-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(12): 1838-1841
doi:10.5923/j.ajmms.20231312.03
Received: Oct. 20, 2023; Accepted: Nov. 17, 2023; Published: Dec. 2, 2023

Assessment of Interferon Status in Patients with Type 2 Diabetes Mellitus Infected with COVID-19 Infection
Aslonova Marjona Ramazonovna
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Aslonova Marjona Ramazonovna, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. In 2020, the world is facing an unprecedented public health challenge due to the invasion of the novel coronavirus SARS CоV-2. It is also a challenge for the health systems of all countries of the world. Purpose. Study and assessment of interferon status in patients with type 2 diabetes mellitus infected with Covid-19. Methods. The study included 103 patients hospitalized with a diagnosis of SARS-CoV-2 pneumonia and diabetes mellitus in the Bukhara Regional Infectious Diseases Hospital, which was reorganized into the Covid Center 2021-2022. The diagnosis was made on the basis of clinical, epidemiological, objective and laboratory (ELISA, PCR) data. The study of interferon (INF-α, INF-γ) status in the blood of patients was carried out in the laboratory of immunomorphology of the Institute of Human Immunology and Genomics of the Academy of Sciences of the Republic of Uzbekistan. Results. Analysis of the level of serum circulating interferons showed a decrease in IFNα synthesis by 2.3 times in patients of group 1 (p<0.001), by 2.0 times in patients of group 2 (p<0.001), by 1.38 times in patients of group 3. group (p<0.05). Analysis of the level of INF-γ showed a decrease in IFNγ synthesis by 1.5 times in patients of group 1 (p<0.05), by 1.79 times in patients of group 2 (p<0.01), by 1.6 times in patients of group 3 (p<0.05). Conclusions. Thus, the study of interferon status in patients with coronavirus infection against the background of type 2 diabetes showed that IFN-γ- is an indicator of the severity of this disease.
Keywords: SARS CоV-2, Pneumonia, Type 2 diabetes mellitus, Pneumonia, Interferon
Cite this paper: Aslonova Marjona Ramazonovna, Assessment of Interferon Status in Patients with Type 2 Diabetes Mellitus Infected with COVID-19 Infection, American Journal of Medicine and Medical Sciences, Vol. 13 No. 12, 2023, pp. 1838-1841. doi: 10.5923/j.ajmms.20231312.03.
1. Introduction
- Coronavirus disease 2019 (COVID-19) is a newly recognized infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was recently declared a pandemic [9]. The death toll from COVID-19 is on the rise. As of 21 April 2020, 2,397,217 patients have been confirmed worldwide and 162,956 have died. A total of 84,250 cases have been diagnosed in China, of which 4,642 have died [10]. Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), has rapidly reached pandemic proportions. SARS-CoV-2 is a member of the betacoronavirus family, as well as SARS-CoV (severe acute respiratory syndrome coronavirus) and MERS-CoV (Middle East respiratory syndrome-associated coronavirus). Since the beginning of 2020, the number of confirmed cases of COVID-19 worldwide has risen sharply and by March 2020 exceeded one million [13]. Concomitant diseases are a serious risk factor for more severe course of coronavirus pneumonia and death of the disease 50 [7].For SARS, chronic heart disease, diabetes, chronic hepatitis B, malignancy, and chronic lung disease were the main adverse prognostic factors [9]. At the very beginning of the epidemic, diseases were isolated, increasing mortality due to COVID-19. To data group diseases include hypertension, obesity, diabetes mellitus (DM), cardiovascular disease, diseases of the kidneys and liver [1].DM worsens the outcome of most acute and chronic diseases leading to shortened life expectancy. Mortality from infectious diseases is also higher in patients with diabetes, especially with the development of pneumonia or sepsis [2]. Type 2 diabetes (DM2) is the second most common comorbid pathology in COVID-19[12]. A meta-analysis of studies describing the characteristics of patients depending on the severity of COVID-19 in China showed that DM increases the likelihood of adverse disease outcomes by 2-3 times [15]. In a US study in 5,700 patients with COVID-19 (mean age 63; 39.7% women) most frequent comorbidities were arterial hypertension (56.6%), obesity (41.7%) and diabetes (33.8%) [5].The prevalence of DM in patients with COVID-19 varies in different countries and ranges from 11 to 45%. Large studies have demonstrated a higher incidence of DM in a cohort of patients with severe disease (16.3%) than among patients with mild disease (6.9%) [4]. According to C. Huang et al. [3], 72% of patients with COVID-19 and comorbidities (including DM) needed in intensive care unit hospitalization compared to 37% without comorbidities. European data also report that DM was more frequently reported in the ICU group [8].The presence of diabetes in a patient increases the risk of hospitalization. death by 2.85 times [3], which is comparable in terms of risk to patients with oncohematological profile (by 5.35 times) and obese patients (by 3.2 times). In a large epidemiological study by the Chinese Center for Disease Control, the mortality rate from COVID-19 with diabetes was 7.3%, which is significantly higher than the mortality from COVID-19 without any comorbidities (0.9%) with an overall mortality rate of 2 .3% [2].Neutrophils, C-reactive protein, and some cytokines (such as IL-6, TNF, IL-10) increase with COVID-19, and this increase correlates with disease severity and death [8]. In severe disease, the same protein levels were found, and an increase in inflammatory cytokines correlated with a decrease in T CD4 + and T CD8 + lymphocytes and a decrease in IFNγ production. B-lymphocytes do not appear to be susceptible to disease regardless of severity [3]. These characteristics observed in patients indicate that COVID-19 may be mediated by an intense inflammatory process that depends on the severity of the disease. As with SARS-CoV-1 and MERS, this increase in cytokine levels, known as cytokine storm, may be related to the pathogenesis of the disease [3]. Against the background of the COVID-19 pandemic, an increase in the number of deaths of the population in all countries is noted. At the same time, separate groups of patients are distinguished, in which mortality significantly exceeds the average. One of these groups, of course, includes patients with diabetes mellitus (DM). Numerous studies in various countries have demonstrated a higher risk of COVID-19 infection in diabetic patients, as well as a more severe course of the disease and a high mortality rate [15].
2. Material and Methods
- The study included 103 patients hospitalized for SARS-COV-2 pneumonia at the Bukhara Regional Infectious Diseases Hospital, which was reorganized into the Covid Center. Of all those hospitalized for SARS-COV-2 pneumonia against the background of type 2 diabetes, there were 35 patients with severe pneumonia (group 1), and 33 with moderate severity (group 2). The comparison group (group 3) consisted of 35 patients with SARS-COV-2 pneumonia who did not suffer from diabetes. The control group consisted of 30 healthy people of the appropriate age. The average age of patients in group 1 was 60.2 ± 2.2 years, in patients in group 2 it was 50.0 ± 2.0 years, and in the comparison group it was 52.4 ± 2.0 years. In the control group, the average age was 54.0 ± 2.0 years. The average time of stay in the hospital was: group 1 - 8.7 ± 0.47 days, group 2 - 6.4 ± 0.26 days, group 3 - 10.6 ± 0.45 days.Immunological studies of the patients' blood were carried out in the laboratory of immunomorphology of the Institute of Human Immunology and Genomics of the Academy of Sciences of the Republic of Uzbekistan. Indicators of interferon (INF-α INF-γ) status in the blood were studied. The test system was used by the manufacturer, JSC Vector Best (St. Petersburg). Determination of cytokine levels was carried out according to the attached instructions. The operating principle of the set is according to the attached instructions. The kit uses a “sandwich” version of an enzyme-linked immunosorbent assay. To implement this option, two monoclonal antibodies with different epitope specificities for the studied cytokines were used. One of them is immobilized on the solid phase (inner surface of the wells), the second is conjugated with peroxidase. At the first stage of the analysis, contained in calibration and test samples, binds to antibodies immobilized on the inner surface of the wells. At the second stage of the analysis, the immobilized interleukin interacts with the conjugate of the second antibodies - peroxidase. The amount of bound conjugate is directly proportional to the amount of interleukin in the test sample. During incubation with the substrate mixture, the solution in the wells becomes colored. The degree of coloring is directly proportional to the amount of bound labeled antibodies. After measuring the optical density of the solution in the wells, the concentration of the corresponding interleukin in the samples being determined is calculated based on the calibration curve.
3. Results
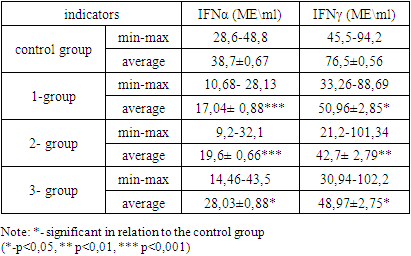
- Patients with type 2 diabetes are among the most vulnerable group of patients with COVID-19. Mortality among patients with type 2 diabetes is 2 times higher compared with individuals without a history of DM, with a predominant predominance of women in the proportion of deaths. Sick DM2 had a high incidence of associated diseases (IHD, CHF, CKD, obesity) and were naturally characterized by more severe course of COVID-19, with a proportion of mechanical ventilation and transfers to the ICU 1.3 times higher compared to the group without DM. Of the cardiovascular diseases, hypertension, compared with coronary artery disease and chronic heart failure, was the most important in the risk of death for patients with type 2 diabetes. In patients with type 2 diabetes, the risk of death is detected at an earlier age than in individuals without diabetes (66 years vs. 71 years). The cut-off points according to the ROC analysis of the main parameters reflecting the severity of the course of COVID-19 (CRP, LDH, D-dimer) are lower in the DM2 group than in the control group [16,18].Studies conducted in Uzbekistan showed that COVID-19 was the cause of deaths in 6.7% of cases, the COVID-19 pandemic caused a significant increase in mortality - 1.5 times among patients with diabetes, mainly due to acute cardiovascular accidents, as well as accelerating the progression of chronic complications SD [17]. Taking into account the above results of studies to study the state of immunity, in particular interferon status, a study was conducted to determine the level of INF-α and INF-γ in the blood serum of patients suffering from SARS-COV-2 pneumonia in association with type 2 diabetes mellitus.The study included 103 patients hospitalized for SARS-COV-2 pneumonia at the Bukhara Regional Infectious Diseases Hospital, which was reorganized into the Covid Center. Of all those hospitalized for SARS-COV-2 pneumonia against the background of type 2 diabetes, patients with severe pneumonia amounted to -35 (group 1), with moderate severity - 33 (group 2). The comparison group (group 3) consisted of 35 patients with SARS-COV-2 pneumonia who did not suffer from diabetes. The control group consisted of 30 healthy people of the corresponding age.The average age of patients in group 1 was 60.2 ± 2.2 years, in patients of group 2 - 50.0 ± 2.0 years, and in the comparison group - 52.4 ± 2.0 years. In the control, the mean age was 54.0 ± 2.0 years. The average time of stay in the hospital was in patients: group 1 - 8.7 ± 0.47 days, group 2 - 6.4 ± 0.26 days, group 3 - 10.6 ± 0.45 days.Analysis of the level of serum circulating interferons showed a decrease in IFNα synthesis by 2.3 times in patients of group 1 (p<0.001), by 2.0 times in patients of group 2 (p<0.001), by 1.38 times in patients of group 3 groups (p<0.05), Table 1.
|
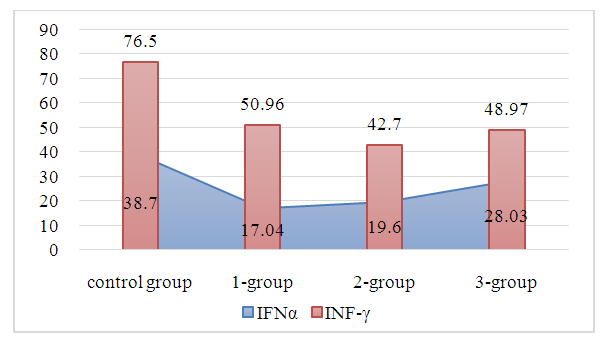 | Figure 1. Interferons in coronavirus infection depending on the severity of pneumonia and the presence of type 2 diabetes mellitus |
4. Conclusions
- Thus, the study of interferon status in patients with coronavirus infection against the background of type 2 diabetes showed the dependence of the outcome of the disease on multifactors:- the presence of diabetes and chronic non-communicable diseases of other organs;- duration of use of antidiabetic drugs;- glucocorticosteroid therapy.At the same time, IFN-γ- is an indicator of the severity of coronavirus infection in patients with type 2 diabetes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML