-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 2032-2039
doi:10.5923/j.ajmms.20231312.46
Received: Dec. 5, 2023; Accepted: Dec. 23, 2023; Published: Dec. 28, 2023

Cardiac Rehabilitation of Patients with Coronary Heart Disease Undergoing Aortocoronary Bypass Surgery
Kilichev A. A.
Samarkand Medical University, Samarkand, Uzbekistan
Correspondence to: Kilichev A. A. , Samarkand Medical University, Samarkand, Uzbekistan.
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In Uzbekistan the incidence of coronary heart disease continues to be stably high fluctuating between 240-400 people per year per 100 000 adult population, but lethality from coronary heart disease has a steady downward trend from 324.1 to 260.4 patients per year per 100 000 adult population, by 2020 lethality decreased by 19.7%. The proposed complex adequate personalized program of cardiac rehabilitation and School of coronary patients at the outpatient-polyclinic stage is highly effective, increases self-control of compliance with doctor's prescriptions and health improvement lifestyle. It is an effective secondary prevention of coronary heart disease, as it improves lipid spectrum, reduces total cholesterol, normalizes body mass index of patients, improves quality of life and increases socialization of patients.
Keywords: Ischemic heart disease, Morbidity, Mortality, Disability, Cardiac rehabilitation
Cite this paper: Kilichev A. A. , Cardiac Rehabilitation of Patients with Coronary Heart Disease Undergoing Aortocoronary Bypass Surgery, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 2032-2039. doi: 10.5923/j.ajmms.20231312.46.
1. Relevance
- The most frequent pathology of cardiovascular system is generally recognized ischemic heart disease, also this disease is the leader in lethality among cardiovascular diseases – 46,8% of patients with cardiovascular diseases [5,13]. Globally, coronary heart disease kills about 3 million people annually, with more than 1/3 of them being young working-age population, and this number is increasing every decade, which gives this problem a socio-economic connotation [18]. The World Health Organization cites data on 690 million people in the world over 65 years of age for 2020 with coronary mortality among this age group of 50 million annually [14]. In Russia, 9,385,000 people died of cardiovascular diseases in 2020, of which 5,087,000 died of coronary heart disease and 581,000 died of myocardial infarction [3]. Economic damage from cardiovascular diseases in Russia in 2020 reached 3.8% of gross domestic product, what is almost the entire annual health care budget, but this is also due to the scarcity of health care funding in Russia (4.6% of the budget), so in Sweden 9.3% of the budget is allocated annually for health care, in Japan – 9.2%, in Germany – 8.9%, in Norway - 8.6%, the USA – 8.5% [3]. Direct medical costs of coronary heart disease in Europe and the USA reach about 40-50% of the total economic damage, 50-60% - indirect economic losses of the state [16,20]. In the structure of direct medical costs for cardiovascular diseases on a global scale, the costs of inpatient care – 60%, doctors – 13%, drugs at the outpatient stage – 7%, home therapy – 4%, visits and monitoring of patients by nursing staff at home – 16% [23]. In Uzbekistan, the total economic losses due to myocardial infarction amount to more than 30 billion soums annually, with only 18.6% being direct medical costs and 81.4% being indirect economic losses [8]. The colossal economic damage due to cardiovascular diseases with extremely poor funding of health care causes the growth of economic damage, which requires the search for the most cost-effective methods of treatment of these pathologies [19,22]. The increasing occurrence and prevalence of coronary heart disease, the tremendous mortality and economic losses due to the decline in productivity and provision of medical care dictate the need to find effective prevention, treatment and rehabilitation measures for patients with coronary heart disease [21]. In the USA aortocoronary bypass surgery is performed on 180 patients out of 1 million, in European countries on average 360 patients, in Sweden – 777 per 1 million [15], in Russia the annual number of aortocoronary bypass surgeries exceeds 3000 and increases from year to year [7]. [15], in Russia the annual number of aortocoronary bypass operations exceeds 3000 and increases from year to year [7]. In Uzbekistan during the second decade of the new millennium the number of aortocoronary bypass surgeries increased fivefold due to the growing number of operations in an increasing number of institutions – the increase amounted to 26% over 5 years [2,4].The results of studies by foreign scientists are practically not extrapolated to Uzbekistan due to differences in the principles of financing of medical institutions, methods and availability of insurance medicine, sources of medicines, etc. It is also a problem to medico-economic analysis of treatment of non-working patients, for example, after 65 years of age, and the frequency of such interventions is increasing annually. Despite the preservation of the basic principles, the methods of cardiac rehabilitation in the new millennium have changed significantly - dynamic monitoring is optimized by the latest objective methods and scientifically unsubstantiated restrictions are removed, the widespread use of psychophysiological rehabilitation of patients [17,22]. In the Russian Federation, the duration of inpatient cardiac rehabilitation after aortocoronary bypass surgery, in the absence of complications of the operation, is 10-19 days, depending on the medical institution. Further cardiac rehabilitation is possible in the department of a specialized cardiological sanatorium, followed by lifelong secondary prophylaxis, which often turns into only outpatient dispensary monitoring by a district doctor with cardiologist consultations if necessary [1,6,11,12]. The main reasons for insufficient patient participation in cardiac rehabilitation are poor awareness of doctors, social workers, nurses, and patients who have undergone myocardial infarction or aortocoronary bypass surgery about the need for cardiac rehabilitation and its programs, which causes low patient interest, the labor intensity of various cardiac rehabilitation programs in terms of volume and duration, and the significant economic component of cardiac rehabilitation [9,10,25,26]. There are no data on medical and economic efficiency of cardiac rehabilitation carried out in Uzbekistan, as well as on the level of economic costs for its implementation, but in the context of world experience its high costliness and huge labor intensity of highly qualified medical personnel are known, which casts doubt on the expediency of prolonged cardiac rehabilitation in our country, taking into account the sharply increasing in this case health care costs and not known socio-economic effect. This all substantiates the relevance of the present study, the purpose of which was to determine the main indicators of morbidity, disability and mortality from ischemic heart disease in Uzbekistan, to assess the effectiveness of cardiac rehabilitation of patients with ischemic heart disease who underwent aortocoronary bypass surgery.
2. Material and Methods
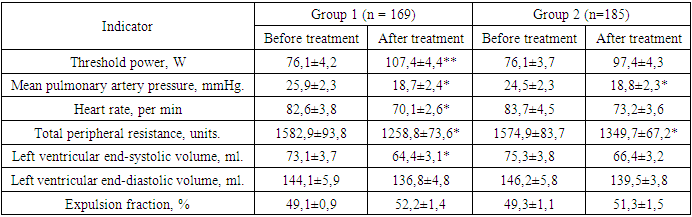
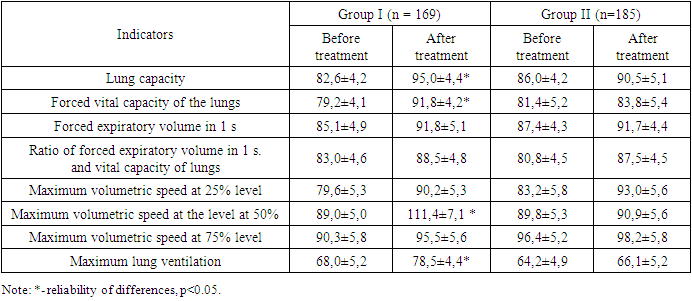
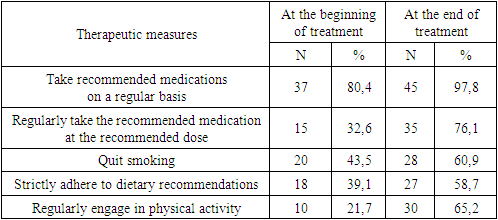
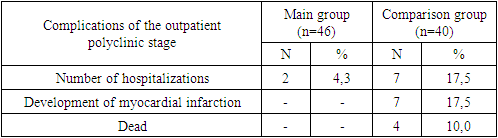
- We studied 354 patients after aortocoronary bypass surgery, aged 40-65 years, (mean age 53.7±5.1 years) hospitalized on days 12-27 for cardiac rehabilitation. Clinical efficacy of cardiac rehabilitation was evaluated in all studied patients and in a comparative aspect between two groups - Group I included 169 patients who performed >75% of the planned cardiac rehabilitation activities, Group II included 185 less active patients. Three-stage rehabilitation system (hospital, late hospital and sanatorium stages) was used for 86 patients who were admitted to the outpatient and polyclinic stage of cardiac rehabilitation on average on the 59th day after surgery, from which we formed two groups - the main group of 46 patients after aortocoronary bypass surgery, who underwent outpatient cardiac rehabilitation with inclusion of therapeutic physical training and passing the "School of coronary patients" and the comparison group of 40 patients after aortocoronary bypass surgery who did not undergo the outpatient stage of cardiac rehabilitation. All patients were treated with standard medical therapy – antithrombotic therapy, hypolipidemic therapy, as well as prevention of heart failure progression, development of heart rhythm disorders and maintenance of optimal blood pressure [24]. We performed general clinical, laboratory, radiologic and functional methods of investigation.
3. Results of the Study
- Information on the incidence and prevalence of ischemic heart disease and its consequences in the Republic of Uzbekistan is based on the data on demand for medical care, which are reflected in the relevant lines of the state statistical reporting form of the Ministry of Health of the Republic of Uzbekistan. Morbidity, on the one hand, characterizes the prevalence of diseases in the population, on the other hand - the availability of medical care, including preventive care.
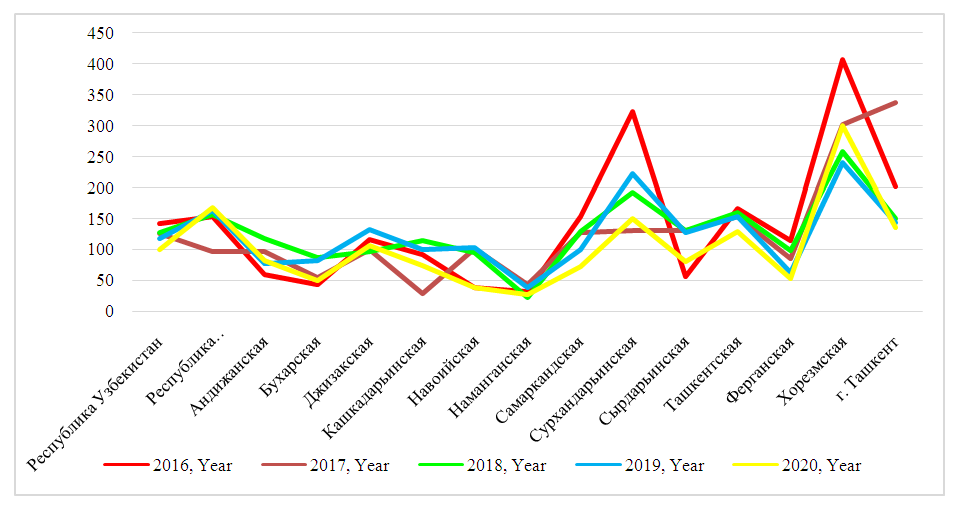 | Figure 1. Average annual primary incidence of coronary heart disease per 100,000 inhabitants in the regions of Uzbekistan in 2016-2020 years |
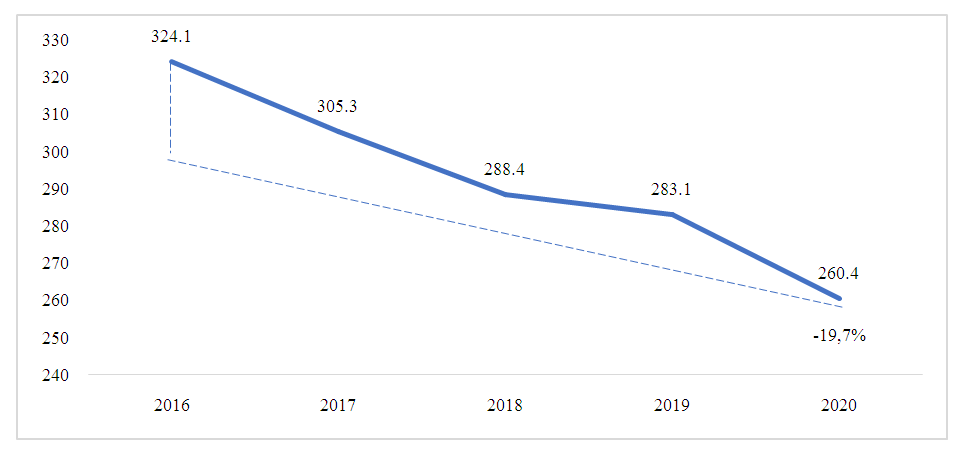 | Figure 2. Dynamics of mortality from ischemic heart disease per 100,000 population |
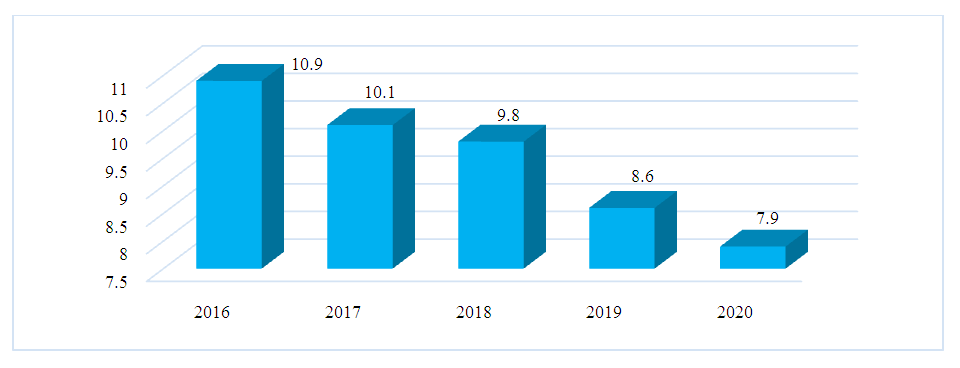 | Figure 3. Primary disability among the adult population of Uzbekistan due to ischemic heart disease in 2016-2020 (per 10,000 population) |
 | Figure 4. Share of primary disability among the adult population of Uzbekistan due to ischemic heart disease in 2016-2020 by groups (%) |
|
|
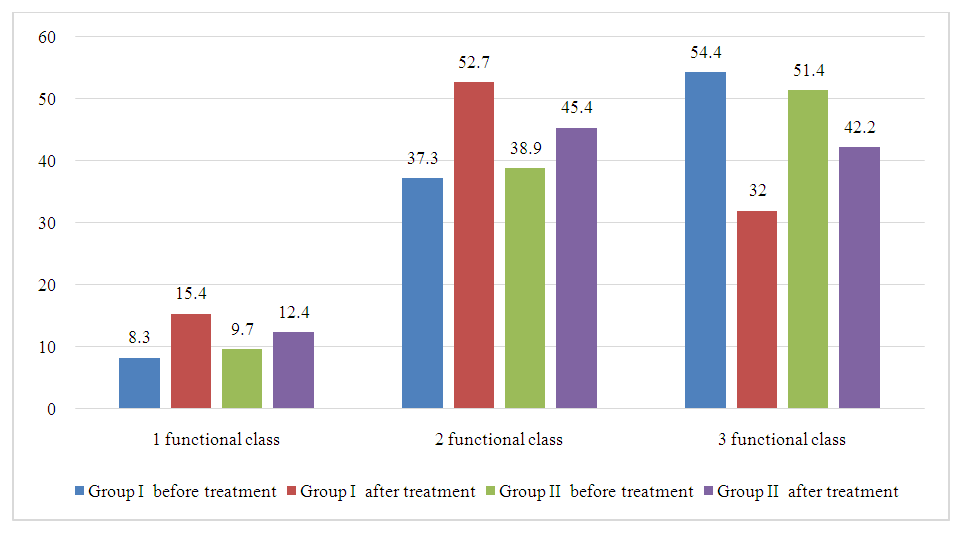 | Figure 5. Redistribution of patients' functional class, % |
|
|
4. Conclusions
- 1. In Uzbekistan, the incidence of coronary heart disease continues to be stably high, ranging from 240-400 per 100,000 adults per year. 2. Due to the competent health care reforms carried out in Uzbekistan, the mortality rate from ischemic heart disease has a steady downward trend from 324.1 to 260.4 patients per 100,000 adults per year; by 2020, the mortality rate has decreased by 19.7%. 3. In 2021, the number of patients with acute myocardial infarction was 59,280, but only 22.9% of them received inpatient treatment in specialized institutions, which cannot but alarm the cardiology service of the Republic of Uzbekistan. 4. Primary disability among the adult population of Uzbekistan due to ischemic heart disease is decreasing every year, for 2016-2020 decreased by 27.5%, from 10.9 to 7.9 per 10,000 adults, also from year to year there is a clear trend to reduce the number of disabilities of groups 1 and 2 due to an increase in disability group 3. 5. The proposed methodology of the hospital stage of cardiac rehabilitation improved exercise tolerance, hemodynamics and myocardial contractility, which immediately after aortocoronary bypass surgery were inferior to those in patients with conservative therapy of ischemic heart disease, indicating the greater severity of the condition after aortocoronary bypass surgery. 6. The proposed complex adequate adequate personalized cardiac rehabilitation program and "School of coronary patients" at the outpatient-polyclinic stage is highly effective, increases self-control of compliance with doctor's prescriptions and health improvement lifestyle. It is an effective secondary prevention of coronary heart disease, as it improves lipid spectrum, reduces total cholesterol, low-density lipoproteins and body mass index of patients, improves quality of life and increases socialization of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML