-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 1842-1846
doi:10.5923/j.ajmms.20231312.04
Received: Oct. 24, 2023; Accepted: Nov. 10, 2023; Published: Dec. 2, 2023

Clinical and Economic Efficiency of Percutaneous Nephrolithotripsy in Children in a Short-Term Hospital
Boboev Alisher Shukrullaevich1, Rizaev Jasur Alimdjanovich2, Abdurizaev Abdumalik Abdugaffarovich1, 2, Umirov Azamat Abduraimovich1
1Private Medical Center "Dr. Boboev Health Center", Kitab, Republic of Uzbekistan
2Samarkand State Medical University, Samarkand, Republic of Uzbekistan
Correspondence to: Boboev Alisher Shukrullaevich, Private Medical Center "Dr. Boboev Health Center", Kitab, Republic of Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective. To evaluate the clinical and economic effectiveness of percutaneous nephrolithotripsy in children with kidney stones in a short-stay hospital. Materials and Methods. A comparative analysis of the direct medical costs of percutaneous nephrolithotripsy in children in a short-stay unit and during hospitalization in a regular hospital was performed using the cost minimization analysis method. Results. Endourological treatment of children with urolithiasis in a short-stay hospital turned out to be economically favorable, which allowed saving more finances. It was found that the differences in direct medical costs between the two groups of patients were statistically significant (p=0.0018) in favor of the group of patients treated in a short-stay hospital. Conclusion. Our clinical and economic analysis has shown that percutaneous stone removal in children with urolithiasis in the conditions of short stay hospital is more economically effective.
Keywords: Cost effectiveness, Direct medical costs, Urolithiasis, Children, Short-stay hospital, Percutaneous nephrolithotripsy
Cite this paper: Boboev Alisher Shukrullaevich, Rizaev Jasur Alimdjanovich, Abdurizaev Abdumalik Abdugaffarovich, Umirov Azamat Abduraimovich, Clinical and Economic Efficiency of Percutaneous Nephrolithotripsy in Children in a Short-Term Hospital, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 1842-1846. doi: 10.5923/j.ajmms.20231312.04.
Article Outline
1. Introduction
- Kidney stones are one of the most common diseases of the urinary tract in all age groups [1,2]. In the last few decades, the prevalence of kidney stones in the liver has been increasing with an increase rate of 10.6% per year [3,4]. The main goal of treating kidney stones in children, as in adults, is to eliminate stones and improve the quality of life of patients [5]. Currently, there are many options for the treatment of kidney stones in children - from non-invasive approaches, such as pharmacological treatment, to less invasive ones, such as extracorporeal shock wave lithotripsy (ESWL), retrograde intrarenal surgery (RIRS) or percutaneous nephrolithotripsy (PNLT) [6,7].Over the past decade, the structure of surgical interventions for urological diseases has changed in favor of minimally invasive urology, which has become the method of choice for the treatment of urolithiasis and gives better clinical results than traditional methods of treatment. At the same time, the economic parameters characterizing the impact of new technologies on the total costs of the treatment process, as well as on their structure, have been studied much less. The relevance of the economic assessment of the effectiveness of modern methods of diagnosis and treatment of patients is due to several factors: firstly, the emergence of alternative methods of treatment of the same disease; secondly, the emergence of new expensive medical technologies and an increase in the cost of medical services; thirdly, the relative limited funds spent on healthcare.Currently, more and more attention is being paid to optimizing the quality of medical care and reducing healthcare costs. However, there is limited data on how best to achieve these goals with such a common and resource-intensive disease as urolithiasis in children.Studies conducted by Pasquali S.K. have established that one of the factors associated with high costs is an increase in the duration of hospital stay [8]. In conditions of scarce financing of the healthcare system, the most difficult and costly link requiring unconditional optimization is inpatient care [9]. It is the duration of hospitalization that is one of the key factors determining hospital costs, and a significant component of cost containment is reducing the length of stay [10].The purpose of this study was to evaluate the clinical and economic efficiency of percutaneous nephrolithotripsy in children with kidney stones in a short-term hospital.
2. Material and Methods
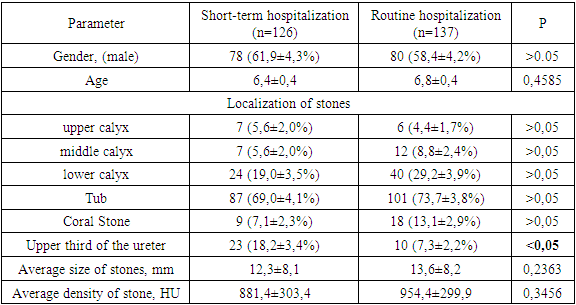
- In the period from 2018 to 2022, 263 percutaneous nephrolithotripsies were performed in children suffering from urolithiasis at the private medical center "Dr. Boboev Health Center". Of these, 126 (47.9%) were treated in a short–stay hospital, and 137 (52.1%) were treated with a regular hospitalization period. In our study, we limited the duration of the "short-term hospital stay" to the patient's stay in the hospital for no more than 36 hours.60 patients were selected and included by random sampling for the purpose of clinical and economic analysis: 30 patients from the main group and 30 patients from the control group.Using the "cost minimization analysis" analysis method, the amounts of direct medical costs for percutaneous nephrolithotripsy in children during hospitalization in a short-term hospital were determined in comparison with conventional hospitalization.The analysis of direct medical costs at PNLT was carried out on the basis of the register of services rendered to patients and data from profitability tables in the private medical center "Dr. Boboev Health Center".Direct medical costs were calculated according to the formula: DMC =A +B+C,where DMC is direct medical costs (direct medical cost), sum.;A is the cost of percutaneous nephrolithotripsy, sum;B – costs of drug therapy, sum;C – the cost of hospital stay, sum.The calculation of the cost difference of the compared treatment conditions was carried out according to the following formula:CMA = DC1– DC2,where:SMA – Cost Minimization Analysis — an indicator of the difference in the costs of comparable treatment regimens;DC1 – direct costs of treatment in a short-stay hospital;DC2 is the direct cost of treatment for routine hospitalization.As criteria for clinical effectiveness, we will define the complete removal of a stone (Stone free).Common indications for the active removal of kidney stones and ureter were concretions causing severe pain, hematuria, obstruction and inflammation of the upper urinary tract, impaired kidney function. The choice of the treatment method was carried out according to the national standards for the diagnosis and treatment of urological diseases and the recommendations of the European Association of Urologists for the treatment of ICD [11].The selection of patients for treatment in a short-term hospital was carried out by a multidisciplinary team of specialists, which included a pediatrician, an anesthesiologist and a urologist. Patients of the main group were hospitalized on the day of endourological intervention and discharged on the next day after the procedure in the absence of indications for prolongation of hospitalization. The average duration of hospitalization of patients in the control group was 2.7±1.4 bed days.The frequency of complete release from stones (SFR) during PNLT was detected in 121 (96.0±1.7%) patients treated in a short-term hospital, which did not have a statistically significant difference with the standard hospitalization group, where the same indicator was 96.3± 1.6% and was observed in 132 patients (p>0.05). Also, the analysis of postoperative complications showed that the treatment of patients in a short-term hospital does not lead to an increase in the frequency of postoperative complications.Demographic indicators and clinical characteristics of the patients included in the study are presented in Table 1.
|
3. Statistical Analysis
- For all patients included in the study, the method of descriptive statistics was applied. Quantitative variables were described as an average value with a standard error of the average value. Absolute and relative (%) frequencies were used to describe qualitative variables. During statistical processing and analysis of the results obtained, the calculation of average values (Meap), minimum (Min), maximum (Max) values and standard deviation (SD) was carried out. The distribution was described by calculating the Median, the 1st quartile (Q25) and the 3rd (Q75) quartile. Since the distribution of values of the studied variables differed from normal, the Mann-Whitney criterion was used to assess the significance of intergroup differences. At p≤0.05, the presence of differences between the groups on the studied trait was considered significant.
4. Results
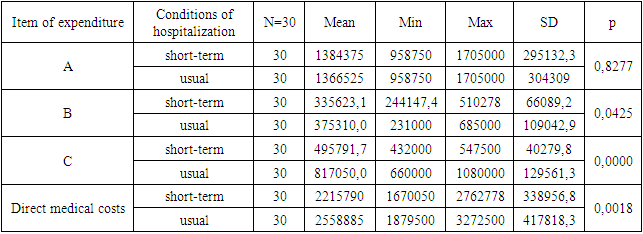
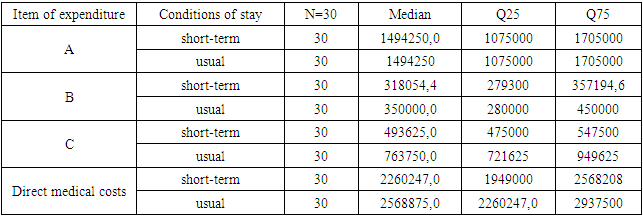
- Table 2 presents the results of the analysis of direct medical costs during percutaneous nephrolithotripsy in children under the compared conditions of hospitalization. The average expenses (Mean) for endourological intervention (A) in a short–stay hospital amounted to 1384375.0 soums, with normal hospitalization - 1366525.0 soums: with the same minimum and maximum values. The application of the Mann–Whitney test showed that these differences were not significant (p=0.8277).
|
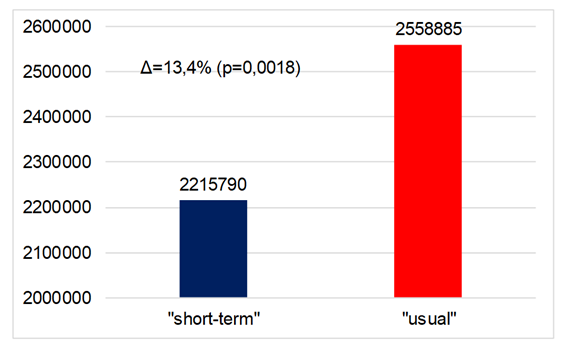 | Figure 1. Average values of direct medical costs in case of PNLT |
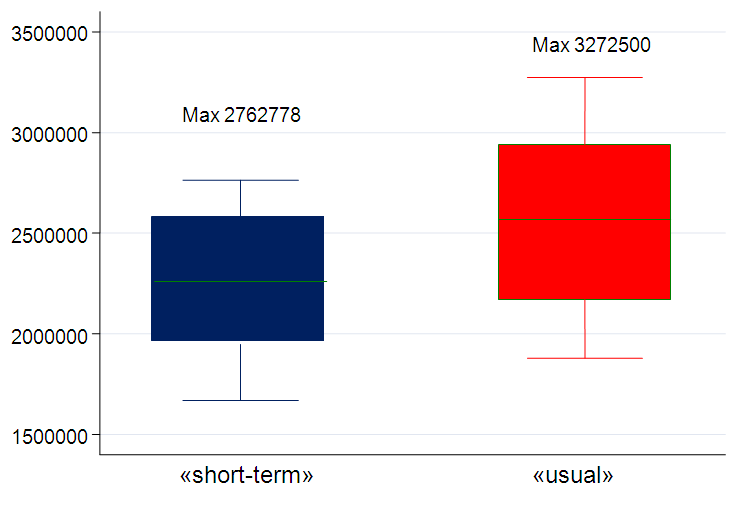 | Figure 2. Direct medical costs for PNLT |
5. Discussion
- Although urolithiasis is a relatively common disease in adults, which affects from 3 to 5% of the population [1], from an epidemiological point of view, it is noteworthy that children make up only 2-3% of all patients with urolithiasis [2,3]. On the other hand, the number of patients suffering from urolithiasis increases every year. The incidence of ICD in children depends on the level of economic development; thus, in developed countries, the incidence ranges from 1 to 5%, and in developing countries - from 5 to 15% [1].The socio-economic significance of this disease for health care is primarily due to the high frequency of emergency and repeated hospitalization due to frequent relapse, long periods of inpatient treatment and loss of work capacity [12]. New and more complex methods of treatment are accompanied by an increasingly widespread use and increasing dependence on increasingly expensive medical and surgical interventions. The use of these methods of treatment leads to an increase in the burden on medical systems, which are already experiencing significant difficulties.To date, the main direction of the development of the healthcare system in the world is to increase the efficiency of resource use through the introduction of resource-saving technologies and the development of hospital-substituting forms of medical care to the population. At the beginning of the new millennium, significant efforts were already made to promote one-day surgery [13], and recent efforts to reduce the length of hospital stay and improve the quality of postoperative recovery have led to the fact that the principles of one-day surgery have become fundamental in modern patient care. In conditions of limited funding, as well as the irrational use of material resources available in the healthcare system, the search for new, effective approaches to the organization of medical and medicinal care becomes urgent. As a modern scientific basis for solving the problem of optimizing drug care for patients, clinical and economic studies can be used, assuming that the characteristics of the effectiveness, safety and economic feasibility of using certain medicines are taken into account. The use of methods of clinical and economic analysis at different levels of the healthcare system makes it possible to clearly justify the allocation of budget funds and choose the most effective and acceptable alternative from the compared medical technologies [14].The economic evaluation of the effectiveness of a particular treatment method is the ratio of the costs of their implementation and their effectiveness [15,16]. At the same time, clinical and economic analysis (CEA) is a process of comparing two or more medical technologies in terms of their results and costs. The application of the results of clinical and economic analysis makes it possible to use not only effective, but also economically feasible methods [16].Cost-effectiveness, which characterizes the rationality of spending resources, is the most important component of the process of providing medical care [15]. This indicator can be estimated using the methodology of clinical and economic analysis. The relevance of this methodology is felt at all levels of healthcare; the users of clinical and economic analysis are health management bodies, territorial mandatory medical insurance funds, manufacturers of medicines and medical equipment, medical organizations, consumers of medicines and technologies (doctors, pharmacists, patients) [10].Economic efficiency is considered in two directions: firstly, it is the use of various resources; secondly, the impact of healthcare on the development of social production as a whole.The following 4 methods of economic evaluation of the effectiveness of treatment are most often used: cost minimization analysis, cost effectiveness analysis [14], cost utility analysis and cost benefit analysis [14]. The cost minimization analysis that we have resorted to in our work is limited to cases when the compared treatment methods have the same clinical effectiveness. In this case, the method of treatment that requires less costs is considered economically preferable. In this paper, we did not compare treatment methods, but compared 2 different programs of inpatient stay of patients who underwent PNLT. Of course, the clinical effectiveness of PNLT does not depend on the hospitalization option. According to the results of our study, endourological treatment of children with urolithiasis in a short-term hospital turned out to be more cost-effective and cost-effective, which allowed saving more money. The reduction in the duration of hospitalization, accompanied by a reduction in the cost of maintaining the patient in the hospital, led to significant financial savings (the difference between hospitalization modes was 13.4% in favor of hospitalization in a short-term hospital).
6. Conclusions
- Our clinical and economic analysis has shown that percutaneous removal of stones in children with urolithiasis in a short-term hospital is more cost-effective and safe. The presented results indicate the clinical and economic feasibility of a wider introduction of percutaneous nephrolithotripsy in children in a short-stay hospital.
References
| [1] | Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. //Kidney Int. (2003) 63: 1817–23. doi: 10.1046/j.1523-1755.2003.00917.x. |
| [2] | Liu Y., Chen Y., Liao B., Luo D., Wang K., Li H., Zeng G., Epidemiology of urolithiasis in Asia, // Asian J. Urol., 2018, 5, 205–214. |
| [3] | Resorlu B, Sancak EB, Resorlu M, Gulpinar MT, Adam G, Akbas A, et al. Retrograde intrarenal surgery in paediatric patients. // World J Nephrol. (2014) 3: 193–7. doi: 10.5527/wjn.v3.i4.193. |
| [4] | Ikhtiyarova, G. A., Dustova, N. K., Khasanova M. A., Suleymanova G. S., & Davlatov, S. S. (2021). Pathomorphological changes of the placenta in pregnant women infected with coronavirus COVID-19. International Journal of Pharmaceutical Research, 13(1), 1935-1942. doi: 10.31838/ijpr/2021.13.01.283. |
| [5] | Routh J.C., D.A. Graham, C.P. Nelson, Epidemiological trends in pediatric urolithiasis at United States freestanding pediatric hospitals, J. Urol. 184 (2010) 1100–1105. |
| [6] | Caione P., Collura G., Innocenzi M., De Dominicis M., Nappo S.G., Capozza N., Percutaneous endoscopic treatment for urinary stones in pediatric patients: where we are now // Transl. Pediatr., 2016, 5, 266. |
| [7] | D. P´erez-Fentes, B. Blanco-Gomez, ´ C. García-Freire, Micropercutaneous nephrolithotomy. A new therapeutic option for pediatric renal lithiasis, Actas Urol. Esp. 38 (2014) 483–487. |
| [8] | Bozorov, A.G., Ikhtiyarova, G.A., & Davlatov, S.S. (2020). Biochemical markers for prediction of premature labor in urogenital infections // International Journal of Pharmaceutical Research, 12, – P. 4894–4897. DOI: 10.31838/ijpr/2021.13.01.674. |
| [9] | G. Zeng, W. Zhu, W. Lam, Miniaturised percutaneous nephrolithotomy: its role in the treatment of urolithiasis and our experience, Asian J. Urol. 5 (2018) 295–302. |
| [10] | Pasquali S.K., He X., Jacobs M.L., et al. Excess costs associated with complications and prolonged length of stay after congenital heart surgery. // Ann Thorac Surg 2014; 98: 1660–6. doi:10.1016/j.athoracsur.2014.06.032. |
| [11] | Tekgul S., Dogan H.S`., Erdem E. Urinary stone disease, guidelines on pediatric urology. EAU Urol Guidel 2015; 56-58. |
| [12] | NHS Modernisation Agency. 10 High Impact Changes for Service Improvement and Delivery. 2004. https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/10-High-Impact- Changes.pdf (accessed 30/04/ 2018). |
| [13] | Doubilet P., Weinstein M.C., McNeil B.J. Use and misuse of the term «Cost Effective» in medicine. New England Journal of Medicine. 1986; 314 (4): 253–6. DOI:10.1056/NEJM198601233140421. |
| [14] | Bakhodirova Sh. F., Ikhtiyarova G. A., Aslonova M. J., Davlatov S. S. (2020). Features of perinatal outcomes in women after supporting reproductive technologies. European Journal of Molecular & Clinical Medicine, 7(2), 6350-6356. |
| [15] | Jönsson B. Measurement of health outcome and associated costs in cardiovascular disease. Eur Heart J. 1996; 17 Suppl A: 2–7. |
| [16] | Bowling A. Research methods in health: investigating health and health services. 3. ed., repr. -Maidenhead: Open Univ. Press; 2010. 525 с. ISBN: 978-0-335-23364-9. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML