-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 1953-1958
doi:10.5923/j.ajmms.20231312.29
Received: Nov. 29, 2023; Accepted: Dec. 16, 2023; Published: Dec. 18, 2023

Role of Cytokines in the Regulation of Immune Response in Patients with Cutaneous Leischmaniasis
Ismailova G. A.1, Umurov F. F.2
1Doctor of Medical Sciences, Professor, Department of Dermatovenereology and Cosmetology, Tashkent Medical Academy, Uzbekistan
2Assistant, Bukhara Medical Institute, Uzbekistan
Correspondence to: Ismailova G. A., Doctor of Medical Sciences, Professor, Department of Dermatovenereology and Cosmetology, Tashkent Medical Academy, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

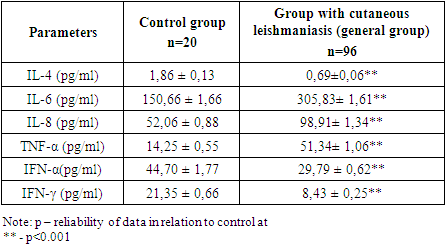
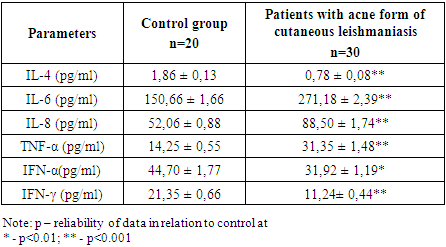
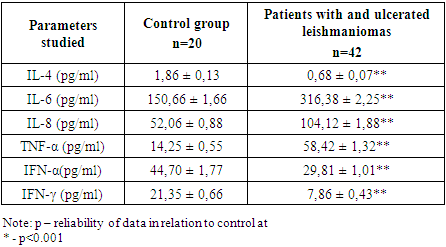
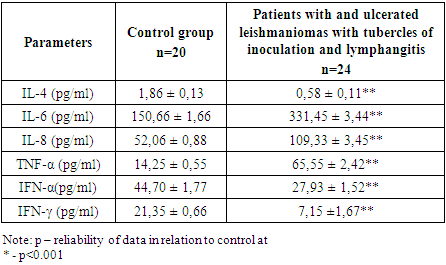
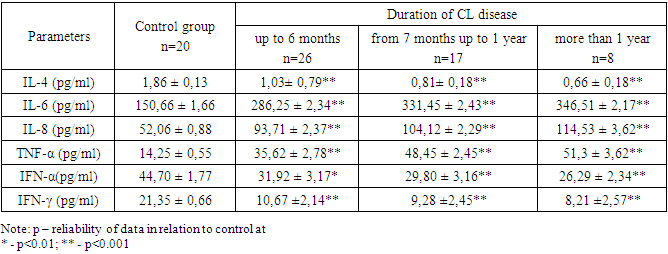
To study the role of some cytokines in the regulation of the immune response in patients with cutaneous leishmaniasis, taking into account the clinical form. Clinical; immunological (IL-4, IL-6, IL-8, TNF-α, IFN-α and IFN-γ), statistical research methods were used. Blood plasma from 96 patients with various clinical manifestations of cutaneous leishmaniasis were selected for the study. Of these, thirty patients were diagnosed acne form of cutaneous leishmaniasis, 42 – and ulcerated leishmaniomas, 24 – and ulcerated leishmaniomas with tubercles of inoculation and lymphangitis. The control group consisted of 20 practically healthy individuals aged 25 to 40 years. In patients with various clinical forms of cutaneous leishmaniasis, a significantly pronounced decrease in the synthesis of IL-4 and IFN-γ and high concentrations of proinflammatory cytokines, in particular TNF-α, are observed. In complicated forms of cutaneous leishmaniasis with lymphangitis and lymphadenitis, the levels of IL-6 and IL-8, as well as the synthesis of TNF-α, increased significantly relative to the control. A pronounced imbalance of cytokines was most typical in patients with a disease duration of more than 1 year. In cutaneous leishmaniasis, changes in the content of cytokines are detected, expressed by a deficiency in the concentration of the anti-inflammatory cytokine IL-4 and an increase in the content of proinflammatory cytokines IL-6, IL-8 and TNF-α, which are directly dependent on the clinical form and duration of the disease, which indicates active inflammatory process and the presence of immune deficiency, while anti-inflammatory and immune factors are insufficient for a favorable outcome of the disease. Invariation in the concentration of pro- and anti-inflammatory cytokines in various clinical forms of cutaneous leishmaniasis can be considered as a result of the immune response to the leishmania antigen, depending on the severity of the course, the development of complicated forms and the duration of the onset of the disease. The results obtained indicate the important regulatory role of cytokines in the manifestation of the immune response to leishmania and serve as a rationale for immunomodulatory, as well as rational and effective elimination antibiotic therapy.
Keywords: Cutaneous leishmaniasis, Clinical forms, Cytokine profile
Cite this paper: Ismailova G. A., Umurov F. F., Role of Cytokines in the Regulation of Immune Response in Patients with Cutaneous Leischmaniasis, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 1953-1958. doi: 10.5923/j.ajmms.20231312.29.
Article Outline
1. Introduction
- Cutaneous leishmaniasis (CL) (Leishmaniosi cutis), or Borovsky's disease (synonyms: cutaneous leishmaniasis of the Old World - Borovsky's disease; cutaneous leishmaniasis of the New World - American cutaneous leishmaniasis; visceral leishmaniasis - kala-azar) is a vector-borne, protozoal disease with endemic distribution in countries with a hot, tropical and subtropical climate [2,3,11,16]. Depending on the region of distribution, leishmaniasis causes damage to the skin, mucous membranes and internal organs. Cutaneous leishmaniasis affects the skin of exposed areas of the body, causing mainly the formation of ulcers, which can leave permanent scars, cause severe disability and lead to stigmatization of survivors. About 95% of cases of CL are observed in the countries of America, the Mediterranean basin, the Middle East and Central Asia. The annual number of new cases of this form of the disease is estimated to range from 600,000 to 1 million, but only about 200,000 cases are reported to WHO. In Central Asia, the main endemic zones are located in Uzbekistan and Turkmenistan [1,4,6,9]. In the endemic regions of Uzbekistan (Bukhara, Surkhandarya, Kashkadarya, Jizzakh, Karakalpakstan), there is a fairly high prevalence of zoonotic cutaneous leishmaniasis, where dozens of new cases of this disease are recorded annually [13,14].Currently, existing methods of combating CL, including extermination of pathogen reservoirs and vectors is labor-intensive and does not always give significant results. Due to the increase in incidence, registration of complications and atypical forms, insufficient preventive measures and pathogenetically based method streatment make the problem of CL extremely relevant [1,2,4,5,6,10,12,15,17,18,19].An important link in the pathogenesis of CL is the state of the immune reactivity of the patient’s body, the strength and degree of the immune response of which determines the prognosis and outcome of the disease.It is known that the cytokine network is the most important regulatory mechanism of intercellular interactions. An imbalance in cytokine production can affect both immunopathogenesis and the chronicity and progression of the disease. Recently, interest in the synthesis and secretion of cytokine molecules, their receptors, and natural antagonists has grown significantly and is of high importance due to the possibility of their use to determine etiopathogenesis, diagnosis, and monitoring the effectiveness of treatment [7,8].Pro- and anti-inflammatory cytokines, primarily mediators that influence the function of neutrophils and macrophages, play an important role in the regulation of antifungal, antiparasitic and anti-inflammatory resistance. An important role is played by IL-4, IL-6, IL-8 and TNF-α [8,16,18,20,21].Studying the levels of cytokines allows us to obtain information about the functional activity of various types of immunocompetent cells; about the severity of the inflammatory process, its transition to the systemic level and prognosis; on the relationship between activation processes Th1- and Th2-, which is very important in the differential diagnosis of a number of infectious and immunopathological processes; about the stage of development of a number of allergic and autoimmune diseases. In this regard, the study of the state of cytokines in patients with CL at the present stage seems extremely relevant.The purpose of the study: to study the role of some cytokines in the regulation of the immune response in patients with cutaneous leishmaniasis, taking into account the clinical form.
2. Materials and Methods of Research
- The work used clinical data (clinic and course of CL in the endemic region of Bukhara region, Republic of Uzbekistan); immunological (IL-4, IL-6, IL-8, TNF-α, IFN – α and IFN – γ), statistical research methods. Blood plasma from 96 patients with various clinical manifestations of CL were selected for the study. Of these, thirty patients were diagnosed acne form of cutaneous leishmaniasis, 42 – and ulcerated leishmaniomas, 24 – and ulcerated leishmaniomas with tubercles of contamination with lymphangitis. The control group consisted of 20 practically healthy individuals aged 25 to 40 years.
3. Results and Discussion
- We studied the content of anti- and pro-inflammatory cytokines in patients depending on the clinical forms of CL (IL-4, IL-6, IL-8, TNF-α, IFN-α and IFN-γ). These cytokines are important in the regulation cell-mediated immune response and play a decisive role in modulating the immune system, carrying out a complex of protective reactions of the body during the introduction of a pathogen. Thus, proinflammatory cytokines typically regulate the growth, activation and differentiation of immune cells, as well as the targeting of immune cells to sites of infection to control and destroy pathogens, initiating an inflammatory response. Anti-inflammatory cytokines regulate immune responses and limit the development of inflammation in many pathological conditions and infections [7,8].As the results of the study showed (Table 1), the initial data on the level of pro-inflammatory cytokines were significantly increased. Thus, the level of IL-6 was 2 times higher than the values in the control group, averaging 305.83± 1.61pg/ml (p<0.001). The level of IL-8 was 1.9 times higher than the control values. Noteworthy are the high levels of TNF-α, which was 3.6 times higher than the control values. On the contrary, the content of the anti-inflammatory cytokine IL-4 in patients in this group was 2.7 times lower than in the control, amounting to0.69±0.06pg/ml (p<0.001). Similar changes were characteristic of IFN-α and IFN-γ. In this case, IFN-γ deficiency was more pronounced compared to the control (2.53 times), and amounted to8.43 ± 0.25pg/ml (p<0.001).
|
|
|
|
|
4. Discussion
- Thus, analysis of the data obtained shows that in cutaneous leishmaniasis, changes in the content of cytokines are detected, expressed by a deficiency in the blood plasma concentration of the anti-inflammatory cytokine IL-4 and an increase in the content of proinflammatory cytokines IL-6, IL-8 and TNF-α, which are directly related on the clinical form and duration of the disease.Analyzing the results obtained, the following should be noted. Cytokines, key modulators of inflammation, are produced in response to invading pathogens by stimulating, recruiting, and proliferating immune cells. Proinflammatory cytokines are secreted by CD4+ T cells, macrophages and dendritic cells and are characterized by the production of several interleukins, in particular the one we studied TNF-α, IL-6, IL-8, IFN-γ and IFN-α (last the cytokine is involved in both pro- and anti-inflammatory processes). These cytokines regulate the growth, activation and differentiation of immune cells, as well as the direction of immune cells to foci of infection in order to control and destroy the pathogen. In our studies, elevated levels of cytokines, in particular TNF-α indicates the development of a powerful inflammatory response in the body in response to the introduction of Leishmania. In our opinion a high level of these cytokines is a reflection of the activity and severity of the pathological process. Moreover, in our case, with complicated clinical forms of CL, the levels of these cytokines were significantly high (Pic 1).
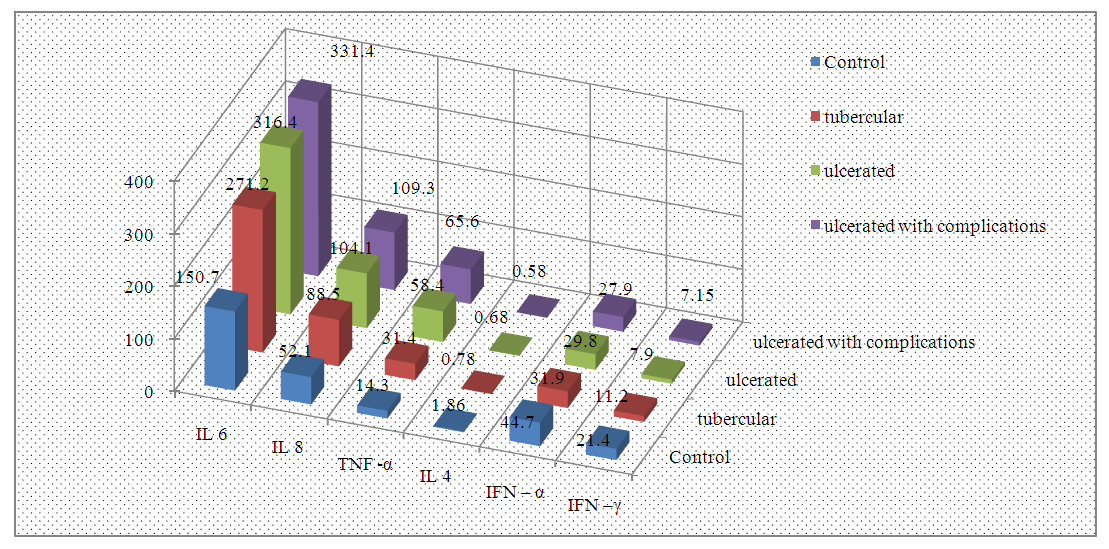 | Picture 1. Blood cytokine levels in patients with various clinical forms of cutaneous leishmaniasis |
5. Conclusions
- 1. The variation in the concentration of pro- and anti-inflammatory cytokines in different clinical forms of CL is quite understandable and can be considered as a result of the course of the inflammatory process caused by Leishmania, depending on the severity of the course, the development of complicated forms and the duration of the onset of the disease.2. Our data indicate the important regulatory role of cytokines in the manifestation of the immune response to leishmania and serve as a rationale for immunomodulatory therapy, as well as rational and effective eliminating antibiotic therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML