-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1786-1788
doi:10.5923/j.ajmms.20231311.38
Received: Oct. 30, 2023; Accepted: Nov. 20, 2023; Published: Nov. 25, 2023

Experience in Surgical Treatment of A-Pattern Strabismus in Children
Kalankhodjaeva D. B. 1, Babadjanova L. D. 2
1Department of Pediatric Ophthalmology, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
2Department of Ophthalmology, «Tibbiyot Dunyosi» Clinic, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A-type strabismus, in adduction, can be caused by hyperfunction of the superior oblique (SO) muscle and hypofunction of the inferior oblique muscle, which leads to dysfunction of this muscle group with an imbalance in the organic balance. Purpose: to study the effectiveness of posterior tenotomy of the SO in A-pattern caused by its hyperfunction. Material and methods. The first group included 15 children (30 eyes) with hyperfunction of the superior oblique muscle, where posterior tenotomy of the SO was performed. The second group consisted of 20 children (40 eyes) without hyperfunction of the superior oblique, where horizontal transposition of the extraocular muscles was performed. Results. In the first group (30 eyes) with hyperfunction of the superior oblique muscle, posterior superior oblique tenotomy eliminated the A pattern in 96% of cases, and its weakening was observed in 4% of cases. Underaction fixed in 98% of cases. In the second group (40 eyes) without hyperfunction of the superior oblique, where the horizontal deviation was simultaneously eliminated with rectus muscles transposition, the vertical component was eliminated in 89%, in 19% there was a residual angle of the horizontal component from 5-15 PD. Forced position of the head -ocular torticollis was corrected in 100% within 3-6 months.
Keywords: Vertical strabismus, A pattern, Hyperfunction of the superior oblique muscle, Posterior tenotomy of the superior oblique muscle, Horizontal transposition of the rectus muscles
Cite this paper: Kalankhodjaeva D. B. , Babadjanova L. D. , Experience in Surgical Treatment of A-Pattern Strabismus in Children, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1786-1788. doi: 10.5923/j.ajmms.20231311.38.
1. Introduction
- There are several types of vertical strabismus, called patterns, that characterize external horizontal deviations when performing vertical movements. Their etiopathogenesis is multifactorial and may be associated with dysfunction of both oblique and rectus muscles, displacement of the muscular scleral attachments and orbital anomalies. [1,3,4] The mechanism of patterns remains poorly understood to date. The most common patterns - A or V occur in 15-25% of all cases of horizontal strabismus, and such patterns as Y, X, lambda, etc. are also known. For pattern A, the difference in deviations when looking up and down is from 10 PD to 15 PD with the smallest difference in character deviations for the A-pattern, since when looking down, the convergence of tension increases. [2] Attending turns of eye movements, inward-incyclotorsion, as well as outward-excyclotorsion, are possibly due to deviations - the pattern of the figurative form. At the same time, muscle strength of both the medial and lateral rectus muscles changes. [7] Also, vertical types of strabismus are the cause of the abnormal position of the head of ocular torticollis. A-type strabismus, when maintained, can be caused by hyperfunction of the superior oblique muscle and hypofunction of the inferior oblique muscle, which leads to dysfunction of these muscle groups with a violation of the organic balance [5,6,7]. Clinically detected by the presence of underaction during adduction (deviation of the eye downward and inward during adduction). Typically, most patients with pattern strabismus have dysfunctional oblique muscles. This clinical observation, combined with a theoretical construct, has led to the educated guess that oblique muscle dysfunction is the cause of the “A” and “V” patterns.
 | Figure 1. With A-pattern exotropia, convergent deviation increases with depression and decreases with elevation. [1] |
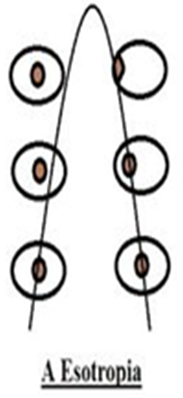 | Figure 2. With A-pattern esotropia, deviation increases with elevation, decreasing with depression |
2. Material and Methods
- All patients underwent: viziometry, refractometry, measurement of deviation in 9 positions of gaze, detection of abnormal head position (ocular torticollis), ophthalmoscopy, assessment of binocular vision, traction test (interoperative).Characteristics of patients. To solve these problems, in the eye department of the clinic of the Tashkent Pediatric Medical Institute and the private clinic “Tibbiyot Dunyosi”, we conducted a prospective analysis of 35 children (70 eyes) with A-Pattern. The patients were divided into 2 groups. The type of surgery was determined by the underlying pathophysiology and targeted the affected extraocular muscle. [6]The first group included 15 children (30 eyes) with hyperfunction of the superior oblique muscle, where a posterior tenotomy of the SO was performed. Age ranged from 4-8 years. All children exhibited underaction (deviation of the eye downwards and inwards) during adduction.The second group consisted of 20 children (40 eyes) without hyperfunction of the superior oblique, where horizontal transposition of the extraocular muscles was performed.Visual acuity in 19 (54%) children was -1.0, in 16 (46%) 0.7-0.9. Emmetropic refraction in 19 (54%), hypermetropic – 11 (33%), myopic – 5 (13%). The difference in the deviation angle of vertical strabismus varied from 10PD - 25PD. Horizontal deviation from 20-40 PD with a divergent component was observed in 14 (40%), converging in 21 (60%). Compensating position of the head (ocular torticolis) - chin up was noted with A-pattern esotropia in 11 (52%), chin down with exotropia in 2 (17%).For good visualization during surgery, we have optimized the conjunctival surgical approach - a “П”-shaped conjunctival incision with an extension at the base, so that both the medial and lateral edges of the superior rectus muscle are sufficiently visualized for revision of possible additional legs of the SO tendon attachment.
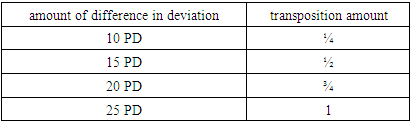
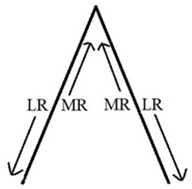 If there was a pattern with no hyperactivity of the oblique muscles, transposition of the horizontal muscles up or down was used. The attachment point of the muscle should be shifted in the direction of weakening its action. To correct the A-shape, the internal rectus muscles are moved upward to the apex, which increases its effect when looking down and weakens when looking up, and the external muscles are moved down to the base.The amount of transposition depends on the magnitude of the difference when looking up and down. (Table 1)
If there was a pattern with no hyperactivity of the oblique muscles, transposition of the horizontal muscles up or down was used. The attachment point of the muscle should be shifted in the direction of weakening its action. To correct the A-shape, the internal rectus muscles are moved upward to the apex, which increases its effect when looking down and weakens when looking up, and the external muscles are moved down to the base.The amount of transposition depends on the magnitude of the difference when looking up and down. (Table 1)
|
3. Results
- In the first group (30 eyes) with hyperfunction of the superior oblique muscle, posterior tenotomy of the SO eliminated the A pattern in 96% of cases, and its weakening was observed in 4% of cases. Underaction eliminated in 98% of cases.In the second group (40 eyes) without hyperfunction of the superior oblique, where the horizontal deviation was simultaneously eliminated with rectus muscles transposition, the vertical component was eliminated in 89%, in 19% a residual angle of the horizontal component was observed from 5-15 PD. In 10% of cases, the horizontal component corrected spontaneously within 6 months; in 8%, the second stage of surgical correction was performed. Forced position of the ocular torticollis corrected in 100% within 3-6 months after surgical correction of the vertical component.
4. Conclusions
- 1. Application of posterior tenotomy technology in surgery A pattern with ECM hyperfunction is promising; it eliminates the vertical deviation that occurs during adduction without disturbing the symmetrical position of the eyes with direct gaze.2. Transposition of horizontal motors without ECM hyperfunction is a fairly effective way to eliminate A-pattern strabismus in children, which allows you to simultaneously eliminate or reduce both the vertical and horizontal components.3. Timely elimination of the vertical component-corrects the ocular torticollis independently allowing differentiation of it from cervical torticollis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML