-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 2057-2061
doi:10.5923/j.ajmms.20231312.51
Received: Dec. 10, 2023; Accepted: Dec. 23, 2023; Published: Dec. 30, 2023

Opportunities of Endovisual Diagnostic Tools in the Management of Women with Secondary Infertility
Zokirov Farkhod Istamovich, Pardaeva Ozoda Gayratovna
Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

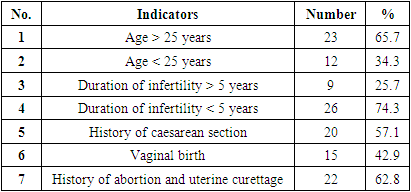
Infertility is the absence of pregnancy in a woman with regular unprotected intercourse for at least one year and today is not only a medical, but also a social problem. According to the literature data, infertility is the third most common reason for women seeking gynecological care and is observed in 186 million people worldwide. According to various authors, 10-15% of married couples suffer from infertility, 40-45% of which are due to the female factor. At the same time, the most common causes of infertility in women are tubo- peritoneal (40-50%), ovulatory dysfunction (30-40%) and uterine factors (15-20%). Aim of the study. Assessment of the role of endovisual diagnostic and treatment methods in the management of women with secondary infertility. Material and methods of the study. The study describes the results of examination and treatment of 35 women with secondary infertility. Results of the study: Of the 35 women, 19 (54.3%) had a normal hysteroscopic findings. They immediately underwent laparoscopy with chromopertubation during which in 32% cases endometriosis (pelvic adhesions), in 26% cases periadnexal adhesions and in 42% of cases peritubal adhesions were found. All of them underwent simultaneous adhesiolysis surgery. In 16 (45.7%) women out of 35, during diagnostic hysteroscopy, pathologies such as a foreign body of the uterine cavity, intrauterine synechiae, endometrial polyps, submucous uterine fibroids, and isthmocele (uterine niche) were identified and simultaneous hysteroscopic treatment was performed. Conclusions: Thus, we can conclude that today the proposed standard methods for diagnosing infertility such as hysterosalpingography and ultrasound are not always fully informative. Hysterolaparoscopy is the most acceptable method for diagnosing infertility. Moreover, these diagnostic methods make it possible to identify so-called “small forms” of lesions such as endometrial polyps, intrauterine synechiae, etc. In addition, the great advantage of this method is the possibility of simultaneous treatment with evaluation of the results ad oculus.
Keywords: Hysteroscopy, Laparoscopy, Secondary infertility
Cite this paper: Zokirov Farkhod Istamovich, Pardaeva Ozoda Gayratovna, Opportunities of Endovisual Diagnostic Tools in the Management of Women with Secondary Infertility, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 2057-2061. doi: 10.5923/j.ajmms.20231312.51.
Article Outline
1. Introduction
- Infertility is the inability to conceive after regular unprotected intercourse for at least one year and today is not only a medical, but also a social problem. It can be subdivided into primary infertility, with no prior pregnancies, occurring with a frequency of 57.5% and secondary infertility, referring to infertility following at least one prior conception, accounting remaining 42.5% of cases [1]. According to Inhorn M.C. et al. (2015) infertility is the third most common reason for women seeking gynecological care and is observed in 186 million people worldwide [3]. According to various authors, infertility affects 10-15% of married couples, 40-45% of which are due to the female factor [15,20]. At the same time, the most common causes in women are tubo-peritoneal (40-50%), ovulatory dysfunction (30-40%) and uterine factors (15-20%) [6].Today, practice shows that the proposed routine and non-invasive methods for investigation of infertility such as ultrasonography, MRT, CT, hysterosalpingography despite having some advantages, do not always satisfy the needs of doctors. These first-line diagnostic tools quite accurately determine the presence of “large lesions” of the uterus, but cannot always determine the presence of so-called “small lesions” such as polyps, synechiae and small myomatous nodules. These pathologies are better visualized using hysteroscopy in an enlarged image. During laparoscopy, in 35-68% of cases, it is possible to detect the presence of tubal pathology, endometriosis, peritubal and periadnexal adhesions, even with normal hysterosalpingogram findings [5]. At the same time, the so-called “small lesions” of the uterine cavity contribute to the disorders of the receptive properties of the endometrium and, as a result, lead to the development of infertility. Therefore, recently endovisual research methods in the diagnosis of infertility have become increasingly popular among clinicians.The advantages of ultrasound and hysterosalpingography are their non-invasiveness, relative cheapness, and they do not require high-tech equipment and highly qualified specialists. Therefore, they still remain the most widely used diagnostic methods of infertility.
2. Aim of the Study
- To evaluate the role of endovisual research and treatment methods in the management of women with secondary infertility.
3. Material and Methods of Research
- We investigated 35 women of reproductive age who applied to the department of gynecology of the Samarkand Regional Multidisciplinary Medical Center in 2022 -2023. The inclusion criteria for patients were: 1) secondary infertility 2) normal hormonal profile 3) normal semen characteristics of the husband (spermogram) 4) normal ovarian reserve 5) normal hysterosalpingography findings 6) no contraindications to hysterolaparoscopy 7) reproductive age (18- 40 years).After a complete examination and the absence of contraindications, the essence of the procedure was explained to the patients (and their spouses). In particular, patients were given detailed information that diagnostic hysteroscopy and laparoscopy would be performed simultaneously. If an intrauterine pathology is detected, diagnostic hysteroscopy will switch to therapeutic. If there are no changes on hysteroscopy, diagnostic laparoscopy will be performed simultaneously, with transition to therapeutic laparoscopy when pathology is detected. For all this, we received informed written consent with accentuation of all peculiarities of the surgical intervention.The operation was performed in the early follicular phase of the menstrual cycle under general anesthesia.
4. Results and Discussion
- The average age of respondents and the average duration of infertility were 27.8±8 and 5.3±3.6 years, respectively. Of the 35 women with secondary infertility, 20 had a history of cesarean section.Of the 35 women under investigation 19 (54.3%) had a normal hysteroscopic findings. In these women, the normal hysteroscopic findings were smooth and preserved relief of the walls of the endocervix; normal size and triangular shape of the uterine cavity, the walls of which had an even relief without deformations; the endometrium was less expressed with a pale pink color and corresponded to the phase of the menstrual cycle, did not have a pronounced vascular pattern; the ostia of the fallopian tubes were accessible for inspection on both sides and were free. These women simultaneously underwent diagnostic laparoscopy with chromopertubation.Diagnostic hysteroscopy is one of the widely used procedure for diagnosing infertility. In 16 (45.7%) women out of 35, various intrauterine pathologies were detected during diagnostic hysteroscopy (Table 1). According to various authors, in approximately 15% of infertile couples the cause of infertility is intrauterine pathology. Moreover, in almost 50% of women, during a diagnostic investigation, one or another pathology of the uterine cavity is detected [8,10,15]. Our data hardly differed from the literature data, 45.7% and 50%, respectively.
|
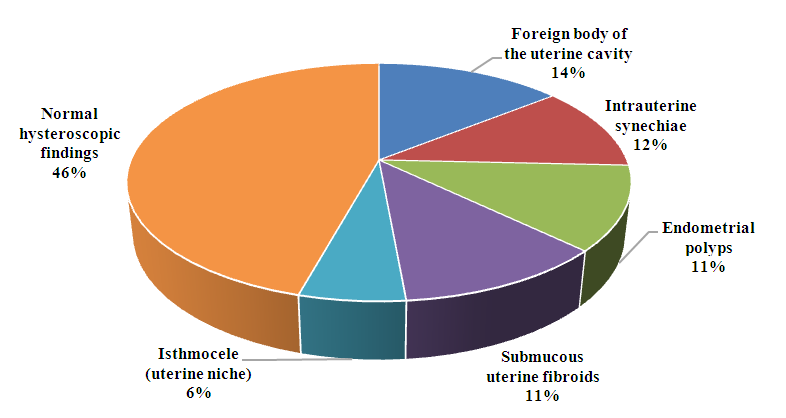 | Figure 1. Pathological findings during hysteroscopy |
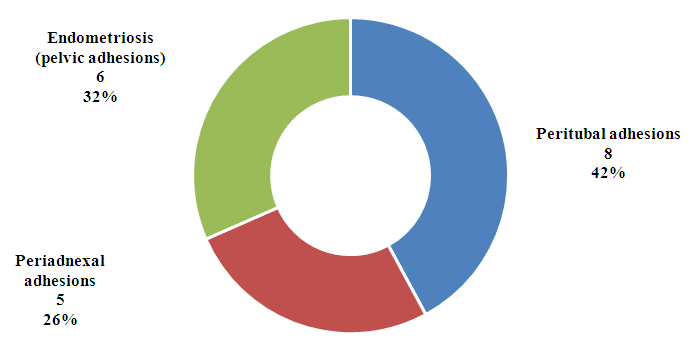 | Figure 2. Pathologies identified during laparoscopy |
5. Conclusions
- Thus, we can conclude that today the proposed standard methods for diagnostics of infertility such as hysterosalpingography and ultrasonography are not always fully informative. Hysterolaparoscopy is the most acceptable method for diagnosing infertility. Today, despite the fact that hystero- and laparoscopy are invasive interventions, the greatest advantage of these methods is the simultaneous implementation of both diagnostic and therapeutic interventions. Moreover, these invasive procedures are considered safe and the percentage of complications according to the literature does not exceed 1.65% [2] and are moderate abdominal pain. And most importantly, unlike traditional diagnostic methods, endovisual diagnostic methods help to identify so-called “small forms” of lesions such as endometrial polyps, synechiae, etc.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML