-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 2007-2011
doi:10.5923/j.ajmms.20231312.40
Received: Nov. 30, 2023; Accepted: Dec. 19, 2023; Published: Dec. 23, 2023

The Effect of Intrapleural Analgesia on the External Respiration Function of Patients after Surgical Interventions in the Hepatobiliary Zone
F. E. Sharapov1, A. L. Rosstalnaya1, 2, A. U. Tokhirov1
1Center for the Development of Professional Qualifications of Medical Workers, Tashkent, Uzbekistan
2Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to determine the effect of intrapleural analgesia on the function of external respiration of patients in the postoperative period. Introduction. Postoperative pain sensations represent only the visible part of the iceberg, being the root cause of a pathological postoperative syndrome development, which negatively affects the respiratory system. The main trend of clinical research in recent years in this area is the use of the principle of multimodality of pain protection with an emphasis on preventive (before injury and pain) protection. Material and methods. We observed 93 patients diagnosed with liver echinococosis and acute calculous cholecystitis, who were performed traditional liver echinococectomy and cholecystectomy from 2018 to 2022. The mean age of the examined patients was 52±3.4 years. The patients were divided into 2 groups depending on the type of anesthetic provision. In Group 1, the opioid analgesic promedol, 20 mg IM, was used for the treatment of postoperative pain; in group 2, patients for this purpose were administered intrapleural lidocaine 1% at a dose of 2.5 mg/kg upon request. Results. In Group 1, at the stages of surgery, there was an increase in the total peripheral vascular resistance by 15.1% (P<0.05) and a decrease in the indicators of one-time and one-minute heart performance. The main indicators of central hemodynamics of patients in Group 2 of patients at the stages of surgery were stable. Discussion. The use of intrapleural analgesia helps to normalize the patency of small bronchi and improves the patency of large and medium bronchi, creates prerequisites for the realization of muscular effort during breathing and coughing. Clinically, this was manifested by the disappearance of pain syndrome, relief of sputum discharge. Conclusion. Intrapleural analgesia using local anesthetics lidocaine 1% at a dose of 2.5 mg / kg is the most affordable and adequate method of postoperative anesthesia for surgical interventions in the hepatobiliary zone. Intrapleural administration of lidocaine improves the parameters of respiratory mechanics, which promotes the implementation of patients' active postoperative rehabilitation program.
Keywords: Analgesia, Intrapleural analgesia, External respiration, Liver echinococectomy, Cholecystectomy
Cite this paper: F. E. Sharapov, A. L. Rosstalnaya, A. U. Tokhirov, The Effect of Intrapleural Analgesia on the External Respiration Function of Patients after Surgical Interventions in the Hepatobiliary Zone, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 2007-2011. doi: 10.5923/j.ajmms.20231312.40.
1. Introduction
- Currently, there has been a significant increase in interest to the problem of postoperative pain and methods of combating it, due to the emergence of modern effective methods of analgesia and awareness of the role of adequate anesthesia in the postoperative rehabilitation of patients. Postoperative pain itself represents only the visible part of the iceberg, being the root cause of the development of pathological postoperative syndrome, which negatively affects the respiratory system [1-4]. The main trend of clinical research in recent years in this area is the use of the principle of multimodal pain protection with an emphasis on preventive (before injury and pain) protection [5-6]. Acute pain increases the rigidity of the chest muscles and anterior abdominal wall, which leads to a decrease in respiratory volume, vital lung capacity, functional residual capacity and alveolar ventilation. Collapse of the alveoli, hypoxemia and a decrease in blood oxygenation are the consequence of it. Difficulty in coughing due to pain interferes with the evacuation of bronchial secretions, promoting atelectasis with the subsequent development of pulmonary infection [7]. Increased oxygen consumption and carbon dioxide production leads to a corresponding increase in minute respiratory volume. Such an enhancement increases the work of breathing, especially at concomitant lung diseases. Bed rest and immobilization can also cause pulmonary dysfunction, regardless of the pain location. The opioid component remains as the basis of protection against pain at the central (segmental and suprasegmental) level. A preventive approach to the treatment of postoperative pain, based on pathogenetic complex prevention of pain impulses at all levels, is promising. The aim of the study was to determine the effect of intrapleural analgesia on the function of external respiration of patients in the postoperative period.
2. Material and Methods
- We observed 93 patients diagnosed with liver echinococcosis and acute calculous cholecystitis, who were performed traditional liver echinococectomy and cholecystectomy from 2018 to 2022. The mean age of the examined patients was 52±3.4 years. There were 17 males and 76 females. According to their physical status, the patients corresponded to ASA class II-III. All patients received standard premedication 40 minutes before the start of general anesthesia: atropine 0.01 mg/kg, diphenhydramine 0.2 mg/kg, promedol 20 mg were administered intramuscularly.The patients were divided into 2 groups depending on the type of anesthesia. Group 1 included 49 patients who were performed ataralgesia [8,9]. Group 2 included 44 patients in whom ataralgesia was supplemented by intrapleural analgesia (IPA), which transformed into postoperative IPA. Puncture of the pleural cavity was performed at the level of 6-7 intercostal space along the right middle axillary line in the position of the patient on his back. The skin was anesthetized in the usual way. The “Tuohy” needle was inserted to the upper edge of the underlying rib, then along its upper edge the needle was advanced further until resistance was felt, after identification the catheter was inserted 3 cm further from the tip of the needle upward, the needle was removed, the catheter was fixed on the skin with an adhesive plaster. A fixed catheter was used for postoperative pain relief.In Group 1, the opioid analgesic promedol, 20 mg IM, was used for the treatment of postoperative pain; in group 2, patients for this purpose were administered intrapleural lidocaine 1% at a dose of 2.5 mg/kg upon request. When deciding on the need for pain relief, we were guided by the international recommendations “Acute Pain Management: Scientific Evidence” (2005), focusing on the criteria for the maximum permissible pain intensity on a visual analogue scale (VAS) [10]. All patients were conducted standard clinical and laboratory tests: measurements were taken before the administration of the analgesic (baseline), and 5 and 15 minutes after its administration. The efficiency of analgesia was assessed by monitoring Mean Arterial Pressure (MAP), Heart Rate (HR), SaO2, Respiratory Rate (RR) with a Nihon Corden cardiac monitor (Japan); end-diastolic volume (EDV), end-systolic volume (ESV) were assessed by echocardiography; Stroke index (SI), cardiac index (CI), and total peripheral vascular resistance (TPVR) were determined using the generally accepted formula. Pain was assessed using a visual analog scale (VAS).The study of pulmonary functions was carried out in patients in the pre- and postoperative period using spirography. Pneumoscreen was done with Chesrgrapht – Hi–701. The study was carried out in a sitting position before and 24 hours after surgery. All parameters were automatically calculated as absolute values and as a percentage of the proper values. We studied the dynamics of the following parameters: vital capacity (VC), forced expiratory volume (FEV) in the first second, forced vital capacity (FVC), Tiffno test – FEV1/VC ratio (%); Parameters of the flow-maximum expiratory volume curve: peak expiratory volume flow rate, maximum volume flow rates (MVF) at 75, 50, 25% (VC) (MVF 75, MVF 50, MVF 25), aerodynamic resistance of the respiratory tract (Raw). Standards and gradations of deviations from the norm were specified according to data from N.N. Kanaev and R.F. Clement. The time of the patient's awakening, the time of tracheal extubation were determined.The received data were processed on a computer using the Microsoft Excel package. The average indicators were compared using standard methods of variational statistics of the biomedical profile.
3. Results
- The analysis of the obtained results of hemodynamic parameters study at various stages of anesthesiological support, depending on the technique used, revealed the following patterns: there was an increase in TPVR by 15.1% (P<0.05) and a decrease in the indicators of one-time and minute heart performance in Group 1 at the stages of surgery. Stroke volume (SV) decreased by 14.4% (P<0.05) compared to the initial stage, HR - by 14.7% (P<0.01), MAP was higher by 10.3% (P< 0.05) compared to the initial stage, which increased the myocardial oxygen demand. All this indicated the inadequacy of anesthetic protection in Group 1. The main indicators of central hemodynamics (CH) of patients in Group 2 of patients at the stages of surgery were stable. It was fundamentally important that at the stage of echinococectomy or isolation of the cystic duct, cholecystectomy, HR was lower by 22.2% (P<0.05), TPVR - by 20.3% (P<0.01), EDV was higher by 19.5% (P<0.05) compared with Group 1. Cardiac activity was transferred to a more economical mode of operation.With the same duration and the same type of surgical intervention, the time for recovery of consciousness and tracheal extubation from the moment of completion of surgical intervention in Group 1 was 43.3 ± 5.6 minutes (p < 0.01); in Group 2 it was 22.1 ± 5.2 minutes, which, accordingly, reduced the number of patients of this group requiring intensive monitoring in the ICU. Thus, more than 75% of patients in Group 2 were transferred to a specialized surgical department at the end of the operation, their postoperative period proceeded smoothly, and IPA was used for postoperative pain relief. The first need for analgesics in the early postoperative period in patients of Group 1 occurred after 65.3 ± 25.2 minutes, in Group 2 - 150.4 ±20.4 (P <0.05) minutes after the end of the surgery. After intramuscular administration of promedol, the analgesic effect began at the 10th minute and reached a maximum after 30 ± 10 minutes. Pain decreased by 55.1% according to VAS (averaging 3.6±1.3 points). 90 ± 15 minutes after administration of the drug, the pain occurred again (increased by 29.4% VAS). In addition, after the use of promedol, hypoventilation syndrome occurred in 2 (4.08%) of 49 patients. The data presented in Table 1 indicate that in the postoperative period, indicators of external respiratory function (ERF) were statistically significantly reduced from the proper standards.
|
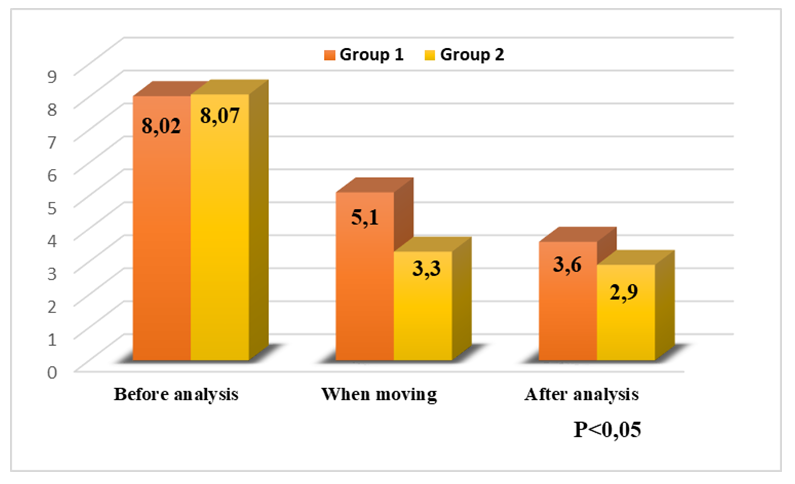 | Figure 1. Evaluation of postoperative pain relief efficiency (Visual Analogue Scale) |
4. Discussion
- The subjective assessment of the analgesic effect of the IPA is undoubtedly positive. In all cases, we managed to relieve pain syndrome on the first day of the postoperative period, without the use of opioid analgesics. Many patients had drowsiness or sleep. Intrapleural administration of local anesthetics causes unilateral sensory blockade of the chest and anterior abdominal wall. The block also applies to the muscles innervated by the pectoral nerves, including the external intercostal muscles - the muscles of inspiration and the internal intercostal muscles and abdominal muscles, which are also the muscles of inspiration. IPA was accompanied by an increase of VC by 4.9%, FVC - by 7.09% (P<0.05) and FEV - by 5.3%. The Tiffno index was decreased by 4.1% compared to the pre-analgesic stage, which was associated with the interruption of pain impulses from the surgical area. These data indicate a negative effect of pain syndrome on the tone of the small bronchi in the analyzed type of patients. The use of IPA helps to normalize the patency of small bronchi and improve the patency of large and medium bronchi, creates preconditions for the realization of muscular effort during breathing and coughing. Clinically, it was manifested by the disappearance of pain syndrome, relief of sputum discharge. All patients noted an improvement in their general condition. It became possible to take a deep breath and forced exhalation. A normal cough with active sputum discharge became possible. The data obtained suggest that external respiration in the postoperative period is significantly affected by surgical trauma, afferent impulses and postoperative pain syndrome. As a result of these changes, adynamia, impaired intestinal motility and cardiovascular insufficiency appear in operated patients. Since the pain of the operated patient inevitably increases with movement, it leads to his immobilization.IPA had a sufficient analgesic effect while fully preserving the function of the respiratory muscles, which, while maintaining the function of the intercostal muscles, ensures a full act of inspiration, keeping physiological breathing. Thus, in addition to adequate analgesia, an improvement in ventilation parameters and respiratory mechanics parameters was noted during IPA. As the block is selective, the effect on the motor activity of the respiratory muscles is minimal, and the contractility of the diaphragm is also not impaired. Analgesia is accompanied by an improvement in the component functions of the external respiration system, mechanical properties, and the musculoskeletal system—inspiratory and expiratory muscles. Since the patients we studied did not have a history of chronic pathology of the respiratory system, the results obtained allow us to confirm that postoperative pain syndrome disrupts the mechanical properties of the lungs and airway patency.
5. Conclusions
- Our studies confirmed the positive role of regional methods, the use of which begins before and continues during and after surgery. It dramatically reduces the intensity of pain and the need for analgesics of central action, allow to completely abandon the administration of drugs, or use them in moderate doses. Adequate postoperative analgesia is the main condition for the implementation of an active postoperative rehabilitation program. Combined IPA is an adequate and safe method of intraoperative protection of patients during surgical interventions in the hepatobiliary area. Intrapleural administration of lidocaine improves the parameters of respiratory mechanics, facilitating the implementation of an active postoperative rehabilitation program for patients. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML