-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1817-1820
doi:10.5923/j.ajmms.20231311.46
Received: Nov. 12, 2023; Accepted: Nov. 27, 2023; Published: Nov. 29, 2023

Features of the Clinical Course of Bronchoobstructive Syndrome in Children, Depending on Etiological Factors
H. E. Turakulova1, N. D. Azizova2, F. M. Shamsiev2
1Andijan State Medical Institute, Uzbekistan
2Republican Specialized Scientific and Practical Medical Center of Pediatrics of the Ministry of Health of the Republic of Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In the past decade, obstructive bronchitis has seen a rise in prevalence among pediatric respiratory diseases, marked by recurrent episodes and potential progression to bronchial asthma. This retrospective study, spanning 2015-2019, delves into the medical histories of 6965 children, focusing on 1208 cases diagnosed with bronchoobstructive syndrome. The analysis categorizes these cases into three groups: community-acquired acute pneumonia with obstructive syndrome, acute obstructive bronchitis, and recurrent bronchitis with bronchoobstructive syndrome. The research investigates risk factors and clinical manifestations, revealing that acute obstructive bronchitis is more prevalent in children under one year and is often associated with deficient conditions and complex premorbid background. Recurrent bronchitis with bronchoobstructive syndrome exhibits acute onset, paroxysmal cough, and vacute respiratory diseases and auscultative signs dependent on bronchial mucosal damage. Notably, all recurrent bronchitis with bronchoobstructive syndrome cases present signs of bronchial obstruction in X-ray examinations. The virological analysis identifies respiratory syncytial virus as a predominant etiological factor, notably more prevalent in the autumn-winter seasons. The severity of bronchial obstruction correlates with detecting respiratory syncytial virus, both isolated and in combination with bacterial infections. MS-viral infection, especially in conjunction with bacterial infections, emerges as a predictor of severe disease, occurring significantly more frequently in grade 3 severity of bronchial obstruction compared to grade 1. In conclusion, this study sheds light on the intricate relationship between respiratory infections, especially respiratory syncytial virus, and the development of bronchoobstructive syndrome in children. Understanding these factors and mechanisms is crucial for effective management and preventive strategies in pediatric respiratory care.
Keywords: Obstructive bronchitis, Bronchoobstructive syndrome, Pediatric respiratory diseases, Respiratory syncytial virus, Risk factors, Recurrent bronchitis, Bronchial asthma, Immune status, Etiological factors, Clinical manifestations
Cite this paper: H. E. Turakulova, N. D. Azizova, F. M. Shamsiev, Features of the Clinical Course of Bronchoobstructive Syndrome in Children, Depending on Etiological Factors, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1817-1820. doi: 10.5923/j.ajmms.20231311.46.
1. Introduction
- In the last decade, there has been an increase in the proportion of obstructive bronchitis in the structure of respiratory damage [1,4], associated with an increase in the number of frequently ill children and the impact of adverse environmental factors. Bronchoobstructive syndrome occurs in 25-31% of children hospitalized for acute respiratory viral infection [2,3].The viruses that most often cause obstructive bronchitis include respiratory syncytial virus (50%), parainfluenza virus, less often influenza virus, and adenovirus. A significant role of mixed viral infections has been noted [5,6]. In 30-50% of cases, episodes of bronchial obstruction recur with repeated respiratory diseases, and in 15-30% of cases, typical bronchial asthma is formed [4]. The etiological role of respiratory syncytial and chlamydial infections was noted in recurrent bronchial obstruction [4,6].In the immune status of children with obstructive bronchitis, acute respiratory diseases or disorders are recorded in the form of changes in the functional activity of phagocytic cells, a deficiency of the NK cell system, a decrease in the cellular level of immunity, dysimmunoglobulinemia, and IgA deficiency [1,5].Thus, the growth trend of acute respiratory diseases in children and their role in the development of bronchial obstruction, the high risk of recurrence of obstructive bronchitis, and the possibility of bronchial asthma, an acute respiratory disease ety of immune disorders in this pathology, determine the relevance of studying the factors and mechanisms of the formation of bronchial-structural syndrome in children with respiratory tract infections.
2. Materials and Methods
- A retrospective analysis of the medical histories of children for the period 2015-2019 who were on inpatient treatment in the Department of Pulmonology of the RSSPMC of Pediatrics of the Ministry of Health of the Republic of Uzbekistan and Allergology, as well as in the City Children's Hospital of Andijan, Andijan district Multidisciplinary Central Polyclinic. Based on a retrospective analysis of 6965 medical histories of children aged 1 to 18 years with bronchopulmonary pathology, of which 1208 (17%) children with an established diagnosis of BOS, 1208 children were divided into three groups with diagnoses. I group 966 children with the community–acquired acute pneumonia with the obstructive syndrome; IIgr. – Acute obstructive bronchitis– 72 (6%) children; III -gr. - recurrent bronchitis with bronchoobstructive syndrome– 170 (14%) children. The assessment of risk factors for the development of BOS was carried out using statistical methods in epidemiological analysis. Objective: To study the main etiological factors and to identify the features of the clinical course of bronchoobstructive syndrome in children.
3. Results and Discussion
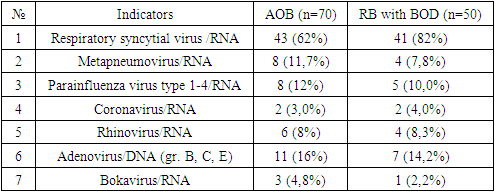
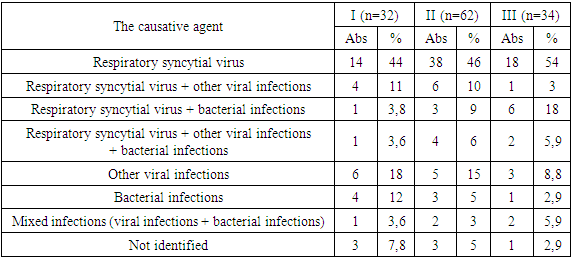
- To assess the risk factors for the development of the disease, studies were carried out, which included a thorough analysis of complaints, anamnestic data of patients, general examination data, results of physical examination methods, general clinical laboratory, microbiological, and instrumental research methods according to standard methods. To diagnose the syndromological features of the disease, data from paraclinical research methods were used: a general analysis of blood, urine, feces, X-ray examinations of the chest organs, pulse oximetry data and expert opinions. Surveys of children in the age group from 1 to 15 years were conducted. The distribution of children by age showed that community-acquired pneumonia with obstructive syndrome is more common in 1-3 years 800 (83%), 125 (13%) were registered in children aged 4-6, 32 (3%) in 7-11 years, while 9 (1%) were registered in children aged 12-18 years. Among all the examined patients, children under 1 year of life were more often ill with acute obstructive bronchitis (44%) than older children (4-6 years - 23%; 7-11 years – 24%, 12-18 years - 9%). Repeated cases of acute respiratory diseases (6 times or more) during the year were noted in 35 (48%) children with acute obstructive bronchitis, and in RB children with BOS in 88 (52%). The majority of children with acute obstructive bronchitis 52 (72%) revealed deficient conditions and a burdened premorbid background: 31 (43%) and 95 (56%) children were transferred to artificial feeding early, 40 (56%) had a history of perinatal CNS lesion, 25 (35%) and 82 (48%) - rickets, 70 (97%) and 59 (82%) and 156 (92%) - anemia. Upon admission to the department of patients with acute clinical manifestation of the disease was respiratory failure. Such a condition as weakness was observed in 33 (55.0%) patients, and appetite was reduced in 49 (81.6%) patients. Sleep disturbance, skin pallor, and shortness of breath were observed in 60 (100.0%) cases. Cyanosis of the nasolabial triangle was observed in 19 (31.6%) children. Body temperature at admission was febrile in 11 (18.3%) patients, and sub febrile - in 17 (28.3%). The cough pattern was dry in 49 (81.6%) patients and wet in 11 (18.3%). During auscultation of the lungs against the background of hard breathing, dry wheezing was heard in 47 (78.3%) patients, and wet wheezing was heard in 13 (21.6%). With chest percussion, a boxy shade of percussion sound was determined in 53 (88.3%).Exacerbation in children with recurrent bronchitis with bronchoobstructive syndrome was characterized by acute (subacute) onset, cough, and dryness at first – in 5 (8.3%), wet – in 55 (91.7%) patients. Dry cough at admission is paroxysmal, more at night; on 5-6 days of treatment, it transformed into a wet one. Cyanosis of the nasolabial triangle was observed in 39 (65.0%), from the skin - dryness – in 70.0% of patients. Auscultative signs were diverse and mainly depended on the damage to the bronchial mucosa. Dry wheezing was detected in 8 (13.3%) children, and wired wheezing in 52 (86.7%) children.During X–ray examination, 60 (100%) patients with recurrent bronchitis with bronchoobstructive syndrome showed signs of bronchial obstruction - swelling of the lung tissue, increased transparency, horizontal location of the ribs, wide intercostal spaces, flattening and low standing of the pulmonary pattern. The leading clinical manifestation of BA in all patients (in 100%) was expiratory dyspnea with the participation of auxiliary muscles in breathing with a respiratory rate under the age of 8 years above 45 in 1 minute, and older than ten years above 48 in 1 minute. The duration of shortness of breath was 4.2 ± 0.2 days. Signs of hypoxia in the form of cyanosis of the nasolabial triangle were observed in 49.2% (32) of patients, in other children cyanosis their duration was 5.5 ± 0.3 days. Acute respiratory viral infections can initiate the development of bronchial asthma (a risk factor) and cause subsequent exacerbations of the disease. The effect of respiratory viral infection on bronchial asthma is realized through the inflammatory process induced by viruses, increased reactivity of the bronchi, and activation of IgE synthesis. In patients with bronchial asthma and allergic rhinitis, attention is drawn to the significant prevalence of frequent acute respiratory infections preceding the disease (more than 4-5 times a year) in 79% of children. The association of exacerbations of bronchial asthma with acute viral infections was subsequently observed in 70% of children, which was most severe in young children (up to 3 years old). 29% of children at an early age (up to 3 years) had pneumonia; in 11% of patients, it was pretty severe and required inpatient treatment. In patients with allergic rhinitis, previous acute respiratory viral infections were much less common than in the main group (12.5%), and pneumonia was twice as rare (12.5%). The virological examination of sputum is presented in Table 1.
|
|
4. Conclusions
- Thus, a comparison of the results of clinical observations of children and patients in all study groups showed that in acute obstructive bronchitis, regardless of nasology, there is a longer manifestation of shortness of breath, oral wheezing, wet cough, and wet wheezing in the lungs. Radiographs of patients of all groups, as a rule, show emphysematous expansion of the lungs on both sides with horizontal standing of the ribs, characteristic of obstructive bronchitis syndrome. The study showed that in the etiological structure of bronchoobstructive syndrome, respiratory syncytial virus was detected in acute obstructive bronchitis in 62.0%, in recurrent bronchitis with bronchoobstructive syndrome in 82.0%, adenovirus in 16.0%, and 14.2%, metapneumovirus 12.0% and 8.0%, parainfluenza virus 12.0% and 10.0%, respectively.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML