-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(1): 24-26
doi:10.5923/j.ajmms.20241401.05
Received: Dec. 5, 2023; Accepted: Dec. 28, 2023; Published: Jan. 3, 2024

Clinical Features of Pregnancy and Childbirth in Women with Epilepsy
Zufarova Shakhnoza Alimjanovna1, Kosimhojieva Fotima Takhirovna2
1Republican Center for Reproductive Health, Uzbekistan
2Andijan State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Insufficient knowledge of the comorbidity of epilepsy in pregnant women, which stands at the intersection of neurology and obstetrics and gynecology, often causes many unfounded fears or, conversely, remains without due attention. The purpose of this article was to reveal possible complications in the mother and fetus depending on the chosen tactics of antiepileptic therapy and the individual characteristics of women in labor. Material and methods. Data from the medical records of 200 parturient women with epilepsy were prospectively studied. Factors contributing to the development of these complications and aggravating the course of pregnancy were also studied. The results of the analysis showed that the risk of complications in the fetus with monotherapy is lower than with polytherapy.
Keywords: Pregnancy, Epilepsy, Teratogenic risk, Antiepileptic drugs, Complications, Anticonvulsants
Cite this paper: Zufarova Shakhnoza Alimjanovna, Kosimhojieva Fotima Takhirovna, Clinical Features of Pregnancy and Childbirth in Women with Epilepsy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 1, 2024, pp. 24-26. doi: 10.5923/j.ajmms.20241401.05.
1. Introduction
- Epilepsy is a common, chronic and serious neurological disease, the treatment of which usually needs to be continued during pregnancy, which in itself raises concerns about the teratogenicity of the drugs used [3,6,7].Pregnancy does not usually affect the frequency of seizures in parturient women with epilepsy (PE). Although percentages vary between studies, approximately 60% of patients have a seizure frequency similar to their baseline prepregnancy seizure frequency, whereas 15% experience an increase in frequency and 15% a decrease [1,2]. If a patient has had seizures, if she is healthy for 1 year before pregnancy, it is very likely (80%) that she will continue to be seizure free during pregnancy. The incidence of status epilepticus in pregnant EC is comparable to the annual incidence of 1.6% in the general population of epileptics [4,5,8].
2. Material and Research Methods
- Under our direct supervision in the Andijan branch of the Republican Perinatal Center there were 200 women in labor with epilepsy in the period from 2020 to 2023. Conventionally, all women in labor were divided into two groups: 108 of them received polytherapy (two or more anticonvulsants), 82 - monotherapy. The main contingent of patients - 62 people (59.1%) were housewives. The age limit was 18-38 years.
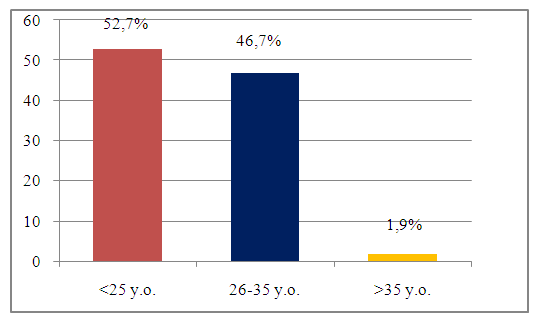 | Figure 1. Age distribution of patients receiving monotherapy |
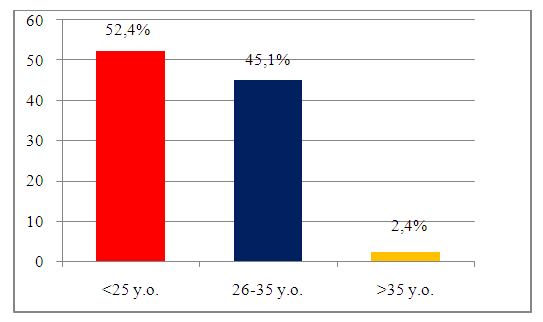 | Figure 2. Age distribution of patients receiving polytherapy |
 | Figure 3. Presence of concomitant somatic pathologies |
3. Research Results
- As complications of the use of antiepileptic drugs, we took into account low body weight, signs of chronic fetoplacental insufficiency, acute fetal hypoxia during childbirth, fetal deformities, and adynamia of newborns.Although percentages vary across studies, approximately 60% of patients have a seizure frequency similar to their baseline prepregnancy seizure frequency, while 15% experience an increase in frequency and 15% a decrease. If a patient has had seizures, if she is healthy for 1 year before pregnancy, it is very likely (80%) that she will continue to be seizure free during pregnancy. The incidence of status epilepticus in pregnant WWE is comparable to the annual incidence of 1.6% in the general population of epileptics.
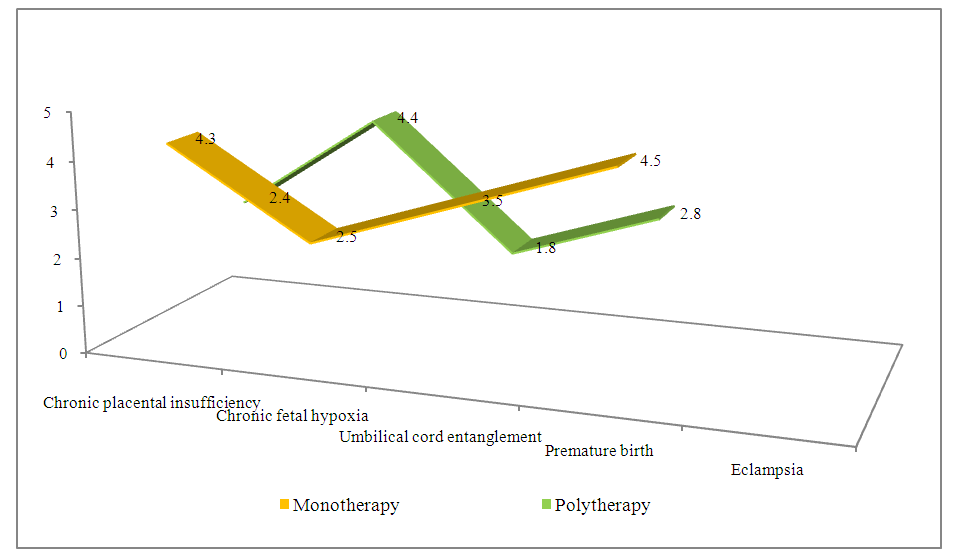 | Figure 4. Complications during labor |
4. Conclusions
- The presence of epileptic status in the mother and the use of antiepileptic drugs certainly affects the course of pregnancy and fetal development, but stopping antiepileptic therapy would, of course, be inappropriate. However, it can be noted that the risk of complications when conducting monotherapy is significantly lower than when using several anticonvulsants.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML