D. A. Alimov, S. B. Tursunov, Sh. R. Mubarakov, B. Sh. Alimkhanov
Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The aim of the research was to study the efficiency of the thrombus extraction method in patients with ischemic stroke during the therapeutic window”. Introduction. Currently, stroke is the second most common cause of death in the world, only slightly behind coronary heart disease. Ischemic stroke makes up at least 75-80% of all cases of stroke. To date, thrombolytic therapy in patients with ischemic stroke during the therapeutic window is the standard method of treatment, ensuring the achievement of recanalization of the occluded vessel. However, the efficiency of this method is only 20%. Material and methods. 43 patients with acute cerebrovascular accident who were admitted to the Department of emergency Neurology and therapeutic ICU of the Republican Research Center of Emergency Medicine during the therapeutic window from 2015 to 2022 were examined. The mean age of the patients was 65.2±7.8 years. The largest number of patients were in the age range of 41-60 years (20.9%), as well as at the age of 61-80 years (79.1%). Results. As a result of thrombus extraction, recanalization was not achieved in 5 (11.6%) of 43 patients (TICI 0 points) and in 3 (7.0%) patients the degree of recanalization and reperfusion was minimal (TICI grade I). In 35 (81.4%) patients, recanalization was achieved through thrombus extraction. In 10 (23.2%) patients, the degree of reperfusion was TICI IIa, in 15 (35%) – TICI IIb, in 10 (23.2%) patients complete recanalization was achieved -TICI III. Discussion. The morphological basis of the patient’s clinical outcome is the recanalization of the target stroke-related artery, as a result of which blood circulation is restored in the penumbra zone, and, as a consequence, neuronal function is restored. Clinically, this manifests itself as regression of focal neurological deficits. Conclusion. Thrombus extraction is a pathogenically substantiated method of treating patients in the acute period of ischemic stroke. Carrying out thrombus extraction outside the 6-hour “therapeutic window” reduces the clinical efficiency of this method.
Keywords:
Thrombus extraction, Stroke, Recanalization, Reperfusion
Cite this paper: D. A. Alimov, S. B. Tursunov, Sh. R. Mubarakov, B. Sh. Alimkhanov, Urgent Endovascular Interventions in the Acute Period of Ischemic Stroke, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 1879-1886. doi: 10.5923/j.ajmms.20231312.13.
1. Introduction
Currently, stroke is the second most common cause of death in the world, only slightly behind coronary heart disease. In addition, stroke is one of the main causes of disability of the population [1-2]. It should be noted that ischemic stroke makes up at least 75-80% of all cases of stroke [3]. In 80% of cases, the cause of cerebral infarction is acute thrombotic occlusion of the intracranial artery, which makes recanalization of the infarct-related artery and reperfusion of the affected area of brain tissue the basis of pathogenetic treatment [4-6]. Achieving recanalization and reperfusion of the brain as early as possible from the onset of the disease significantly reduces the infarct area due to the survival of neurons in the penumbra (“ischemic penumbra”) and, as a result, improves clinical outcomes [7]. Today, thrombolytic therapy in patients with ischemic stroke during the “therapeutic window” is a standard treatment method, ensuring the achievement of the occluded vessel recanalization. However, the efficiency of this method is only 20% when successful reperfusion of the ischemic area of the brain is achieved [8]. One of the reasons for the low efficiency of thrombolytic therapy are thrombi with stabilized fibrin in large-diameter vessels (proximal sections of the internal carotid artery and large intracranial arteries), which do cardioembolic not respond well to the effects of tissue plasminogen activator, which occurs in cardioembolic subtype of ischemic stroke [9]. The results of 5 randomized trials involving 1,287 patients showed that the combination of thromboextraction with thrombolytic therapy improved ischemic stroke treatment results in the carotid basin and does not increase the risk of hemorrhagic transformation of the ischemic focus [10-14]. In 2018, the American Heart Association and the American Stroke Association, based on the results of evidence-based medicine, published updated recommendations for the management of patients with ischemic stroke in the acute period, in which the thrombus extraction method was assigned the I class of evidence (level A) [15]. In patients with ischemic stroke in the vertebrobasillary basin, mortality can reach 85-95% in the absence of recanalization of the occluded vessel [16]. The use of the thrombus extraction method for acute occlusion of a. Basilaris within the first 6 - 8 hours allows to achieve recanalization and reduce the mortality rate to 10-15% [17].There are several methods with appropriate devices to perform mechanical thrombextraction. All devices for mechanical thrombus extraction are delivered via endovascular access proximal to the site of occlusion. The devices can be divided into 3 main groups depending on where they will affect the thrombus:• Proximal devices apply force to the proximal base of the thrombus - this group includes various aspiration catheters and systems. • Distal devices approach the thrombus proximally, but then move with the help of a microcatheter through to be positioned behind it, where force is applied to the distal base of the thrombus - this group includes devices in the form of "brushes", "baskets" or "spirals".• The most recently developed devices operating on the principle of a stent: the device is placed on the proximal side of the occlusion, inserted into the thrombus and deployed inside it, after which the stent with the thrombus is removed from the vessel. This group includes various self-expanding stent devices for retrieving blood clots (stent retrievers).Thus, mechanical endovascular recanalization - thrombus extraction - is a pathogenetically substantiated principle in the treatment of acute ischemic stroke. This method is a controlled and managed type of intervention. Reperfusion of the occluded vessel can be achieved by endovascular treatment in 90% of cases [18].The aim of the research was to study the efficiency of the thrombus extraction method in patients with ischemic stroke during the "therapeutic window”.
2. Material and Methods
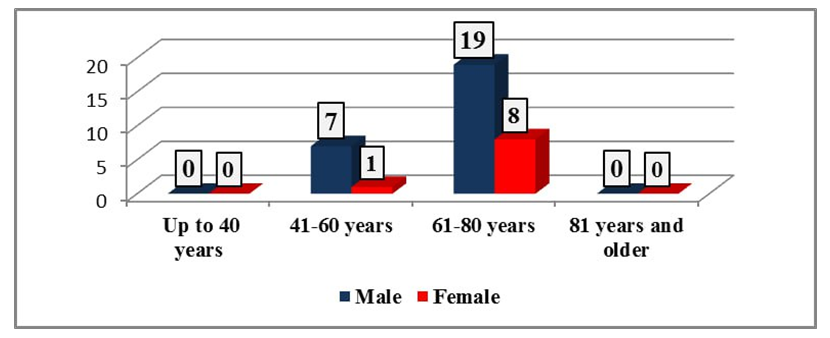
43 patients with acute cerebrovascular accident who were admitted to the Department of emergency Neurology and therapeutic ICU of the Republican Research Center of Emergency Medicine during the "therapeutic window" from 2015 to 2022 were examined. The mean age of the patients was 65.2±7.8 years. In terms of age, patients were divided into the following age groups: Group 1 - up to 40 years – 0 (0%); Group 2 - 41-60 years old – 9 (20.9%; Group 3 - 61-80 years old – 34 (79.1%); Group 4 - 81 years old and older – 0 (0%) (Fig. 1).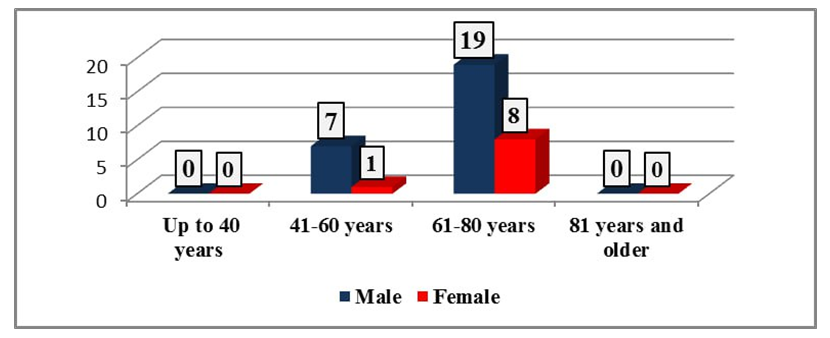 | Figure 1. Distribution of patients by age and gender |
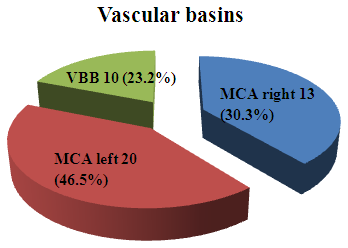
The largest number of patients were in the age range of 41-60 years (20.9%), as well as at the age of 61-80 years (79.1%). There were no patients under the age of 40 and over 81 years old. Males prevailed in all age groups.According to the localization of vascular basins lesion, the following was revealed: in the middle cerebral artery (MCA) basin of the right hemisphere, acute cerebrovascular accident (ACVA) developed in 13 (30.3%) patients, MCA basin from the left – in 20 (46.5%) cases and in the vertebrobasilar basin (VBB) – in 10 (23.2%) patients (Fig. 2).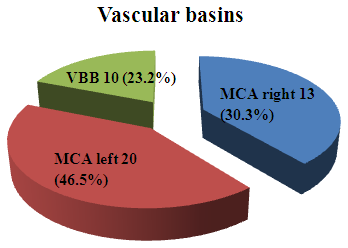 | Figure 2. Patients’ distribution according to vascular basins lesion |
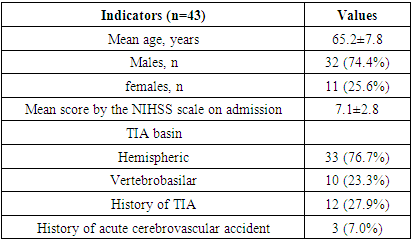
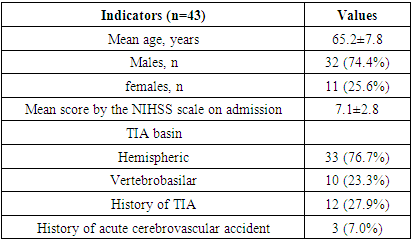
The level of consciousness in all patients was clear and corresponded to 15 points on the Glasgow scale. The severity of neurological deficit on the NIHSS scale averaged 7.1±2.8 points.Inclusion criteria of patients for thrombus extraction were as follows [15]:• Patients with acute ischemic stroke during the 4.5 hour “therapeutic window”;• Presence of occlusion of the internal carotid artery (ICA) or M1-M2 segments of MCA verified by MSCT angiography;• Neurological deficit of 6 or more points by the NIHSS scale. Exclusion criteria for patients undergoing thrombus extraction:• Occlusion of the ICA up to the entrance to the cranial cavity; • Vascular diseases for which the use of endovascular instruments is impossible;• Severe atheromatosis of the aortic arch;• Pronounced looping and tortuosity of vessels;• Intracranial hemorrhage for up to 1 month;• Age over 75 years due to the high risk of developing perioperative complications;• Patients with signs of severe heart failure and cardiac arrhythmias. The patients were admitted to the clinic during the therapeutic “window”, within 4.5 hours from the development of the first symptoms of acute cerebrovascular accident. The patients were performed MSCT examination of the brain, on the basis of which intracerebral hemorrhage was excluded. MSCT angiography of extra- and intracranial arteries was performed to verify occlusion of the cervical part of the internal carotid artery or its intracranial branches. Patients were examined by a neurologist; neurological status was estimated using the NIHSS scale. The clinical picture of ischemic stroke in 33 (76.7%) patients was represented by hemispheric symptoms, and in 10 (23.3%) cases – by vertebrobasilar ones. It should be noted an important fact that 12 (27.9%) patients had a history of transient ischemic attack (TIA), and 3 (7.0%) patients had previously suffered from ischemic stroke with subsequent recovery of neurological deficit (Tab. 1). Table 1. The main clinical indicators of patients
 |
| |
|
Endovascular intervention was a traditional cerebral angiography, which was performed under local anesthesia by puncturing a. femoralis communis using the Seldinger method. Catheterization was carried out followed by contrasting of the proximal parts of the internal carotid and vertebral arteries to verify occlusive-stenotic processes. The thrombus extraction technique was carried out as follows:After treatment of the surgical field and anesthesia in the area of the femoral triangle with 1% lidocaine solution 10 ml, a puncture of the right common femoral artery was performed. A 6F/110 mm introducer was installed into the artery. Using a diagnostic catheter JR 6F-100cm and a hydrophilic guide 035-300 Raptor, catheterization of the right common carotid artery was performed. The 7Fr guide-introducer was installed in the proximal part of the right ICA using a hydrophilic guide 035-260. A TrevoProVue microcatheter on a 014-Runthrough guidewire was advanced into the occlusion zone with distal exit into the M3 segment of the MCA. Next, the Solitaire 4x20 stent retriever was installed into the thrombus in the occlusion zone. Removal of the retriever-microcatheter complex was conducted under continuous aspiration using a 50 ml Luer-Lock syringe.
3. Results
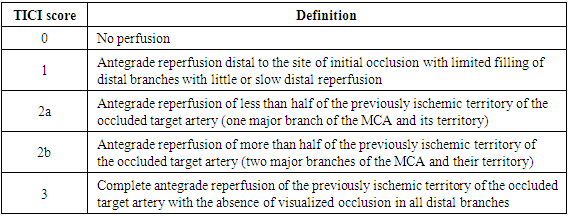
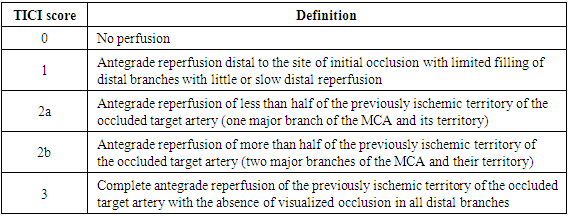
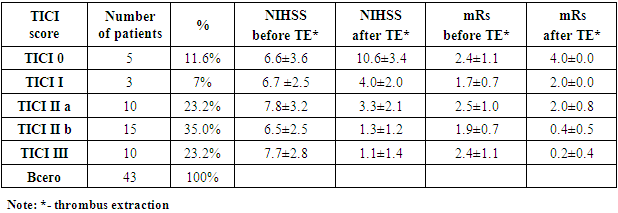
To perform endovascular interventions in patients with acute ischemic stroke, the first stage consisted of MSCT angiography of the main and intracranial arteries of the brain. It aloowed to clarify the causes of ischemic stroke and stroke-dependent artery. Traditional cerebral angiography followed by thrombextraction was performed after accurate determination of the vascular basin and stroke-dependent artery and obtaining the consent of relatives for endovascular interventions. Evaluation of this procedure efficiency was estimated by the Thrombolysis In Cerebral Infarction (TICI) angiographic scale. The clinical efficiency of thrombus extraction was assessed using the NIHSS scale, which characterizes the severity of neurological deficit, as well as the Rankin scale (mRs - modified Rankin scale). The final indicators of endovascular interventions efficacy during the 90-day observation period considered such events as TIA, recurrent ischemic stroke, patient death from recurrent stroke (Tab. 2).Table 2. TICI scale
 |
| |
|
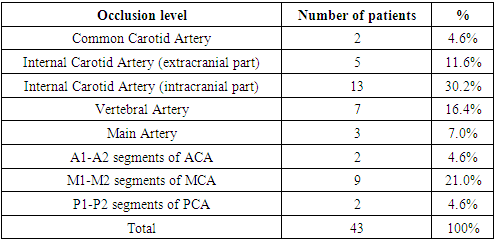
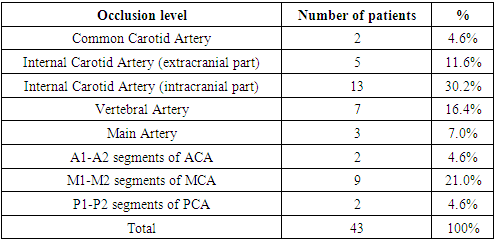
The thrombus extraction technique was performed in patients during the therapeutic “window” of ischemic stroke with blockage of the extracranial and intracranial parts of the internal carotid artery, as well as with blockage of the M1-M2 segments of the middle cerebral artery, A1-A2 segments of the anterior cerebral artery, with blockage of the basilar artery, vertebral arteries and P1-P2 segments of the posterior cerebral artery. The thrombus extraction in smaller segments of the arteries of the anterior cerebral artery (ACA), middle cerebral artery (MCA) and posterior cerebral artery (PCA) is not technically possible. As a result of thrombus extraction, recanalization was not achieved in 5 (11.6%) from 43 patients (TICI score 0) and in 3 (7.0%) patients the degree of recanalization and reperfusion was minimal (TICI I) (Tab. 3). Table 3. The level of the stroke-related artery occlusion
 |
| |
|
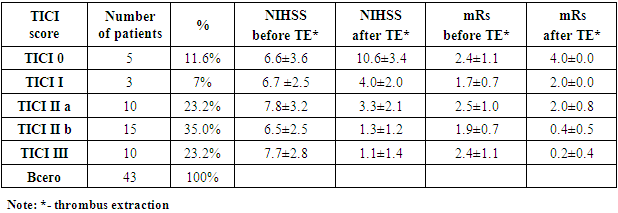
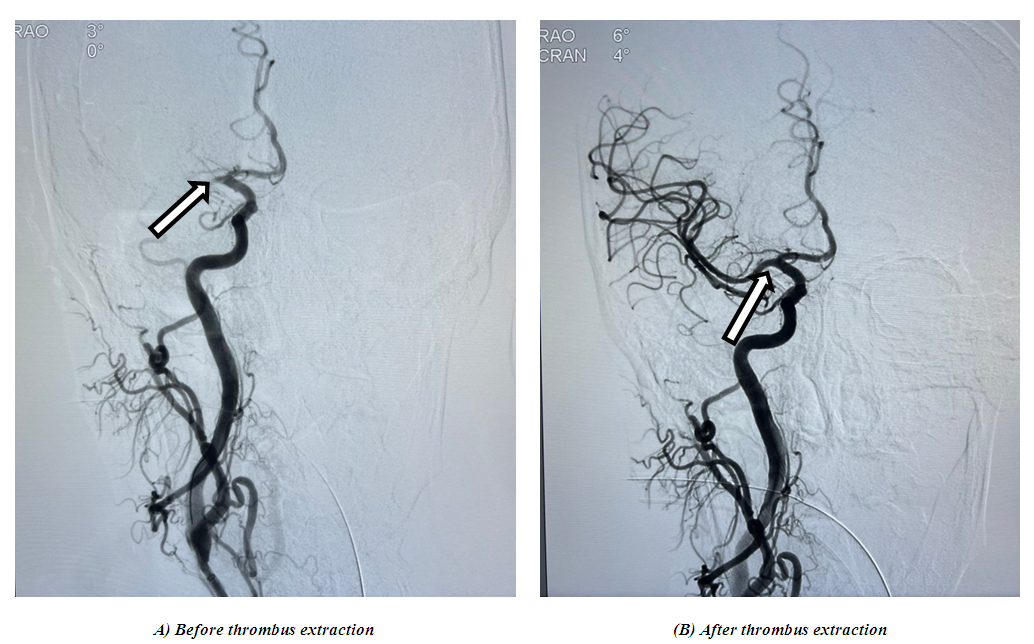
A possible reason was that in all 8 patients the time from the development of the first symptoms of ischemic stroke to thrombus extraction exceeded a 6-hour interval (the mean time was 7.3±1.2 hours). It should be also noted that there was occlusion of the M1 – M2 segments of the MCA. It should be clarified that thrombus extraction becomes technically more complicated as the diameter of the intracranial artery narrows. Clinical evaluation of the efficiency was carried out based on the results of the NIHSS scale before and after thrombus extraction. In patients with no recanalization according to angiography (TICI 0), no clinical effect in the form of neurological deficit regression was observed: in 5 patients upon admission, the average NIHSS score was 6.6±3.6 points. 24 hours after thrombus extraction this indicator made up 10.6±3.4 points. There was an increase in neurological deficit in these patients during the next 24 hours due to the lack of blood flow restoration.At the TICI I degree of recanalization, the average score in 3 patients upon admission was 6.7±2.5, after thrombus extraction - 4.0±2.0 points. In 10 patients with recanalization degree TICI IIa, the neurological deficit by the NIHSS scale was 7.8±3.2 points. After thrombus extraction, there was a significant regression of the deficiency to 3.3±2.1 points. In 15 patients with a recanalization degree TICI IIb at the time of admission, focal neurological symptoms were expressed as 6.5 ± 2.5 points by the NIHSS scale. Endovascular thrombus extraction promoted a significant regression of neurological deficit – 1.3±1.2 points by the NIHSS scale. 10 patients had complete restoration of blood flow in the occluded target artery (TICI III) according to cerebral angiography data. At the same time, the neurological deficit improved from 7.7±2.8 points to 1.1±1.4 points by the NIHSS scale (Tab. 4, Fig. 3 and Fig. 4). Table 4. Recanalization degree after thrombus extraction according to the TICI scale
 |
| |
|
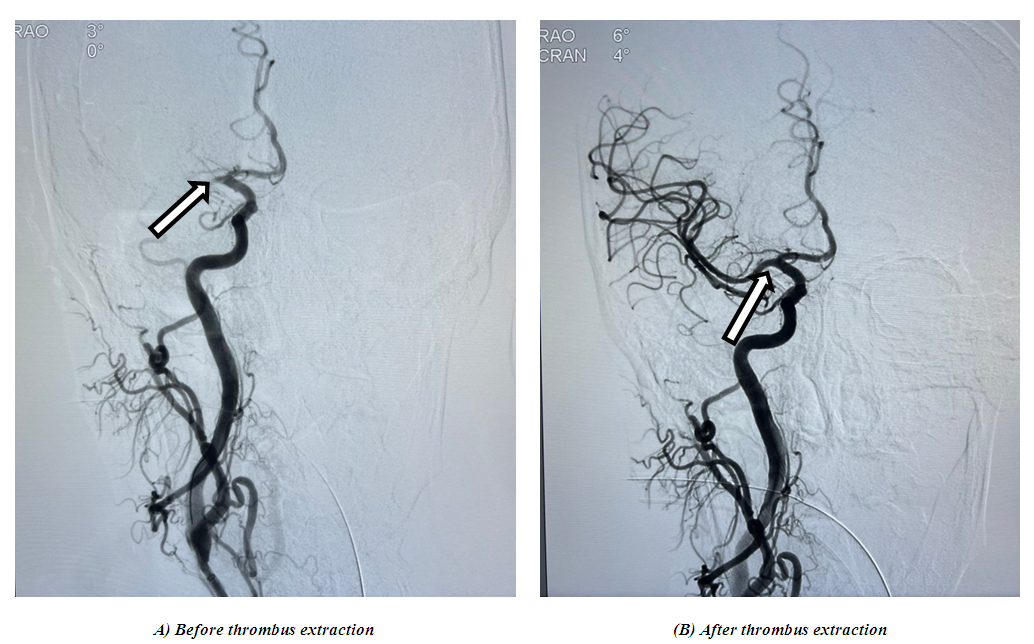 | Figure 3. Patient B., 70 years. Cerebral angiography (A) before thrombus extraction - occlusion of the M1 segment of the right ICA, (B) after thrombus extraction complete recanalization of the M1 segment of the right ICA (TICI III) |
 | Figure 4. General view of a thrombus after thrombus extraction |
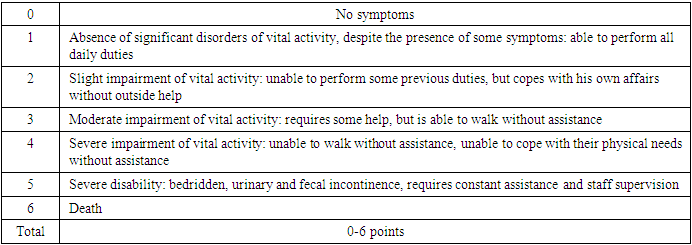
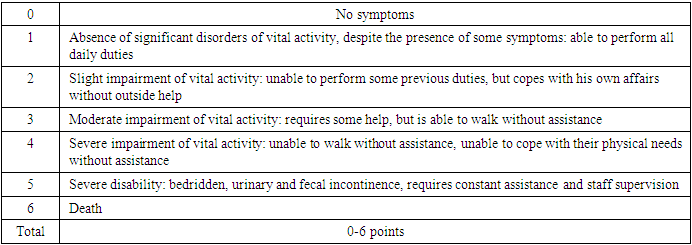
According to Table 4, it can be seen that in 35 (81.4%) patients it was possible to achieve recanalization by thrombus extraction. Thus, in 10 (23.2%) patients, the degree of reperfusion was TICI IIa, in 15 (35%) – TICI IIb, in 10 (23,2%) patients complete recanalization was achieved – TICI III. In patients with a degree of recanalization TICI 0 and TICI I, there was an increase in the degree of disability due to persistent occlusion or minimally expressed recanalization, insufficient to restore the functional activity of neurons in the penumbra zone. Thus, at TICI 0, the average score on the Rankin scale increased from 2.4 ±1.1 to 4.0 ±0.0 points. There was also an increase in the degree of disability from 1.7 ±0.7 to 2.0±0.0 points by the mRs scale in patients with the TICI I recanalization degree. However, in patients with recanalization levels of TICI IIa, TICI IIb and TICI III, as a result of adequate recanalization and reperfusion, there was a decrease in the degree of disability. Thus, in patients with TICI IIa, there was a decrease from 2.5±1.0 to 2.0±0.8 points on the mRs scale, with TICI IIb – from 1.9± 0.7 to 0.4± 0.5 points; with TICI III – from 2.4±1.1 to 0.0 ± 0.4 points.One of the clinical methods for evaluating the recovery of neurological deficits is an assessment by the modified Rankin scale (mRs), which characterizes the degree of the patient's disability as a result of a stroke (Tab. 5).Table 5. The modified Rankin scale (mRs)
 |
| |
|
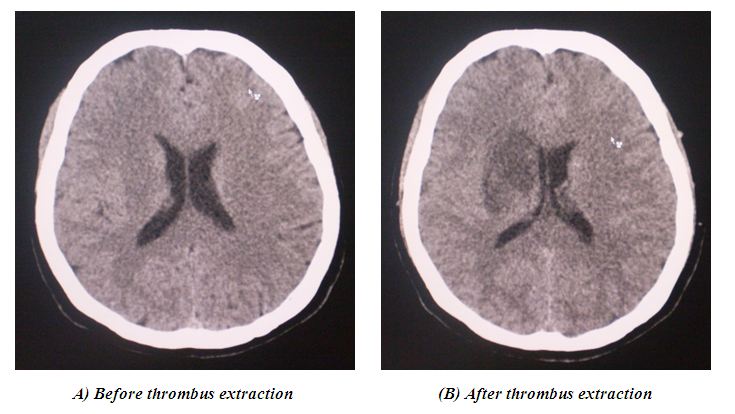
Besides the angiographic and clinical picture in patients with acute ischemic stroke, the MSCT picture of the brain is of great interest. Considering that all patients were admitted to the clinic during the "therapeutic window", according to the results of the MSCT study, no areas of ischemic brain damage were detected. However, an MSCT examination of the brain 24 hours after thrombectomy may show significant changes in the structures of the brain from signs of an ischemic zone to areas of hemorrhage. The absence of recanalization promotes further ischemic damage to the brain substance, which is visually manifested on MSCT in the form of a hypodensic zone, the size of which will be directly proportional to the diameter of the occluded vessel. Also, in practice, a situation may develop when, due to the restoration of blood flow and the achievement of recanalization, hyperperfusion of the brain substance is developed in the occluded vessel, the so-called “luxurious perfusion” syndrome, as a result of which perdiapedetic infiltration of blood into the brain parenchyma may be developed. The MSCT picture in all 5 (11.6%) patients with no recanalization (TICI 0) was characterized by the development of an ischemic stroke zone, the largest size was 4.6x3.2 cm (Fig. 5). 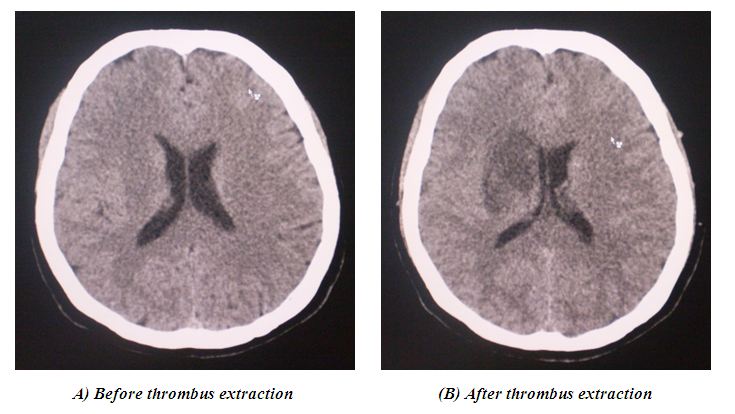 | Figure 5. Patient A, 50 years. (A). Before thrombus extraction, no signs of stroke were detected at the time of the study. (B). After thrombus extraction, a hypodensity zone measuring 4.6 x 3.2 cm is determined in the parietal-temporal region of the right hemisphere with a density of + 26 units. N |
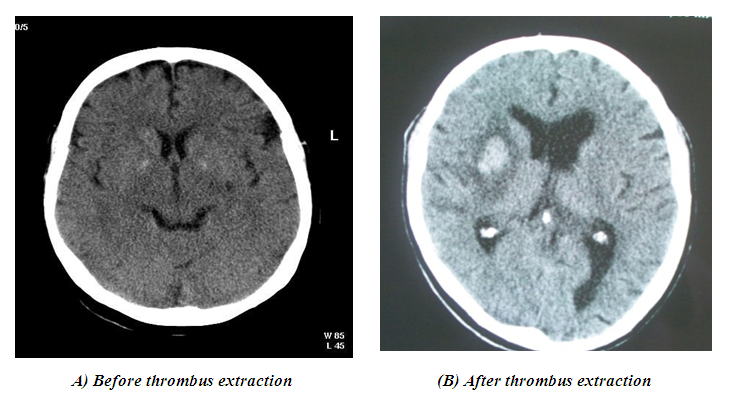
In 5 (11.6%) patients with TICI IIa and in 3 (7%) cases with TICI IIb ischemic stroke was developed, the maximum size of which was 53x32x21 mm. In 3 (7%) patients with complete recanalization of the target artery on MSCT examination of the brain, hemorrhage of the type of perdiapedesis impregnation was developed 24 hours after thrombus extraction. At the same time, a complete regression of focal neurological deficit was clinically observed in all 3 patients (Fig. 6). 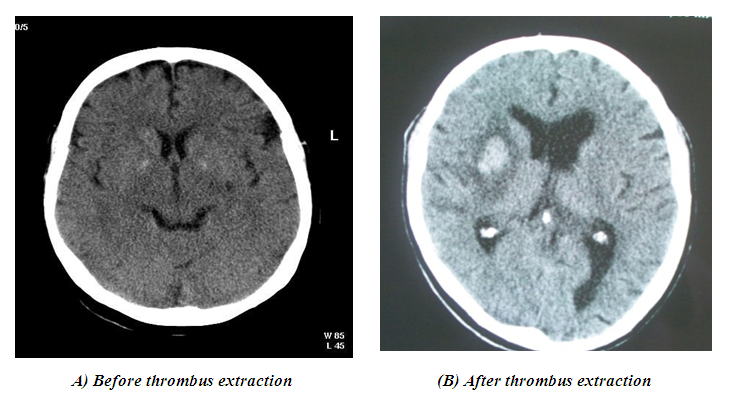 | Figure 6. Patient C. 75 years. (А). CT upon admission revealed no signs of stroke. (B). After thrombus extraction, a hyperdense zone measuring 4.3 x 2.2 cm was determined, with a density of + 46 units of N, with a total volume of 5 cm3 |
Thus, asymptomatic perdiapedic soaking after thrombus extraction can be considered as a marker of adequate recanalization and reperfusion of the brain after thrombus extraction.
4. Discussion
As a result of the work, various clinical and angiographic results were obtained after performing thrombus extraction. The morphological basis of the patient’s clinical outcome is the recanalization of the target stroke-related artery, as a result of which blood circulation is restored in the penumbra area, and, as a consequence, neuronal function is restored. Clinically, it manifests itself as regression of focal neurological deficits. If we consider the inefficiency of the thrombus extraction method, when the angiographic picture corresponds to the level of TICI 0 and TICI I, and clinically there is a deterioration in the patient’s condition in the form of an increase in neurological deficit and a narrowing of the consciousness level, then we can identify such factors as late presentation (more than 6 hours from the onset of clinical development of the Acute Carciovascular Accident), a state of hypercoagulation in which, after removal of the thrombus, there remains a high probability of re-thrombosis of the artery. Hemorrhagic transformation of the ischemic zone as a result of "luxurious perfusion" can be considered the main and main complication of thrombextraction. However, this issue is bipolar. So, if a patient with complete recanalization of the target artery (TICI III), with complete regression of neurological deficit, is diagnosed with hemorrhage by the type of per-diapedesis impregnation 24 hours after thrombus extraction, then this phenomenon should not be considered as a complication, but on the contrary, may be a marker of adequate recanalization and reperfusion of the brain. In cases where, after thrombus extraction, the patient experiences an increase in neurological deficit, a further narrowing of the level of consciousness, and an MSCT examination of the brain diagnoses a stroke-hematoma-type hemorrhage, then this clinical situation is considered as a complication of thrombus extraction.
5. Conclusions
In 80-85% of patients with acute cerebrovascular accident, ischemic damage to the brain substance occurs as a result of acute thrombotic occlusion of the internal carotid artery or intracranial artery of the carotid or vertebrobasilar basins. In this situation, the strategy of the occluded vessel recanalization in patients with ischemic stroke during the therapeutic window is a pathogenetically justified treatment method.The endovascular thrombextraction allowed us to achieve recanalization of the stroke-dependent artery – TICI IIb – III level, which was clinically manifested by regression of neurological focal symptoms. The use of the thrombus extraction method during the “therapeutic window” of acute ischemic stroke requires strict adherence to strict time criteria. Performing this surgery outside the 6-hour interval significantly worsens clinical results due to irreversible changes in the neurons of the penumbra zone, and may also cause hemorrhagic transformation of the cerebral ischemia zone. Hemorrhage of the type of perdiapedetic soaking, which was developed after thrombus extraction, with complete recanalization of the occluded intracranial artery (TICI III) and complete regression of the neurological deficit, should be considered as a marker of adequate recanalization and reperfusion. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
References
| [1] | Béjot Y, Bailly H, Durier J, et al. Epidemiology of stroke in Europe and trends for the 21st century. Presse Med 2016; 45: e391–e398. |
| [2] | Rothwell PM, Coull AJ, Silver LE, et al. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study). Lancet 2020; 366: 1773–1783. |
| [3] | Li L, Yiin GS, Geraghty OC, et al. Incidence, outcome, risk factors, and long-term prognosis of cryptogenic transient ischaemic attack and ischaemic stroke: a population-based study. Lancet Neurol 2015; 14: 903–913. |
| [4] | Amarenco P, Lavallée PC, Labreuche J, et al. One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med 2016; 374: 1533–1542. |
| [5] | Coelho AP, Lobo M, Gouveia R, Silveira D, Campos J, Augusto R, Coelho N, Canedo A. Overview of evidence on emergency carotid stenting in patients with acute ischemic stroke due to tandem occlusions: a systematic review and meta-analysis.J Cardiovasc Surg. 2019; 60: 693–702. doi: 10.23736/ S0021 -9509.18.10312-0. |
| [6] | Seet RCS, Wijdicks EFM, Rabinstein AA. Stroke from acute cervical internal carotid artery occlusion: treatment results and predictors of outcome. Arch Neurol. 2012; 69: 1615-1620. doi: 10.1001/archn eurol.2012.2569. |
| [7] | Papanagiotou P, Haussen DC, Turjman F, Labreuche J, Piotin M, Kastrup A, Steglich-Arnholm H, Holtmannspotter M, Taschner C, Eiden S, et al. Carotid stenting with antithrombotic agents and intracranialthrombectomy leads to the highest recanalization rate in patients with acute stroke with tandem lesions. JACC Cardiovasc Interv. 2018; 11: 1290–1299. doi: 10.1016/j.jcin.2018.05.036. |
| [8] | Savello A.V., Svistov D.V., Sorokoumov V.A. Intravascular methods of treating ischemic stroke: current status and prospects. \\ In Russian. Neurology, neuropsychiatry, psychosomatics. 2015; 7(4): 42–9. |
| [9] | Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous rtPa in ischemic stroke. Stroke. 2010; 41(10): 2254–8. |
| [10] | Berkhemer OA, Fransen PSS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Eng J Med. 2015; 372(1): 11–20. |
| [11] | Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Investigators endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372: 1009–18. |
| [12] | Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372: 1019–30. |
| [13] | Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372(24): 2296–306. |
| [14] | Saver JL, Goyal M, Bonafe A, Diener H-C, Levy EI, Pereira VM, et al. SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372: 2285–95. |
| [15] | Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49: e46–99. |
| [16] | Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: A systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. 2006; 37: 922–8. |
| [17] | Baek JM, Yoon W, Kim SK, Jung MY, Park MS, Kim JT, Kang HK. Acute basilar artery occlusion: Outcome of mechanical thrombectomy with solitaire stent within 8 hours of stroke onset. Am J Neuroradiol. 2014; 35(5): 989–93. |
| [18] | Radiology Soi: Guidelines for percutaneous transluminal angioplasty. J Vasc Interv Radiol 14: S209-S217, 2003. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML