthesia on respiratory function. Respiratory support in the form of oxygen inhalation was required in only one case of general anaesthesia.Muscle tremors were not recorded in any case. When studying hemodynamics, it was revealed that its initial indicators (blood pressure and heart rate) were within normal limits.When studying changes in blood pressure and heart rate, a pattern was identified that was associated both with the stage of the study and the volume of sympathetic blockade. Patients who developed bilateral anaesthesia showed the most pronounced decrease in blood pressure, requiring increased infusion rates and, in rare cases, the use of vasopressors (Table 4).Table 4. Hemodynamic parameters in patients with bilateral anaesthesia
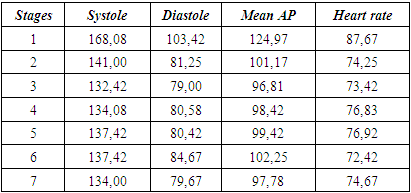 |
| |
|
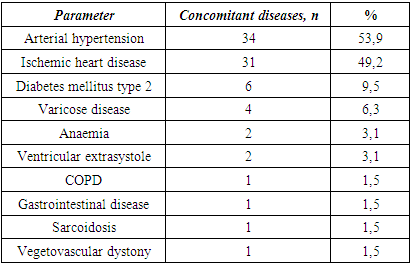
In the remaining patients in whom anaesthesia was unilateral, changes in hemodynamics were less pronounced (Table 5). The decrease in systolic and mean blood pressure did not exceed 10% of the initial level.Table 5. Hemodynamic parameters in patients with unilateral anaesthesia
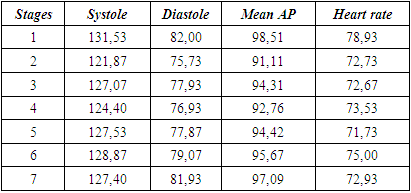 |
| |
|
4. Conclusions
Our study demonstrated that unilateral spinal anaesthesia is an effective method of anaesthesia for percutaneous renal surgery. 80% of patients successfully developed unilateral spinal anaesthesia. In almost all subjects, the level of motor and sensory blockade was maintained until the end of the operation, creating good conditions for carrying out all stages of the operation.Undesirable arterial hypotension, requiring increased infusion rates and the use of vasopressors, was more pronounced in patients with inadvertently developed bilateral anaesthesia.It is very important that to ensure sensory anaesthesia during percutaneous kidney operations, it is necessary to achieve sensory blockade of at least 9–10 thoracic segments [15]. Unilateral anaesthesia made it possible, during puncture of the subarachnoid space at the level of L2-4, to raise the level of blockade to the required level and at the same time avoid, firstly: hemodynamic disorders inherent in high spinal anaesthesia and secondly, the influence on the function of external respiration due to the motor blockade of the muscles involved in the act of breathing.As it was previously assumed [16], when performing percutaneous kidney operations, preference should be given to unilateral spinal anaesthesia, which provides adequate sensory block, the required level of motor blockade and increases safety due to more stable hemodynamics.
ACKNOWLEDGEMENTS
All authors have made significant contributions to the design, execution, analysis and writing of this study, and will share responsibility for the published material. Conflicts of interest: The authors declare no conflicts of interest.Ethics approval: This study was approved by the Institutional Review Board of both institutes, Uzbekistan.
References
| [1] | Sunana G., Rahul G., Nandita M., Arti M., Siddarth V., Rajesh M. Percutaneous nephrolithotomy under spinal anesthesia and the efficacy of adding adjuvant clonidine to intrathecal hyperbaric bupivacaine: a comparative study. The Internet Journal of Anaesthesiology. 2014; 33(1): 1-7. |
| [2] | Ballestrazzi V., Zboralski C., Smith-Morel et al. Importance of suspended peridural anesthesia in percutaneous nephrolithotomy. Apropos of 112 patients in the urology service of the Regional Hospital Center of Lille. Cahiers d’Anesthesiologie. 1988; 36(2): 85–88. |
| [3] | Sari R., Dursum M., and Pirale A. A comparison of levobupivacaine versus racemic bupivacaine in PCNL with spinal anaesthesia,” European Journal of Anaesthesia. 2010; 27: 130-132. |
| [4] | Borzouei B., Habibollah S., and Bahar M. Results of Percutaneous Nephrolithotomy under spinal anaesthesia. World Academy of Science, Engineering and Technology. 2012; 6: 5-20. |
| [5] | Mehrabi S. and Shirazi K. Results and complications of spinal anaesthesia in PCNL. The Journal of Urology. 2010; 7: 22–25. |
| [6] | Kuzgunbay B., Turunc T., Akin S., Ergenoglu P., Aribogan A., and Ozkardes H. Percutaneous nephrolithotomy under general versus combined spinal-epidural anesthesia. Journal of Endourology. 2009; 23(11): 1835-1838. |
| [7] | Atallah M., Shorrab A., Abdel Mageed Y., Demian A.D. Low-dose bupivacaine spinal anaesthesia for percutaneous nephrolithotomy: the suitability and impact of adding intrathecal fentanyl. Acta Anaesthesiologica Scandinavica. 2006; 50(7): 798–803. |
| [8] | Tangpaitoon T., Nisoog C., Lojanapiwat B. Efficacy and safety of percutaneous nephrolithotomy (PCNL): a prospective and randomized study comparing regional epidural anesthesia with general anesthesia. International Brazilian Journal of Urology. 2012; 38(4): 504–511. |
| [9] | Moawad H. El Hefnawy A. Spinal vs. general anesthesia for percutaneous nephrolithotomy: a prospective randomized trial. Egyptian Journal of Anaesthesia. 2015; 31(1): 71–75. |
| [10] | Cicek T., Gonulalan U., Dogan R. et al. Spinal anesthesia is an efficient and safe anesthetic method for percutaneous nephrolithotomy. Urology. 2014; 83(1): 50–55. |
| [11] | Tomak Y, Erdivanli B, Sen A, Bostan H, Budak ET, Pergel A. Effect of cooled hyperbaric bupivacaine on unilateral spinal anesthesia success rate and hemodynamic complications in inguinal hernia surgery. J Anesth. 2016; 30(1): 26-30. |
| [12] | Takiguchi T, Yamaguchi S, Hashizume Y, Kitajima T. Movement of the cauda equina during the lateral decubitus position with fully flexed leg. Anesthesiology. 2004; 101: 1250. 7. |
| [13] | Kulkarni S, Gurudatt CL, Prakash D, Mathew JA. Effect of spinal flexion and extension in the lateral decubitus position on the unilaterality of spinal anesthesia using hyperbaric bupivacaine. J Anaesthesiol Clin Pharmacol. 2018; 34(4): 524-528. |
| [14] | Büttner B, Mansur A, Bauer M, Hinz J, Bergmann I. Einseitige Spinalanästhesie: Literaturübersicht und Handlungsempfehlung [Unilateral spinal anesthesia: Literature review and recommendations]. Anaesthesist. 2016; 65(11): 847-865. |
| [15] | Dasgupta P., Rose F.K., Wickham J.E. Percutaneous renal surgery: a pioneering perspective. J Endourol. 2006; 20(3): 167–169. |
| [16] | Patel S.R., Nakada S.Y. The modern history and evolution of percutaneous nephrolithotomy. J Endourol. 2015; 29(2): 153–157. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML