-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 2048-2052
doi:10.5923/j.ajmms.20231312.49
Received: Dec. 12, 2023; Accepted: Dec. 26, 2023; Published: Dec. 29, 2023

Features of the Psychopathological Symptom Complex in the Structure of Pathologies of the Circulatory System
Magzumova Shakhnoza Shakhzadeevna, Mukhamadieva Nigina Bakhodirovna, Hamraev Sayid Bakaevich
Bukhara State Medical University named after Abu Ali ibn Sina, Bukhara, Uzbekistan
Correspondence to: Mukhamadieva Nigina Bakhodirovna, Bukhara State Medical University named after Abu Ali ibn Sina, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In recent years, there has been more information in the scientific community about the relationship between physical and mental disorders. The nature of the development of these pathological conditions is diverse and is based on a systemic concept. To study the disorders of this circle, 103 patients were studied on the basis of a regional multidisciplinary clinic, with a diagnosis of gastroenterological and cardiological pathologies. In all the studied patients, in addition to various psychopathological signs, the state of the psycho-vegetative circle was revealed. The psycho-vegetative syndrome is a non-specific mediator and an intermediate link in the clinical formulation of symptoms, its transformation from subaffective to psychosomatic or extended affective. The nature of psychopathological symptoms was different, depending on the nosological affiliation of organ pathology. So, coronary heart disease (30%) was characterized by anxiety-phobic disorders with dysthymic saturation, in patients with hypertension, a depressed state with elements of anxiety prevailed (22%), for cardiomyopathy (28%) - hypersthenic manifestations, for heart rhythm disturbances (20%) - psychasthenic disorders. The dynamics of the components of psychosomatic disorders was interconnected with the course of the underlying disease, the development of which, of course, had a certain pattern. The diagnosis of psychosomatic disorders should be multi-axial. In this case, it should be separately stated: psychopathological syndromes and the nature of the underlying disease. The dynamics of the components of psychosomatic disorders was interconnected with the course of the underlying disease, the development of which, of course, had a certain pattern. The diagnosis of psychosomatic disorders should be multi-axial. In this case, it should be separately stated: psychopathological syndromes and the nature of the underlying disease. The dynamics of the components of psychosomatic disorders was interconnected with the course of the underlying disease, the development of which, of course, had a certain pattern. The diagnosis of psychosomatic disorders should be multi-axial. In this case, it should be separately stated: psychopathological syndromes and the nature of the underlying disease.
Keywords: Dysthymia, Psychasthenia, Psychosomatics, Clinical and pathogenetic relationships, Multidisciplinary approach
Cite this paper: Magzumova Shakhnoza Shakhzadeevna, Mukhamadieva Nigina Bakhodirovna, Hamraev Sayid Bakaevich, Features of the Psychopathological Symptom Complex in the Structure of Pathologies of the Circulatory System, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 2048-2052. doi: 10.5923/j.ajmms.20231312.49.
Article Outline
1. Introduction
- Psychosomatic relationships are one of the most complex areas of medicine. Insufficient significant progress in the field of psychosomatics is largely due to the insufficiency of the traditional psychopathological approach when considering the role of the psyche in the development and maintenance of somatic disorders [1,2].The scale of mental health problems requires a significant change in the organization of appropriate counseling and treatment care, with the development of its new forms that go beyond the traditional specialized psychiatric service, and with the combined efforts of various specialists - psychiatrists, therapists, cardiologists, neurologists, as well as psychologists and social workers. Modern psychiatry is undergoing a stage of reforms aimed at improving mental health care, ensuring its accessibility and approaching the population [3,4]. As part of the new regulations aimed at the development of psychiatric services, it is also provided developing the skills and increasing the knowledge of doctors and other medical workers of primary health care institutions on the clinical assessment, treatment and observation of persons suffering from mental disorders (Government of Uzbekistan, No.196, 2023). The obvious one is the need for interaction with the general health care system, in particular, in the form of integration of certain forms of psychiatric care into primary health care institutions [5,12,13].The attention of healthcare professionals is increasingly attracted to mental disorders associated with somatic diseases and detected in general somatic institutions. The frequency of a combination of somatic and mental disorders is a well-known fact of clinical practice, also confirmed by numerous special studies. Mental disorders can: provoke somatic diseases or, more often, their exacerbations; aggravate their course, delay recovery and, accordingly, lengthen the time of hospitalization. On the other hand, mental disorders themselves can be the result of a somatic disease - both due to the psychological reaction to the disease and the restrictions on activity associated with it, and due to possible metabolic changes or intoxication in severe somatic pathology [6,9,11].In recent years, there has been more information in the scientific community about the relationship between physical and mental disorders. The nature of the development of these pathological conditions is diverse and is based on a systemic concept. A wide range of research conducted at the intersection of a number of medical sciences, such as clinical, biological, psychological, is aimed at studying the relationship between mental and somatic processes. This problem is multifaceted and interdisciplinary in nature; it requires consideration from the standpoint of different medical sciences [7].For many years, the authors in their scientific works have provided data on the prevalence of mental disorders in the structure of somatic pathologies. According to various studies (Shepherd M., 1981; Rogers MP, et al., 1980; Snyder S. et al., 1989; Karlsson H. et al., 1995; Smulevich A.B., 1997), the number of patients with mental disorders in the general somatic network varies widely - 10-50% of all those who seek medical help. The high prevalence of mental pathology was noted both among the contingents of polyclinic institutions Lobo A., 1989; de Leon J. et al., 1987, Kozyrev V.N., 1982; Smulevich A.B., et al., 1997), and in general hospitals (Hales RE, et al., 1989; Bronheim H., et al., 1989; Charke DM, Smith GC, 1995; Kisely SR., et al., 1993; Bertolo LD et al., 1996; Prilepsky B.Yu., 1990; Drobizhev M.Yu., Pecherskaya M.B., 1994, Smulevich A.B., et al., 1999). A significant increase in the number of mental patients in general somatic institutions indicates the relevance of creating a system of integrated specialized care for these contingents.Significant prevalence of mental disorders (especially somatoform, dissociative, dysthymic and depressive disorders) during the life reaches 30% in the general population. This figure is significantly higher among people with a variety of medical conditions, such as acute or chronic response to severe illness, suboptimal adjustment to hospitalization or disability, side effects of pharmacotherapy, hormonal and metabolic changes [8,10,14]. In all likelihood, doctors of all specialties have at least a few patients with mental disorders that are either unrelated or secondary to the disease itself. These disorders can often significantly reduce the quality of life, the results of treatment and rehabilitation (Dominika Dudek, Jerzy A. Sobanski, 2013).
2. Purpose of the Study
- The aim of our research was to study of clinical features of mental disorders in somatic diseases of a cardiological nature. To achieve the goal, tasks were defined, such as a comparative analysis of the clinical course of somatic pathology and the nature of the psychopathological picture in patients of the general somatic sphere, as well as optimization of methods for diagnosing psychosomatic disorders.
3. Materials and Methods
- To study disorders of this range, 103 patients (66 men, 37 women) were studied on the basis of a regional multidisciplinary clinic, with a diagnosis of cardiac pathologies. Clinical, pathopsychological methods were used to confirm the mental status of the patient. Has also been used The Giessen Somatic Complaint Inventory arose from the need for physicians to have a standardized list of physical complaints. However, the Psychosomatic Questionnaire (PSQ) is not a list of symptoms that can be used to identify an organic disease. For this purpose, the list of complaints should be much more detailed and have a specification for a particular disease picture. The field of application of PSQ is different - we are talking about psychosomatic conditioning or interdependence of physical ailments. (Soldatkin V.A. Clinical psychometrics, 2018).Statistical processing of the obtained data was carried out using the Statistica 10.0 Windows application package. The significance of differences between the means was assessed by Student. Differences were considered statistically significant at p<0.05.
4. Results and Discussion
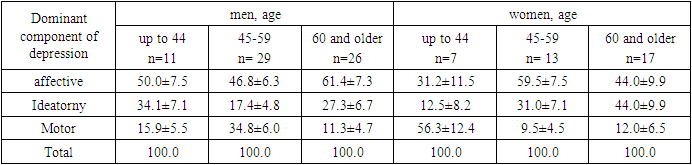
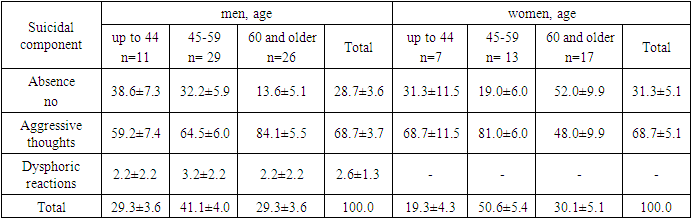
- In all the studied patients, in addition to various psychopathological signs, the state of the somatovegetative circle was revealed. Somatovegetative syndrome is a non-specific mediator and an intermediate link in the clinical presentation of symptoms. The nature of psychopathological symptoms had a different character, depending on the nosological affiliation, course and dynamics of organ pathology. So, for coronary heart disease (29.1%, 30 patients) were characterized by anxiety-phobic disorders with dysthymic saturation. This condition was manifested by symptoms such as uncontrollable fear arising in a specific situation or when interacting with a specific object, avoidance of a situation or object that causes panic attacks, fear of anticipation. Moreover, the expectation of a phobic situation was accompanied by premature anxiety, as well as vegetative reactions in the form of palpitations, dizziness, nausea, sweating, and weakness. In patients with hypertension, a depressed state with elements of anxiety prevailed (27.2%, 28 patients), for cardiomyopathy (22.3%, 23 patients) — hypersthenic manifestations. At the same time, violations such as increased nervous excitability, reactivity, irascibility, there were problems with sleep. Heart rhythm disorders (21.4%, 22 patients) were characterized by psychasthenic circle disorders, which manifest themselves as high level personal anxiety, anticipation of danger exaggerated feelings of inferiority, (the feeling of inferiority is expressed in timidity, shyness, shyness, indecision, anxious suspiciousness, cowardice, a tendency to doubt, self-doubt).The course of the components of psychosomatic disorders had a regular development. These components of the disorder had a psychosomatic and somatopsychic influence on each other, respectively, forming a vicious circle. At the acute stage, the structure of the psychopathological symptom complex was dominated by asthenic disorders, which were supplemented by neurosis-like symptoms, reflecting the premorbid accentuation of the patient's personality. There was also a persistent, syndromologically formed neurosis-like symptomatology, which forms a "facade" of a kind of masked depression.Among the study group, more than half of the patients (51,3%) noted in themselves, more often than other symptoms, a permanent decrease in mood, i.e. in these patients, an affective component of depression was manifested, while the ideator component of depression, which manifested itself in mental retardation, was noted to one degree or another in 27,5% of patients, motor retardation (motor component) was detected in 21,2% of patients. The frequency structure of the triad of symptoms of depression among the patients examined by us was almost the same both among men and among women, with a slight prevalence of the ideator component among females than among males (30.2% of patients and 25.8%, respectively, p>0.05). In general, there were no significant differences in the clinical picture of depressive syndrome in terms of the severity of one or another component among men and women. However, the analysis of these indicators among the latter in the age aspect revealed a more interesting picture (table 1).
|
|
5. Conclusions
- A group of patients suffering from somatic pathology, in particular pathologies of the circulatory system, express complaints specific to this disease, which are characterized by a general emotionally colored intensity. The diagnosis of psychosomatic disorders should be multi-axial. At the same time, it should be separately stated: psychopathological syndromes and the nature of organ pathology. An assessment of the nature and severity of the psychosocial stress factor, the level of the patient's social adaptation will provide additional important information for describing the mental status of the somatic patient.The use of an integrative approach as a basic one in the study of psychosomatic pathology leads to an understanding of this pathology and the development of effective methods for its treatment.Thus, for the majority of patients with a somatic clinic, the very fact of the presence of severe somatic disease is the cause of the development of affective disorders, in particular, dysthymic disorders, among which anxious depressions are more common. The comorbidity of somatic pathology and depression leads to a decrease in the ability to work and activity of patients. If a mild or moderate depressive episode is detected in a patient, a consultation with a psychiatrist is necessary in a planned manner for an agreed decision on the appointment of adequate therapy. In the future, it is necessary to make clinical observation and use methods to determine the depth of depression. This can be done on a daily basis by a ward doctor with the possibility of calling a psychiatrist if necessary. If a severe depressive episode is detected in a patient, an urgent call to a psychiatrist is necessary, and this patient is supervised by a consultant. In this case, it is necessary to assess the severity of a depressive episode using clinical observation and scales. With the reduction of symptoms and the acquisition of the features of a mild or moderate depressive episode, it is permissible to observe only a cardiologist, a consultant psychiatrist is called only if necessary and to coordinate therapy.The organization of advisory psychiatric care in somatic hospitals that meets modern requirements, as well as the development of educational programs in clinical psychiatry and psychopharmacotherapy for internists, are of great importance.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML