-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1813-1816
doi:10.5923/j.ajmms.20231311.45
Received: Nov. 7, 2023; Accepted: Nov. 22, 2023; Published: Nov. 29, 2023

Radiofrequency Surgery and Balloon Dilation for Chronic Stenosis of the Larynx and Trachea in Children
R. U. Djuraev, H. E. Karabaev, F. B. Nurmukhamedova, Z. D. Egamberdieva
Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Laryngeal and tracheal stenosis pose complex challenges in pediatric otolaryngology, often necessitating surgical intervention. The choice of treatment approach is critical, as it directly impacts patient recovery and the duration of treatment. Scar-related stenosis in the larynx and trachea, often resulting from factors like prolonged intubation or surgical procedures, is a prevalent concern in pediatric patients. This study explores the efficacy of minimally invasive treatment options, such as endoscopic, microsurgical scar tissue incision, and balloon dilation, for these patients. Methods: A total of 34 pediatric patients with chronic non-neoplastic laryngeal and tracheal stenosis were treated using radiofrequency surgery or balloon dilation. Patient assessment included endoscopic examinations, radiographic tomography, evaluation of respiratory function, and imaging studies. Patients were divided into two groups based on the duration of intubation, mechanical ventilation, or tracheotomy. Surgical interventions were performed under general anesthesia, and postoperative monitoring occurred for 7-14 days. Results: The primary group, treated with radiofrequency surgery, achieved a success rate of 94.5%, with no recurrent granulation growth. In contrast, the second group, treated with balloon dilation, exhibited a success rate of 65%. Recurrence occurred in 60% of the first group. Notably, patients in the second group experienced no complications, except for one patient, likely due to the large balloon diameter in proportion to the small laryngeal size. Conclusion: Isolated, limited scar stenosis of the larynx and trachea, up to 1 cm long, with preserved cartilaginous structures, can be effectively managed using minimally invasive techniques. Combining these methods streamlines surgical treatment stages, facilitating patient rehabilitation in a single reconstructive therapy phase. These methods offer a shorter hospital stay, prevent tracheostomy in systemically compromised patients, and significantly improve treatment outcomes for this patient category. Minimally invasive techniques are valuable for managing pediatric laryngeal and tracheal stenosis.
Keywords: Radiofrequency surgery, Balloon dilation, Tracheal stenosis, Laryngeal stenosis
Cite this paper: R. U. Djuraev, H. E. Karabaev, F. B. Nurmukhamedova, Z. D. Egamberdieva, Radiofrequency Surgery and Balloon Dilation for Chronic Stenosis of the Larynx and Trachea in Children, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1813-1816. doi: 10.5923/j.ajmms.20231311.45.
1. Introduction
- Laryngeal and tracheal stenosis continues to be a relevant issue in otolaryngology. The choice of surgical approach is complex and critical, as the patient's recovery and the duration of treatment depend on the decision. The primary goal of treatment is to restore the function of the hollow structures of the neck, with extubation of the patient being the ultimate stage. Stenosis of the trachea and larynx is a leading cause of airway obstruction in pediatric patients. Correcting such anomalies remains challenging due to anatomical peculiarities in the pediatric population. Various surgical options are proposed for treatment, ranging from invasive surgery to open procedures such as laryngeal reconstruction and cricotracheotomy [1] [2] [3]. With advances in pediatric intensive care and neonatology, the number of children with scar-related laryngeal stenosis has increased [4] [5].For a long time, open laryngotracheal plastic surgery was the primary treatment approach for scar-related laryngeal stenosis. Balloon dilation has been introduced to treat immature and mild post-intubation airway stenosis [5]. Among all cases of laryngeal and tracheal stenosis, the proportion of post-resuscitation stenosis, according to various authors, ranges from 50 to 90% [6].The treatment of non-neoplastic laryngeal and tracheal stenosis is a challenging task due to the nuances of surgical technique and access, the complexity and risks of anesthesia support, and the tendency of the disease to recur despite its "benign" nature. In the vast majority of cases, these stenoses are scar-related and result from some form of injury to the larynx and trachea, including iatrogenic causes (prolonged intubation, surgical interventions on the larynx and trachea) [7] [8].Children with airway stenosis have represented a significant clinical challenge throughout the history of otolaryngology and head and neck surgery. In recent decades, due to advances in neonatology and cardiac surgery, the number of surviving children with congenital developmental anomalies who have undergone significant surgical treatment and prolonged ventilatory support has increased, leading to the development of upper airway stenosis [10]. Consequently, the number of children needing to restore the patency of their natural airways has significantly increased [8].Objective of the Study: To evaluate the results of endoscopic surgical interventions using radiofrequency and balloon dilation in non-neoplastic laryngeal and tracheal stenosis in children.
2. Materials and Methods
- The research was conducted at the Department of Otolaryngology, Pediatric Otolaryngology, and Pediatric Dentistry in TashPMI Clinic from 2020 to December 2022 to investigate the potential applications of radiofrequency surgery and balloon dilation for the treatment of laryngeal and tracheal stenosis in pediatric patients. A total of 34 children diagnosed with chronic non-neoplastic laryngeal and tracheal stenosis were treated with these techniques during this period.Patient evaluations involved a comprehensive assessment, including endoscopic examinations of the larynx and trachea, radiographic tomography, the measurement of external respiratory function parameters, and both computed tomography and magnetic resonance imaging. Patients were divided into two groups based on the time that had passed since their initial intubation, mechanical ventilation, or tracheotomy.The first group consisted of 16 patients who received treatment in the intensive care units at TashPMI and underwent radiofrequency surgery. The second group included 18 patients who had a history of intubation, mechanical ventilation, and tracheotomy for one month or longer. For this group, balloon dilation was chosen as the treatment modality.
3. Results
- The patient population was stratified by age as follows. The age distribution of the observed patients (n = 34) included the following age groups: under one year - 3 children (8.8%), 1-3 years - 9 children (26.4%), 3-7 years - 14 children (41.1%), 7-10 years - 5 children (14.7%), and 10-14 years - 3 children (8.8%). From the presented information, it is evident that the majority of patients fell within the age range of 3-7 years (see Figure 1).
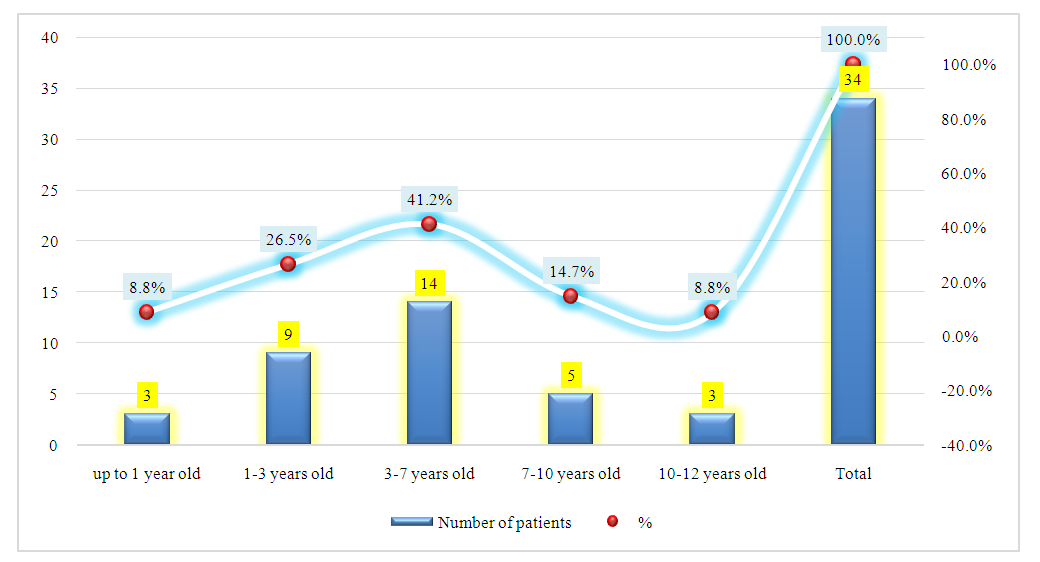 | Figure 1. Demographic Characteristics of Patients with Laryngeal and Tracheal Stenosis |
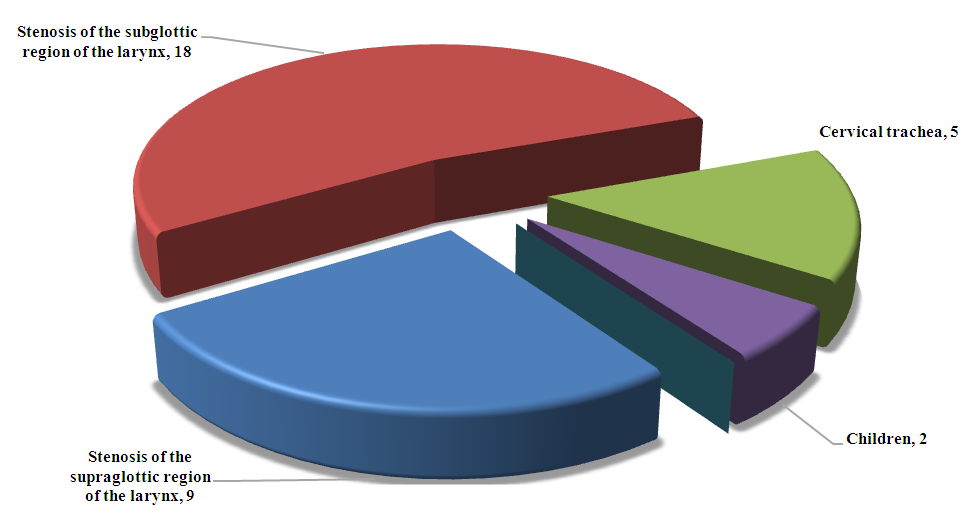 | Figure 2. Distribution of Patients by Stenosis Location |
4. Conclusions
- Isolated, limited scar stenosis of the larynx and trachea, with a length not exceeding 1 cm, and the preservation of cartilaginous structures, regardless of the lumen diameter, represents an indication for minimally invasive treatment methods. These methods include endoscopic, microsurgical scar tissue incision, and balloon dilation. These techniques facilitate the rehabilitation of patients within a short duration of hospitalization, prevent the need for tracheostomy in patients with systemic pathologies, and significantly enhance the effectiveness of treatment for this patient category. The streamlining of surgical treatment stages by combining them allows for the rehabilitation of patients in a single stage of reconstructive therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML