-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 1975-1979
doi:10.5923/j.ajmms.20231312.33
Received: Nov. 20, 2023; Accepted: Dec. 13, 2023; Published: Dec. 20, 2023

Influence of Vitamin D Deficiency on the Course of Autoimmune Thyroiditis
D. A. Urunbayeva, D. K. Najmutdinova
Department of Internal Diseases No. 2 and Endocrinology, Tashkent Medical Academy, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article discusses the role of vitamin D in patients with autoimmune thyroiditis (AIT). The authors found that vitamin D levels were low in patients with AIT. In the article, the authors showed an inverse correlation between thyroid-stimulating hormone, antibodies to thyroperoxidase and thyroglobulin and vitamin D content, which indicates that vitamin D deficiency is also one of the pathogenetic links in the course of AIT.
Keywords: Vitamin D, Autoimmune thyroiditis, Hypothyroidism
Cite this paper: D. A. Urunbayeva, D. K. Najmutdinova, Influence of Vitamin D Deficiency on the Course of Autoimmune Thyroiditis, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 1975-1979. doi: 10.5923/j.ajmms.20231312.33.
1. Introduction
- Over the years, extensive research has highlighted the crucial role of vitamin D in the functioning of the immune system. Numerous studies have indicated that vitamin D plays a pivotal role in modulating immune responses and maintaining immune system homeostasis. The discovery of vitamin D receptors on immune cells has provided insights into its immunomodulatory functions. Understanding the intricate relationship between vitamin D and the immune system has paved the way for exploring its potential implications in various health conditions, including infectious diseases, autoimmune disorders, and inflammatory conditions. This comprehensive review aims to delve into the existing evidence elucidating the role of vitamin D in immune system reactions, providing a deeper understanding of its immunomodulatory mechanisms and its potential therapeutic implications.Autoimmune thyroiditis (another name is Hashimoto's thyroiditis) is a chronic autoimmune inflammatory disease of the thyroid gland with a hereditary predisposition, accompanied by its lymphocytic infiltration with subsequent replacement by fibrous tissue, which is a common cause of primary hypothyroidism [2,11,14,16].The prevalence of Hashimoto's thyroiditis is 800 cases per 100,000 people when assessed by review of published articles and 4600 cases per 100,000 when assessed by biochemical signs of hypothyroidism and thyroid autoantibodies [1,2,15].The etiological factors are stress and the environmental situation, leading to surges in adrenaline and cortisol, adrenal insufficiency, with a subsequent decrease in the adaptation syndrome, resulting in an increase in autoimmune diseases, including AIT; Endogenous factors – genetic predisposition; in order to realize a predisposition to the development of an autoimmune disease, additional external factors (viruses, various infections, and others) are required; Individuals who carry histocompatibility antigens HLA DR3 (atrophic form), DR5 (hypertrophic form) are predisposed to AIT [2,4,7].The disease is caused by a partial defect in immunological control - a deficiency of T-lymphocytes - suppressors, and therefore the survival of a prohibited phorbid clone of T-lymphocytes occurs. The interaction of the forbidden clone of T-lymphocytes with antigens triggers an immune process of the delayed-type hypersensitivity type, inflammatory mediators are released - lymphokines, tumor necrosis factor and other cytotoxic substances. Helper T lymphocytes act on B lymphocytes, which turn into plasma cells and form antibodies to thyroglobulin and the microsomal fraction (TPO). Antibodies on the surface of follicular epithelial cells, combining with killer T lymphocytes, have a cytotoxic effect, causing their destruction, reducing the secretion of T3, T4 and increasing TSH, which leads to an increase in the thyroid gland - goiter (hypertrophic form of AIT) [8,10,17].Autoimmune diseases are conditions in which an individual's immune system mistakenly attacks their own body. In these diseases, individual cells of the immune system play a major role, and there is an imbalance in the immune system's response. There are over 80 recognized autoimmune diseases, ranging from common conditions like rheumatoid arthritis and type 1 diabetes to more rare afflictions like systemic lupus erythematosus and multiple sclerosis. It is crucial to understand the role of individual immune cells in the development and progression of these diseases.The immune system is a complex network of specialized cells, tissues, and organs that work together to protect the body from harmful substances, such as viruses, bacteria, and cancer cells. The immune system is composed of several types of cells, including B cells, T cells, macrophages, and dendritic cells. These cells are constantly patrolling the body, seeking out and destroying foreign invaders.In autoimmune diseases, the immune system mistakenly targets and attacks normal, healthy cells and tissues. This can lead to inflammation, tissue damage, and a wide range of symptoms, depending on which cells and tissues are affected. The exact cause of autoimmune diseases is still unclear, but it is believed to involve a combination of genetic, environmental, and hormonal factors.One of the key elements in autoimmune diseases is an imbalance in the immune system’s response. Normally, the immune system is able to distinguish between self and non-self, meaning it can identify and destroy foreign invaders while leaving the body’s own cells and tissues unharmed. In autoimmune diseases, this balance is disrupted, leading to an overactive immune response against the body’s own cells and tissues.Individual cells of the immune system play a major role in this imbalance. B cells, for example, produce antibodies that target specific proteins on the surface of cells. In autoimmune diseases, B cells can mistakenly produce antibodies that attack the body’s own cells and tissues, leading to inflammation and tissue damage.T cells, another crucial component of the immune system, also play a major role in autoimmune diseases. T cells can directly attack and destroy cells that display abnormal or foreign proteins on their surface. In autoimmune diseases, T cells can become activated and target healthy cells and tissues, leading to the destruction of these tissues and the development of symptoms.Macrophages and dendritic cells are also involved in autoimmune diseases. These cells are responsible for presenting foreign substances to the immune system and initiating an immune response. In autoimmune diseases, macrophages and dendritic cells can become dysregulated, leading to an inappropriate immune response against the body’s own cells and tissues.The imbalance in the immune system’s response in autoimmune diseases can be influenced by various factors, including genetic predisposition, environmental triggers, and dysregulation of the immune system’s checkpoints and control mechanisms. For example, certain genetic variations have been linked to an increased risk of developing autoimmune diseases. Additionally, environmental factors such as infections, stress, and certain medications have been implicated in triggering or exacerbating autoimmune diseases.Recent research has also uncovered the role of epigenetic modifications in autoimmune diseases, which can influence the expression of genes involved in the immune response. This has led to a better understanding of the underlying mechanisms of autoimmune diseases and has opened up new avenues for the development of targeted therapies.Vitamin D is not only the main regulator of calcium-phosphorus metabolism, but also takes part in the control of various processes and functions in the body. The final active substrate, calcitriol, which is formed as a result of step-by-step synthesis from inactive precursors, is, by its mechanism of action and its characteristics, a true hormone D. Vitamin D is involved in calcium metabolism and mineralization of bone tissue [9,18,21]. In addition, vitamin D receptors are located on the surface of immune and cancer cells [11,15,17].First of all, the role of vitamin D is determined by its effect on the immune system. In this regard, special attention is now paid to the problem of vitamin D provision for patients with autoimmune diseases [10]. Vitamin D receptors have been found on almost all immunocompetent cells: CD4+ and CD8+, lymphocytes, antigen-presenting cells, including macrophages and dendritic cells [5,6,7,17,20]. Vitamin D receptor levels change as immune system cells mature. Naive T lymphocytes contain a small number of receptors, and mature forms are characterized by a high level of expression of the vitamin D receptor. In the process of differentiation of monocytes into macrophages and dendritic cells, the number of vitamin D receptors decreases [8,20]. This pattern reflects the sensitivity of immunocompetent cells to vitamin D, which may play a role in the fine regulation of the immune response. Macrophages, being carriers of vitamin D receptors, show greater sensitivity to vitamin D. Macrophages and dendritic cells themselves synthesize the active form of vitamin D, thanks to the expression of the enzyme a 1-hydroxylase, the activity of which, unlike renal localization, is regulated not by parathyroid hormone, but by cytokines [11,12,17,19].The purpose of the study was to study the relationship between vitamin D deficiency and immunological markers of the thyroid gland in patients with autoimmune thyroiditis.
2. Research Methods
- The study was conducted in the department of 2-therapy and endocrinology of the TMA multidisciplinary clinic. The study included 100 patients aged 18 to 45 years with autoimmune thyroiditis. Among them, 85 (85%) were women and 15 (15%) men, with an average age of 31.5±13.5 years. Laboratory tests were carried out: concentration of vitamin D - 25(OH)D in blood serum, levels of thyroid-stimulating hormone (TSH), free thyroxine (fT4), antibodies to thyropyroxidase (TPO-Ab), antibodies to thyroglobulin (TG-Ab), total calcium, as well as ultrasound data of the thyroid gland.A clinical examination and thyroid ultrasound were performed using a SonoScape SSI-6000 device (China) with a 7.5 MHz sensor at the initial visit, then annually. The obtained values of thyroid volume were assessed according to standards calculated relative to the body surface area. Goiter was diagnosed if the upper limit of normal values was exceeded. The levels of TSH, fT4, as well as the titers of TPO-Ab and TG-Ab in the blood serum were determined by ELISA using a set of reagents from the Alkor Bio company. Normal values were TSH 0.3-4.0 mUl/l, fT4 – 8,9-17,2 ng/ml, TPO-Ab – 0-30 IU/ml, TG-Ab– 0-100 IU/ml. The degree of vitamin D supply was assessed by the level of 25(OH)D in the blood serum (enzyme immunoassay method, Rayto analyzer, China) in 100 women using the criteria of the International Society of Endocrinologists (2011) [13] and the recommendations of the Russian Association of Endocrinologists [3,13]. A value of 25(OH)D in the blood serum above 75 nmol/l (above 30 ng/ml) was taken as a normal supply of vitamin D; a insufficiency was taken as 50 to 75 nmol/l (20-30 ng/ml); deficiency 50 nmol/l (below 20 ng/ml). The combination of an elevated TSH level with normal fT4 was regarded as subclinical hypothyroidism, and with a decreased level – as manifest hypothyroidism.Statistical processing of the results obtained was carried out using the “STATISTICA for Windows” system in accordance with the type of data and the size of the study groups. The criterion for statistical reliability of the obtained conclusions was considered to be the value p <0.05, generally accepted in medicine.
3. Results of Our Own Research
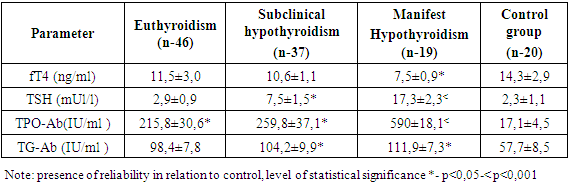
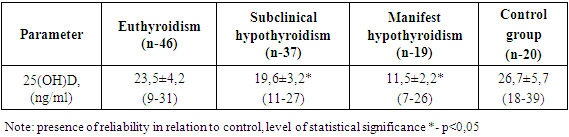
- An analysis of thyroid hormone levels revealed: euthyroidism in 46 (46.0%) patients, with the average TSH level being 2.9±0.9 mIU/ml; hypothyroidism in 56 (56.0%) patients. Among them, patients with subclinical hypothyroidism (SH) prevailed - 37 (66.0%) compared with manifest hypothyroidism (MH) - 19 (34.0%). According to a hormonal study with SH and MH, the blood TSH content was 7.5±1.5 mIU/ml and 17.3±2.3 mIU/ml (p<0.001), fT4 was 10.6±1, 1pg/ml and 7.5±0.9pg/ml, respectively. The control group consisted of 20 people who did not suffer from autoimmune thyroiditis and other thyroid pathologies, with an average age of 32.3±7.9 years. In patients with autoimmune thyroiditis, the average 25(OH)D content was 17.7±3.4 ng/ml (p<0.05) versus the control - 26.7±7.9 ng/ml.Among these patients, 54 (54.0%) had insufficiency, 26 (26.0%) had vitamin D deficiency, determined by the level of 25(OH)D in the blood serum. 20 (20.0%) patients had normal vitamin D levels. In the control group, it was revealed: vitamin D insufficiency in 12 subjects, normal levels of this vitamin in 8 subjects. At the same time, vitamin D deficiency was not detected in the control group. Calcium in the blood of patients ranged from 1.9 to 2.5 mmol/l, on average 2.2±0.5 mmol/l and there were no significant differences in the study group, but in patients with MH this figure was lower and amounted to 1.89±0.05 mmol/l in comparison with the SH and euthyroidism groups.
|
|
|
4. Conclusions
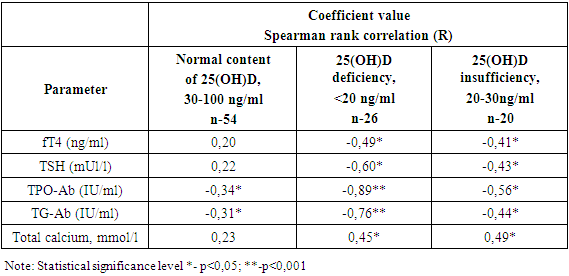
- In recent years, the importance of 25(OH)D in the treatment of autoimmune thyroiditis has been highlighted in many scientific works. 25(OH)D mainly plays an important role in calcium-phosphorus metabolism. In addition, the presence of vitamin D receptors in all organs and tissues of the human body indicates that this vitamin plays an important role in the human body. Vitamin D has receptors in human immune cells and acts as an immunomodulator. Vitamin D also plays a role in the treatment of autoimmune diseases of the thyroid gland. Several studies have shown a negative correlation between this vitamin and immune markers in patients with autoimmune thyroiditis.In this study, it was involved the patients with autoimmune thyroiditis who applied to the Multy-Specialty clinic of the Tashkent Medical Academy.In the examined patients, the amount of 25(OH)D in the deposit (17.7±3.4 ng/ml; r<0.05) was found to be lower than in the control (26.7±7.9 ng/ml). According to the results of the correlation analysis, in patients diagnosed with vitamin D deficiency, the amount of 25(OH)D in the deposit and TTG (-60), TPO-Ab (-0.89) (R<0.001), TG-Ab (-0.76) (R<0.001 ) was found to have a negative reciprocal feedback. The results once again proved that the amount of vitamin D in the blood is important in the disease process in these patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML