-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 1875-1878
doi:10.5923/j.ajmms.20231312.12
Received: Nov. 16, 2023; Accepted: Nov. 28, 2023; Published: Dec. 6, 2023

Admissibility of Diapeutic Methods in the Surgical Treatment of Cystic Locations of the Liver
Umarkulov Zabur Zafarjonovich1, Khamidov Obid Abdurakhmanovich2, Davlatov Salim Sulaymonovich3
1Department of Medical Radiology and FPDO, Samarkand State Medical University, Samarkand, Uzbekistan
2Department of Medical Radiology and Faculty of Advanced Education, Samarkand State Medical University, Samarkand, Uzbekistan
3Department of Faculty and Hospital Surgery, Urology, Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Umarkulov Zabur Zafarjonovich, Department of Medical Radiology and FPDO, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. An analysis of modern literature shows that there are several directions in the treatment of liver cysts: traditional surgical interventions, endo-videosurgical methods and percutaneous puncture-drainage treatment of cysts under ultrasound or CT control with pre- and postoperative chemotherapy for parasitic liver cysts. The PAIR technique is widely used and approved by WHO. Nevertheless, attempts to modify percutaneous methods in order to improve treatment results continue. The purpose of the study is to improve the results of diagnosis and surgical treatment of patients with parasitic and non-parasitic liver cysts based on the use of diapeutic methods. Materials and methods of research. The study is based on a clinical and laboratory examination of 39 patients with cystic liver formations who underwent diapeutic and surgical interventions in the surgical department of the multidisciplinary clinic of Samarkand State Medical University for the period from 2016 to 2023. Research results. The immediate results of percutaneous interventions for cystic liver formations were assessed by the presence of intraoperative complications and unsatisfactory results in the early postoperative period. Conclusions. Analysis of the long-term results of diapeutic interventions for liver cysts showed the radicality of the method, being more preferable in patients with non-parasitic liver cysts and can be the operation of choice in patients with severe concomitant diseases.
Keywords: Liver cysts, Diapeutic interventions
Cite this paper: Umarkulov Zabur Zafarjonovich, Khamidov Obid Abdurakhmanovich, Davlatov Salim Sulaymonovich, Admissibility of Diapeutic Methods in the Surgical Treatment of Cystic Locations of the Liver, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 1875-1878. doi: 10.5923/j.ajmms.20231312.12.
Article Outline
1. Introduction
- An analysis of modern literature shows that there are several directions in the treatment of liver cysts: traditional surgical interventions, endovideosurgical methods and percutaneous puncture-drainage treatment of cysts under ultrasound or CT control with pre- and postoperative chemotherapy for parasitic liver cysts [1]. The PAIR technique is widely used and approved by WHO [3,5,8]. Nevertheless, attempts to modify percutaneous methods in order to improve treatment results continue. Thus, new types of minimally invasive interventions for echinococcosis have appeared - PEVAC, PAI, Örmeci, MoCaT. The PEVAC technique involves replacing the Seldinger drainage, which carries the risk of contamination of the puncture canal. PAI and Örmeci involve leaving the germicide in the cavity, which does not help reduce the residual cavity and increases the risk of suppuration [2,6,8]. According to the MoCaT method, the cyst is punctured immediately with a thick drainage, which is dangerous due to detachment of the chitinous membrane and rupture of the cyst [5,7]. Despite the fact that the authors of these methods declare their effectiveness and safety, the small number of patients and the short period of postoperative observation do not allow us to draw objective conclusions. Thus, the decision on the choice of the optimal method of surgical intervention and the method of its implementation remain relevant.
2. The Purpose of the Study
- The purpose of the study is to improve the results of diagnosis and surgical treatment of patients with parasitic and non-parasitic liver cysts based on the use of diapeutic methods.
3. Materials and Methods of Research
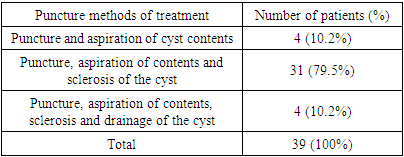
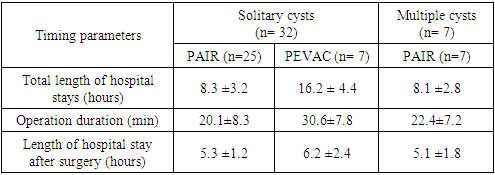
- The study is based on a clinical and laboratory examination of 39 patients with cystic liver formations who underwent diapeutic and surgical interventions in the surgical department of the multidisciplinary clinic of Samarkand State Medical University for the period from 2016 to 2023.Puncture-drainage cystectomy methods known as PAIR (Punction-Aspiration-Injection-Reaspiration percutaneous method of puncture treatment) and PEVAC (Percutaneos-Evacuation of cyst contens percutaneous method of puncture evacuation and drainage of the cavity). Percutaneous puncture and sclerotherapy of non-parasitic liver cysts under ultrasound guidance was performed in 39 patients. A total of 6 (15.4%) men and 33 (84.6%) women with serous liver cysts from 4 to 15 cm in diameter were operated on. Solitary cysts, localized in the vast majority of cases in the right lobe of the liver, were diagnosed in 4 (10.2%) men and 17 (43.6%) women; multiple cysts were diagnosed in 2 (5.1%) men and 25 (25, respectively). 64.1%) patients.Percutaneous puncture and sclerosis of liver cysts under ultrasound control were considered indicated in the presence of solitary and multiple true non-parasitic liver cysts measuring 5 cm or more in diameter in the presence of contraindications to laparoscopic operations. Echosonographically, true cysts were round or oval cavities limited by a thin wall (0.1 - 0.2 cm) without echogenicity of the internal space with clear, even contours and the presence of a clearly visible posterior wall, the absence of internal reflections and a characteristic increase in echo signals directly behind cystic formation. In the presence of an intraluminal septum of the cyst, a characteristic spotty pattern was visualized. Intraluminal echo signals indicated hemorrhage into the cyst cavity or its infection.Percutaneous puncture was also performed in patients with severe concomitant pathology, who were contraindicated for operations through laparotomy access.The procedure was carried out in an operating room equipped with high technology, including an ALOCA SSD-630 ultrasound machine (Japan). Depending on the location of the cyst, the patient was placed in a special position in order to prevent the needle from passing through the pleural sinus and for convenient manipulation without damaging the hollow organs of the abdominal cavity.In 4 (10.2%) patients, only aspiration of the cyst contents was performed (Table 1).
|
4. Research Results
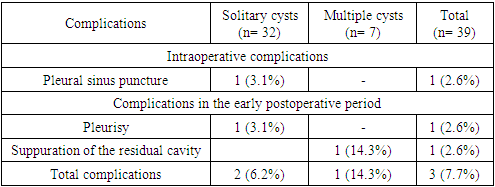
- The immediate results of percutaneous interventions for cystic liver formations were assessed by the presence of intraoperative complications and unsatisfactory results in the early postoperative period.Intraoperative complications were assessed using the following indicators:- bleeding- damage to the bile ducts and bile leakage- puncture of the pleural sinus- damage to hollow organs- allergic complications.Unsatisfactory results in the early postoperative period were assessed by the following indicators:- contamination of the abdominal cavity- infection of the residual cavity- biliary peritonitis- subphrenic abscess- pleurisy.Intraoperative complications were noted in 3 patients with liver echinococcosis. As noted in Chapter 3 of the dissertation, in 2 cases of patients with liver echinococcosis during diapeutic intervention due to profuse bleeding in one case and profuse bile leakage in another case due to direct puncture of the lumen of the gallbladder through the lumen of the cyst, emergency laparotomy was required with continuation of the operation in an open manner. The puncture of the gallbladder wall was assessed according to intraoperative sonography, which revealed a sharp shrinkage of the tense bladder. In 1 patient, during diapeutic intervention, an allergic reaction was noted in the form of skin hyperemia, urticaria, and mild tachycardia. The symptoms resolved on the operating table with the use of desensitizing drugs and glucocorticosteroids. We did not observe such reactions in the postoperative period. In other cases, not a single patient developed any significant allergic reaction, not to mention anaphylactic shock. A special role in the absence of pronounced allergic reactions is played by the fact that all patients underwent desensitization therapy on an outpatient basis before the surgical period. Before the operation, antihistamines were started for 10 days, then glucocorticosteroids were started three days before the operation.Intraoperatively, we did not notice a puncture of the pleural sinus or damage to the hollow organs, but in the early postoperative period, exudative pleurisy on the right was noted in 1 patient. Perhaps there was a puncture of the pleural sinus during percutaneous puncture of a non-parasitic cyst localized in the diaphragmatic surface of the VII segment of the liver. In 2 cases, 3-4 days after catheterization drainage of the cyst, suppuration of the residual cavity occurred. Of these, in 1 case after catheterization and drainage of a non-parasitic cyst, which required urgent hospitalization of the patient and repeated puncture drainage. It should be noted that there is an extremely low level of complications, of which only 1 (2.6% of 39 patients) can be regarded as caused by the procedure, or more precisely by non-compliance with the third of the above rules (Table 2).
|
|
5. Conclusions
- Analysis of percutaneous puncture methods of surgical operations has revealed wide possibilities for treatment and diagnostic tactics for managing patients with liver cysts, which allows, in most cases, to perform surgical intervention in conditions more favorable for the patient. Patients with non-parasitic solitary cysts or a dominant cyst in polycystic disease up to 5 cm in diameter require dynamic monitoring. Indications for puncture cystectomies are non-parasitic solitary and multiple liver cysts measuring 5 cm or more. Contraindications are the localization of cysts on the posterior surface of the liver, as well as intraparenchymal location.Percutaneous puncture cystectomy is a modern minimally invasive method of surgical treatment of parasitic and non-parasitic liver cysts, which has great clinical effectiveness, which has an important social significance and economic effect in comparison with laparoscopic and traditional methods. The advantages of the intervention include early postoperative rehabilitation of patients, reduction or prevention of various types of complications characteristic of laparoscopic and open traditional operations, as well as a reduction in hospital stay.Analysis of the long-term results of diapeutic interventions for liver cysts showed the radicality of the method, being more preferable in patients with non-parasitic liver cysts and can be the operation of choice in patients with severe concomitant diseases.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML