-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1808-1812
doi:10.5923/j.ajmms.20231311.44
Received: Oct. 28, 2023; Accepted: Nov. 17, 2023; Published: Nov. 25, 2023

Reconstructive Surgery of the Urethra in Men
Ergashev Bobirjon Abdilhashimovich
Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Ergashev Bobirjon Abdilhashimovich , Andijan State Medical Institute, Andijan, Uzbekistan.
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Urethral stricture is a polyethological disease characterized by symptoms of the lower urinary tract, in which the diameter of the urethral lumen narrows down to its complete obliteration due to scar degeneration of the tissues of the urethra wall. The prevalence of narrowing of the urethra in men varies from 0.6% to 0.9% in the population and increases with the age of patients, while extensive and subtotal lesions of the urethra are diagnosed in 15-18% of cases. Urethral strictures are scarring of the urethra that can lead to obstructive and/or irritating symptoms when urinating, regardless of anatomical localization.
Keywords: Reconstructive surgery, Urethra, Men, Strictures, Iatrogeny
Cite this paper: Ergashev Bobirjon Abdilhashimovich , Reconstructive Surgery of the Urethra in Men, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1808-1812. doi: 10.5923/j.ajmms.20231311.44.
Article Outline
1. Introduction
- Urethral strictures are more often acquired than congenital. Congenital forms are located mainly in the anterior part of the urethra, usually have a short length and are usually associated with other malformations, such as hypospadias or megalourethra. Acquired forms of urethral stricture are iatrogenic, but there may also be post-inflammatory, caused by various sexual infectious diseases (gonorrhea, chlamydia, etc.), chronic inflammation or post-traumatic conditions.However, in about 30% of patients, the etiology remains unclear. Age also plays an important role in the causal group. Recent studies show that urethral strictures in men under the age of 35 mostly have an inflammatory or unclear etiology. On the contrary, in men over 50 years of age, iatrogenic correlation (post-transurethral surgery, history of catheter insertion) was found in 55% of cases [1,3].Urethral stricture occurs as a result of scarring of the urethra. There are two responsible factors in pathogenesis. On the one hand, the lesion of the mucous membrane with a local infection, which can subsequently spread to the corpus spongiosum, and on the other hand, the subsequent healing process with the formation of a scar. The so-called spongy fibrosis develops. The more pronounced the scarring, the more severe the stricture [4]. Proximal strictures, which occur as a result of fibrosis after traumatic ruptures of the urethra, differ from them. Distal strictures are a special condition that can occur as a result of non-infectious inflammatory processes of balanitis xerotica obliterans (lichen sclerosus).
2. Diagnostics
- A necessary condition for successful therapy is the correct choice of surgical intervention. In preoperative diagnosis, in addition to anamnesis, clinical examination, uroflowmetry (Fig.1 a), urethrocystoscopy, retrograde urethrogram (Fig. 1 b) or alternative urethra cystography are of great importance. This allows you to estimate the localization, length and shape of the stricture. With the help of urethral sonography, under certain circumstances, it is possible to estimate the extent of spongiofibrosis [5-7]. However, this method has not yet found application in everyday clinical practice. Cystoscopy is of particular importance in special cases. In order not to affect the possible subsequent reconstructive intervention, care must be taken not to expand the strictures. Unlike many other diseases in urology, diagnostic and therapeutic procedures are less standardized.
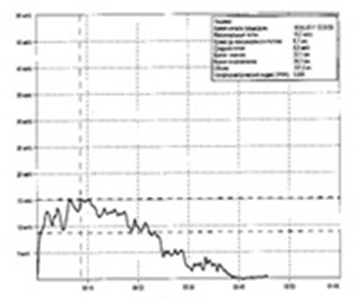 | Figure 1a. Uroflowmetry |
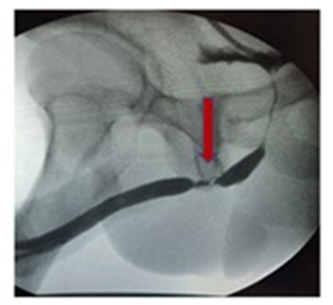 | Figure 1b. Retrograde urethrography (arrows indicate strictures of the bulbous urethra) |
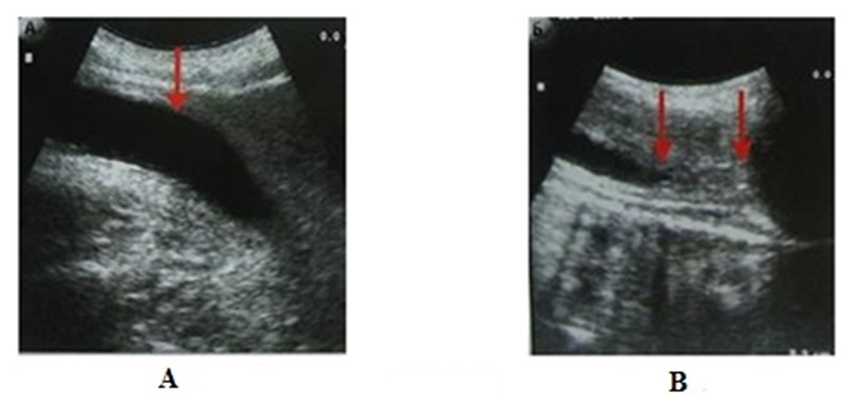 | Figure 1c. Ultrasound of the urethra: A – normal lumen of the bulbous urethra; B – arrows indicate the boundaries of severe stricture of the bulbous urethra |
3. The Possibilities of Therapy
- Minimally invasive therapy. Augmentation/dilation. Urethral stricture augmentation is the most ancient form of therapy and was used already in the pre-Christian era. During this procedure, spongiose fibrosis expands, and countless microtrauma forms in the scar, which leads to repeated scarring. Therefore, the boogie can only have only a temporary effect on the obstacle.As a rule, it can be expected that the narrowing will recur in four to six weeks [8]. For this reason, the procedure is only suitable for patients who refuse surgery or are not suitable for this for anesthetic reasons.
4. Endoscopic Urethrotomy (Urethrotomia Interna)
- The diverse course of the disease and the high tendency to relapse of the disease present enormous difficulties for everyday clinical practice. The choice of a suitable surgical procedure should be individually adapted to the patient. In general, the distal location, stricture length of more than 2.5 cm and the number of previous operations are considered poor prognostic parameters. Short bulbar strictures (< 1 cm) have a better prognosis with a lower recurrence rate and an endoscopic recovery attempt seems justified. Sachse urethrotomy is the main method of treating strictures of the short urethra. Victims should be informed and clarified in this regard. However, there are only a few strictures that can be finally eliminated with these measures. For most strictures, the probability of recurrence of the stricture after dissection significantly exceeds is more than 50%. The resulting new stricture is always longer and more difficult to treat than the previous one. After the third urethrotomy, the recurrence rate increases to 100% [9]. The length of the follow-up period seems to be of particular importance for the frequency of relapses when using this technique. Such operations are not indicated for strictures of the penile urethra or navicular fossa [10].In general, however, due to the poor long-term results of Sachse urethrotomy, on the one hand, and good long-term results of open urethral reconstruction, on the other, repeated urethrotomy should be performed only to those patients for whom open reconstruction is out of the question due to concomitant diseases or who do not want open reconstruction after a detailed consultations [9,11].
5. Open Surgical Reconstruction of the Urethra
- First, a distinction should be made between anterior structures and posterior stenoses. The term "urethral stricture" classically refers to anterior structures. With anterior strictures, panel and bulbar structures are distinguished. Posterior stenoses are fundamentally different in genesis and, accordingly, in therapy.
6. Stricture Resection with End-to-End Anastomosis
- Short bulbar structures < 2 cm are dissected and resected through the perineal approach. Then the continuity of the two ends of the urethra without tension, mutually converging, is restored by an end-to-end anastomosis. Complete removal of stricture and scar tissue (transsection technique) is crucial for success. The literature reports a long-term success rate of up to 90%. Even as a second operation, end-to-end anastomosis can lead to good success with strictures of the short urethra [12]. In surgery of bulbar relapses, this often avoids replacement urethroplasty, the success rate of which is slightly lower than in end-to-end urethral reconstruction. The question of the effect of repeated surgical intervention on erection, ejaculation and continence remains unresolved in many studies.
7. Reconstruction of the Urethra with the Help of Vascularized Skin Flaps
- With the technique using vascularized skin flaps, the urethra opens longitudinally along the entire length of the stricture, and the resulting defect is screwed into the open urethra with the help of a vascularized skin flap of the penis shell, which is prepared on the underlying fascia (Darthos fascia) is inserted into the open urethra. There are various techniques for this, but the blood supply of these "flaps" is always provided through the subdermal connective tissue. These flap methods are a less complex procedure, which in prospective randomized trials has shown comparable results with transplantation methods, but requires a longer operation time and are associated with an increased complication rate (skin necrosis about 15%, fistula formation about 5%) [1,13,14]. Therefore, this is a somewhat outdated surgical technique that can only be used in exceptional cases.
8. Reconstruction of the Urethra with a Free Graft (Foreskin, Oral Mucosa or Thigh Skin)
- Open reconstructive procedures are used in complex strictures or in recurrent situations [17-19]. In our clinic, such procedures are performed secondarily for patients who have undergone two endoscopic urethrotomies, and first of all for so-called high-risk patients. High-risk patients are characterized by an extended stricture of more than 5 cm, penile or membranous localization with pronounced spongiofibrosis. We decide to perform a one-stage or multi-stage reconstructive procedure depending on the length of the stricture, the width of the residual lumen and the degree of spongiofibrosis. Longer strictures require transplantation urethroplasty. Currently, a free graft of the oral mucosa (the inner surface of the cheeks, lips or the lower part of the tongue) is the most common free graft due to its easy availability and low level of complications [20,21]. Numerous other autologous biological materials (foreskin, thigh skin, bladder mucosa, colon mucosa) are used in special cases. A free, neovascularized graft should be very thin and wide, so that rapid new vascularization is possible due to capillary germination. In our department, we fundamentally prefer to use free grafts of the oral mucosa. The urethra is fully mobilized in the stricture area and is cut off from the corpora cavernosa. Then the urethra opens longitudinally along the entire length of the stricture (Fig. 2). Then the removed pieces of the oral mucosa (graft) are sewn for plastic expansion of the resulting defect (Fig. 3 a, b).
 | Figure 2. Longitudinal section of the urethra and measurement of the length of the stricture |
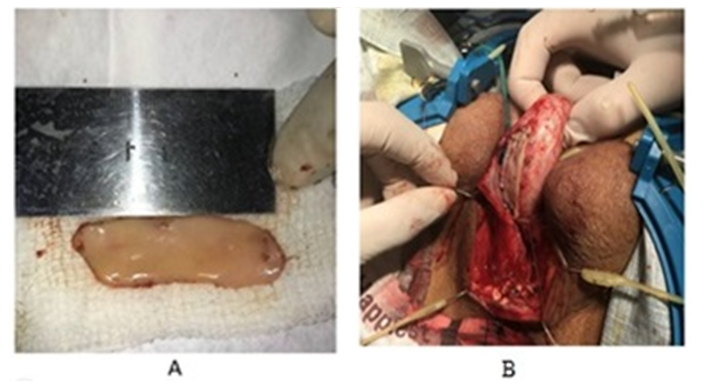 | Figure 3. A – Free buccal flap. B – Dorsal augmentation of the urethra with a free buccal flap |
9. Bulboprostatic Anastomosis
- A special feature is the reconstruction of the urethra in case of complete occlusion after rupture of the urethra against the background of a serious accident. This is explained by the fact that the obstruction is always located in close proximity to the urethral sphincter and is relatively accessible for surgical reconstruction due to its anatomical location [15]. The procedure of choice for such damage to the urethra is bulboprostatic anastomosis. In this case, the scar tissue formed after the injury is completely removed and a new connection is created between the urethra and the prostate. However, in most cases, it is not possible to preserve the urethral sphincter [15,16].
10. Conclusions
- Before planning an operation, it is necessary to carry out sufficient diagnostics. Knowledge of etiology also makes it possible to predict relapse. Standardized perioperative procedures help to avoid complications. The versatility of application of the oral mucosa in any localization and with various techniques and its simplicity of technique make it the most suitable basic material for urethral reconstruction today. The repertoire of a reconstructive surgeon should be broad in order to successfully cope with unexpected and unforeseen situations.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML