-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 1971-1974
doi:10.5923/j.ajmms.20231312.32
Received: Nov. 25, 2023; Accepted: Dec. 8, 2023; Published: Dec. 20, 2023

Pathomorphology of the Zona Glomerulosa of the Adrenal Glands in COVID-19
R. I. Israilov, N. N. Najmiddinova
Tashkent Medical Academy, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this article, pathomorphological changes of the cortical columnar area of the adrenal gland in COVID-19 infection are studied. The results showed that the interstitial tissue and blood vessels of the columnar region of the adrenal cortex during the COVID-19 infection exhibited severe discirculation, edema, haemorrhage and inflammatory infiltrates. It was found that in those patients who died from COVID-19, severe interstitial edema and destruction developed in the outer membrane and zona glomerulosa of the adrenal cortex, and in the columnar zone, the cytoplasm of parenchymal cells expanded and swollen due to vacuolar and fatty degeneration. It has been determined that necrobiosis, necrosis and infarction foci occur in the columnar region of the adrenal cortex due to various mechanisms, including discirculation, dystrophy, hypoxia and ischemia. Foci of necrosis and infarction undergo reparative regeneration over time and are morphologically infiltrated by macrophages, other histiocytic cells and lymphocytes.
Keywords: COVID-19, Adrenal glands, Zona glomerulosa, Columnar region, Fibrinoid necrosis, Thrombosis, Infarction
Cite this paper: R. I. Israilov, N. N. Najmiddinova, Pathomorphology of the Zona Glomerulosa of the Adrenal Glands in COVID-19, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 1971-1974. doi: 10.5923/j.ajmms.20231312.32.
1. Introduction
- The columnar zone of the adrenal cortex occupies two-thirds of the gland and consists of large adrenocorticocytes that form long columns. They predominantly synthesize glucocorticoid hormones, such as cortisol and cortisone, affect the immune system, slow down the growth of connective tissue, and reduce the rate of inflammatory and allergic processes. Today, more than 50 steroid compounds synthesized by the adrenal cortex have been identified. They are divided into two groups: glucocorticoids and mineralocorticoids, the first mainly affects the metabolism of carbohydrates, and the second controls the metabolism of minerals. Cortisol, cortisone and corticosterone from glucocorticoid hormones are synthesized in the columnar region of the adrenal cortex. In particular, hydrocortisone ensures the accumulation of glycogen in the liver and skeletal muscles, and also slows it down in other tissues. Aldosterone is responsible for water-salt metabolism and maintains the ratio of potassium and sodium salts to each other. Cortisol stimulates the immune system. If the body is exposed to unexpected stress, cortisol begins to be produced. As a result, brain function improves, heart muscles are strengthened, and the body can withstand any stress load.Cortisol is one of the glucocorticoids and is produced in the zona fasciculata of the adrenal cortex. It controls blood pressure, participates in protein, fat and carbohydrate metabolism, and protects the body from stressful situations. The synthesis and secretion of cortisol is controlled by adrenocorticotropic hormone (ACTH) through the opposite mechanism. ACTH is a hormone of the anterior pituitary gland, produced under the influence of tropic factors of the hypothalamus and having its own daily rhythmic cycle. Cushing's syndrome develops when the amount of cortisol in the blood increases. The development of this disease is observed with tumor diseases of the glands and the use of glucocorticosteroid hormones in large quantities. If the synthesis of glucocorticoids and mineralocorticoids by the gland is reduced, Addison's disease develops.It has been established that during infection with COVID-19, the blood vessels of the adrenal glands can be damaged, and then the parenchymal cells. Fibrinoid necrosis of the vascular wall in the gland tissue, the development of thrombosis and infarctions continue with irreversible damage to the adrenal parenchyma, the synthesis of hormones is disrupted, and metabolism in the internal organs is disrupted. Therefore, the problem of studying damage to the adrenal glands, including pathomorphological changes developing in the zona fasciculata of the cortex during COVID-19 disease, is relevant.
2. Material and Methods
- During the 2020-2021 pandemic, the adrenal glands were removed during autopsies of people who died from COVID-19 in 42 cases. Pieces of glands were frozen in a neutralized solution of 10% formaldehyde for 72 hours. They were washed in running water for 3-4 hours, dehydrated in alcohols of increasing concentrations, paraffin and wax were added and blocks were prepared. Histological sections 5-7 µm thick were prepared from paraffin blocks, deparaffinized and stained with hematoxylin and eosin. The state of connective tissue fibers in the tissue was studied with picrofuchsin using the Van Gieson method, and the accumulation of acid glycosaminoglycans was studied with Alcian blue staining.
3. Results
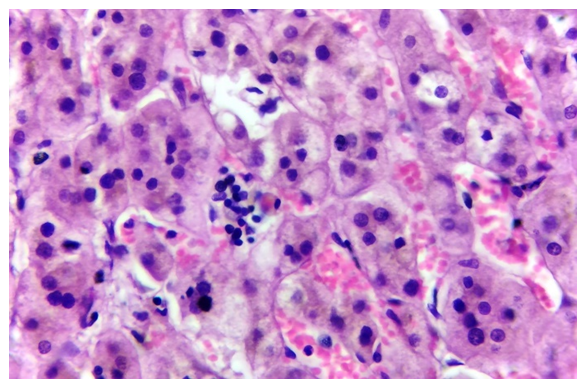
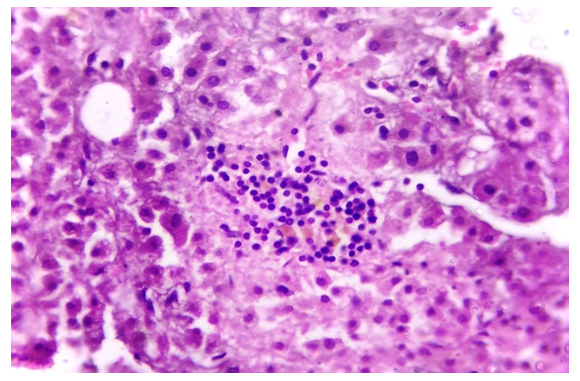
- The results of the study showed that the morphofunctional areas of the adrenal cortex of patients who died from COVID-19 underwent various morphological changes, including vasodilation, the development of plethora, and the development of perivascular hemorrhages in some areas. It has been established that the histotopographic area where the blood vessels are located, i.e. interstitial tissue is highly edematous and susceptible to hydration, especially in the subcapsular region, glomerular and fascicular zones, focal development of the edema process is noted. It was established that in some areas of the zona fasciculata the process of edema predominated, in others hemorrhages and necrotic processes took up a lot of space, and in others inflammatory lymphohistiocytic infiltration appeared. During COVID-19, under the influence of the SARS-CoV-2 virus, first the arteries and arterioles of the outer shell undergo fibrinoid edema, some of them undergo thrombosis, resulting in acute discirculation in the blood vessels that penetrate the parenchyma of the gland, as a result of damage to the intermediate tissue, acidic substances accumulate glycosaminoglycans, the tissue was hydrated and edematous. To determine the accumulation of acidic glycosaminoglycans, when staining a tissue section with Alcian blue, acidic interstitial tissue was stained dark blue, and this process was manifested by positive staining of the interstitial tissue of the outer membrane and the zona glomerulosa of the subcapsular region (Figure 1).
 | Figure 1. E, 37-year-old man who died of COVID-19, blue staining of the adrenal gland, outer connective tissue membrane, and interstitium of the glomerulosa region. Alcian blue(10x20) |
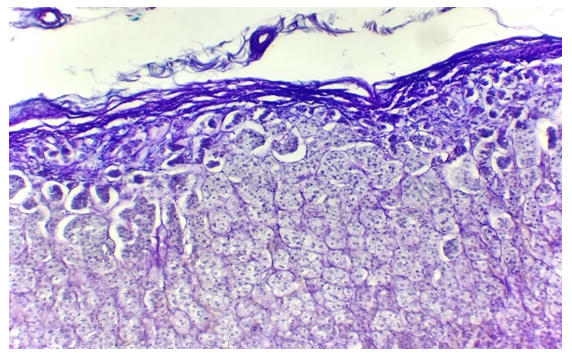
 | Figure 2. A, 51-year-old man who died of COVID-19, adrenal cortex, severe plethora, hemorrhage, edema of zona glomerulosa, severe vacuolar dystrophy of columnar cells. H-E(10x10) |
4. Discussion
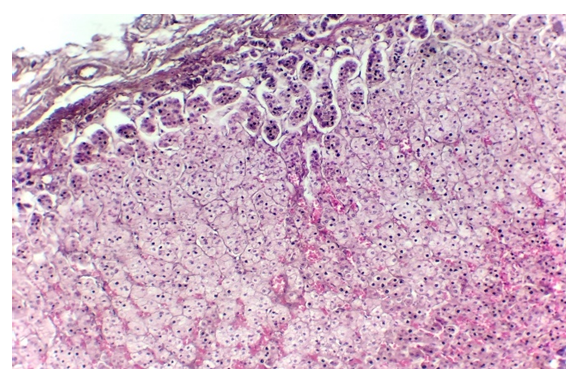
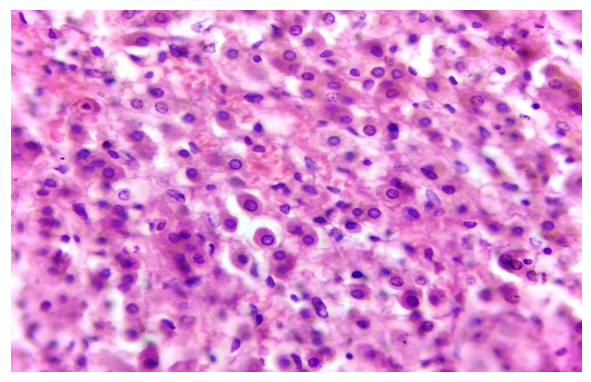
- It has been established that blood cells poured into the columnar region of the adrenal gland disintegrate, are absorbed by macrophages and other connective tissue cells and turn into hemoglobinogenic pigments, as a result of which histiocytic cells and connective tissue macrophages multiply in the interstitial tissue, and an infiltrate appears. It is observed that the parenchymal cells of the columnar region of the gland have lost their columnar arrangement and are located chaotically, most of the cells have undergone necrosis and necrobiosis, and foci of necrosis have appeared in the form of microinfarcts (Fig. 4). Among the parenchymal cells, the presence of regenerating and restoring cells was determined. These cells are relatively small in size, the cytoplasm is thin and eosinophilic, the nucleus is round and relatively large.
 | Figure 4. B, 55-year-old man who died of COVID-19, showed adrenal cortical, columnar area microinfarct foci and interstitial tissue proliferation. H-E(10x40) |
 | Figure 5. Z, 45-year-old woman who died of COVID-19, had an infarct in the columnar area of the adrenal cortex and lymphoid infiltrate. H-E(10x40) |
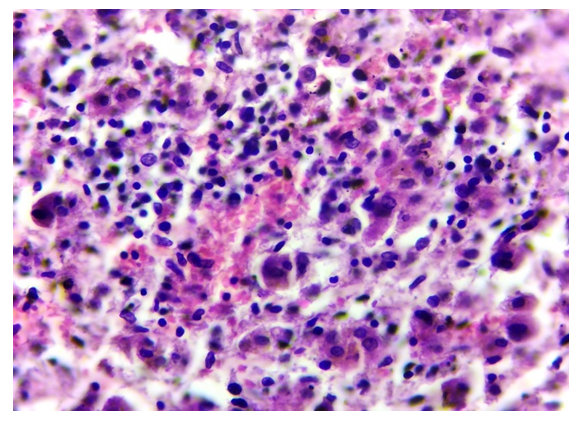 | Figure 6. Y, 61-year-old man who died of COVID-19, macrophages, histiocytic, and lymphoid cell infiltration in a focus of necrosis in the columnar area of the adrenal cortex, H-E(10x40) |
5. Conclusions
- When infected with COVID-19, severe discirculation, edema, hemorrhage and inflammatory infiltrate are observed in the interstitial tissue and blood vessels of the columnar region of the adrenal cortex.In those patients who died from COVID-19, severe interstitial edema and destruction developed in the outer membrane and capsular zones of the adrenal cortex, and in the columnar zone, the cytoplasm of parenchymal cells grew and swelled due to vacuolar and fatty degeneration.It has been established that necrobiosis, necrosis and infarction foci occur in the columnar region of the adrenal cortex due to various mechanisms, including discirculation, dystrophy, hypoxia and ischemia.Foci of necrosis and infarction undergo reparative regeneration over time and are morphologically infiltrated by macrophages, other histiocytic cells and lymphocytes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML