-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(11): 1778-1785
doi:10.5923/j.ajmms.20231311.37
Received: Oct. 28, 2023; Accepted: Nov. 19, 2023; Published: Nov. 23, 2023

Results of Plastic Surgery of Post-Burn Scar Deformity of the Face and Neck with a Free Skin Graft
Madazimov М. М. , Rasulov J. D. , Nizamkhodjaev S. Z. , Yakubov F. R.
Andijan State Medical Institute, State Institution “Republican Specialized Scientific and Practical Medical Center for Surgery named after V.Vakhidov
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

With plastic surgery of post-burn scarring of the face and neck and the inability to use local tissues, it becomes necessary to use plastic surgery with a full-layer free skin graft. In this aspect, the issues of the quality of graft engraftment remain relevant, and in the long term – aesthetic moments, including the formation of hypertrophic scars, keloids, changes in pigmentation of the transplanted skin, as well as the most formidable complication - the retraction of the graft with a recurrence of scar deformation. The aim of the study: to improve the results of surgical rehabilitation of patients with post-burn scar deformity of the face and neck by applying a free full-layer skin graft. Materials and methods: according to the applied plastic surgery methods, 115 patients were divided into two groups. In the main group – 54 patients, the proposed method of eliminating post–burn scar deformity of the face and neck was performed; in the comparison group - 61 patients, plastic surgery with a free skin graft was performed according to traditional methods. Results: an improved method of surgical treatment of post-burn scarring of the face and neck with a free full-layer skin flap, characterized by an improvement in the quality of the graft taken, by reducing the degree of its retraction, as well as stimulation of vascularization, reducing the risk of formation of subcutaneous fluid accumulations, excluding long-term wearing of a pressure bandage, which generally contributes to a more physiological engraftment of transplanted tissues.
Keywords: Burns of the face, Plastic surgery, Post-burn scar deformity, Free skin graft
Cite this paper: Madazimov М. М. , Rasulov J. D. , Nizamkhodjaev S. Z. , Yakubov F. R. , Results of Plastic Surgery of Post-Burn Scar Deformity of the Face and Neck with a Free Skin Graft, American Journal of Medicine and Medical Sciences, Vol. 13 No. 11, 2023, pp. 1778-1785. doi: 10.5923/j.ajmms.20231311.37.
1. Introduction
- Post-burn contractures in the face and neck have a multifactorial origin and are difficult to prevent with extensive burns. Burns of the face lead to distortion of anatomical landmarks, causing aesthetic, functional and psychological problems. Each subunit of the face is unique in structure, so the surgeon needs to adjust the operation time and technique depending on the area and severity of the contracture. The contracture of one unit, especially the neck and forehead, can strengthen the contracture of neighboring subunits. The role of these external influences must be taken into account when determining the sequence of surgical procedures. The surgeon must master all methods of reconstructive surgery, from skin grafting to tissue expanders and microsurgery, in order to get the best results [1]. Surgical intervention in post-burn contractures should be avoided during the active phase of healing and scarring (i.e. while the scar is still immature and highly vascularized). It usually takes about 1 year. Before surgery for contracture, the scar should mature, become soft, elastic and less vascularized. A highly vascular scar bleeds more during surgery and makes it difficult to achieve ideal hemostasis, which leads to poor graft engraftment and leads to a recurrence of contracture.One of the radical methods of plastic surgery for burns in this area is expander dermotension. The extension can be located in direct contact with the reconstructed area to perform a local pre-expanded flap, or in another area to perform a regional pre-expanded flap, followed by a local or distal extension to achieve a pre-expanded complete skin graft [2]. The advantage of using healthy skin next to the affected areas is that it is similar in terms of pigmentation, hairiness, thickness and texture. In light of this, zygomatic, chin or labial skin extensions are considered particularly suitable for the treatment of perioral lesions. However, they can cause certain consequences for the donor site, such as the appearance of stretch marks, loss of skin elasticity or a decrease in hair density both on the scalp and in the beard area in men. Treatment of the consequences of burns or other loss of perioral tissues is difficult due to the place of their occurrence, functional importance, as well as social and aesthetic aspects. This is a mobile area with concave and convex features and a complex muscular structure, the deformation of which can manifest itself during movement or only during relaxation. The functional consequences of burns in this area are skin retraction and lack of skin, which can lead to labial eversion, microstoma, the formation of folds and subsequent lip failure, as well as the inability to open the mouth opening, which jeopardizes oral hygiene and intubation procedures. The results of the reconstruction of the upper and lower lips, as well as the eyelids, indicate that this technique is associated with the risk of ectropion [3]. The main problem of expander dermotension with the vastness of a scar defect that occupies almost the entire head or neck area is the lack of a substrate - normal tissue for expander dermotension.Skin grafts, dermal substitutes with grafts and flaps are available to cover the post-release raw area [4]. Grafts help to show the cervical-chin angle and the contour of the neck. Nevertheless, the grafts are not malleable and shrink. To a large extent, the use of dermal substitutes gives better results and can lead to pinching of the skin, although attention to detail will be required to obtain a complete grip on large areas [5]. Good results can be obtained if the patient can have thin perforant flaps raised. In the presence of microsurgical experience, thin flaps from deep lower epigastric perforation, thin anterolateral femoral flaps or flaps of the radial artery of the forearm can be used [6]. These flaps can also be pre-straightened so that the area of available skin is larger for excellent results. Extensive primary thinning of these flaps can lead to partial necrosis and may require skin grafting. This jeopardizes the result, and the alternative is to strive for the complete survival of the flap and its subsequent thinning.Thus, the issue of plasty of extensive post-burn defects of the soft tissues of the head and neck is still open. Microsurgical autotransplantation of complex flaps is acceptable and effective for plasty of extensive scar defects of the head (in the absence of conditions for expander dermotension). At the same time, microsurgical autotransplantation of tissues requires special equipment and tools, a trained microsurgical team. Microsurgical flaps cannot be used in cases where there are no recipient vessels for revascularization of the graft [7]. If it is impossible to use local tissues, it becomes necessary to use plastic surgery with a full-layer free skin graft. In this aspect, the issues of the quality of graft engraftment remain relevant, and in the long term – aesthetic moments, including the formation of hypertrophic scars, keloids, changes in pigmentation of the transplanted skin, as well as the most formidable complication - the retraction of the graft with a recurrence of scar deformation. An improved method of free skin grafting has been proposed for plastic surgery, the evaluation of the results of which served as the basis for this study.
2. Materials and Methods
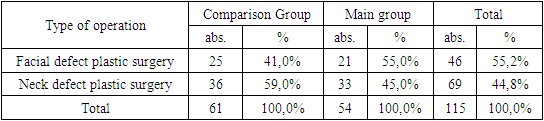
- All patients were divided into two groups according to the applied plastic surgery methods. In the main group – 54 patients, the proposed method of eliminating post–burn scar deformity of the face and neck was performed; in the comparison group - 61 patients, plastic surgery with a free skin graft (FSG) was performed according to traditional methods (Table 1).
|
 | Figure 1. Patient Zh. Post-burn mid-lateral bilateral scarring of the neck. Neck contracture III art . Pronounced cosmetic defect. Plastic surgery with a free skin graft |
3. Results and Discussions
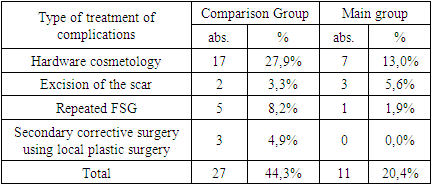
- The fundamental point in FSG plastic surgery is the long-term fixation of the pressure bandage, which is applied for 5 or more days. That is, the first dressing is performed no earlier than 5 days later. In this regard, the proposed method of FSG plastic surgery made it possible both to eliminate the need for applying a pressure bandage and to shorten the time of primary isolation of the transplanted skin flap. In particular, after plastic surgery in the facial area in the comparison group, the primary dressing was performed after 5.2±0.5 days, whereas in the main group after 3.3±0.5 days (t=12.84; p<0.05), after plastic surgery in the neck, these indicators were 5.1± 0.4 days versus 3.1± 0.3 days (t=22.10; p<0.05). Accordingly, in general, in all patients, the average duration of wearing the bandage was 5.2±0.5 days versus 3.2± 0.4 days (t=24.30; p<0.05).The following complications were characteristic of this type of plastic surgery. Partial graft necrosis after facial plastic surgery developed in 2 (8.0%) patients in the comparison group, in these cases, flap necrosis occupied about 20% of the entire surface. There were no such complications in the main group. Divergence of sutures in the flap tension zone in the comparison group was noted in 2 (8.0%) patients, in the main group in 1 (4.8%). Subcutaneous suppuration developed in 1 (4.0%) patient in the comparison group. A typical complication for FSG plastic surgery in the comparison group was the formation of a subcutaneous hematoma, which was verified by ultrasound, the elimination of the latter was carried out using percutaneous puncture. In the main group, due to the use of a hemostatic agent, no such complications were noted. In total, 5 (20.0%) patients had various complications in the comparison group after FSG facial defects plastic surgery, while only 1 (4.8%) in the main group. Accordingly, the postoperative period proceeded without complications in 20 (80%) and 20 (95.2%) patients. According to this criterion, due to the small number of groups, no significant difference was obtained (χ2=2,337; df=1; p=0.127).After plastic surgery in the neck area, there were 7 (19.4%) patients with various complications in the comparison group, 2 (6.1%) in the main group (χ2=2.719; df=1; p=0.100).The analysis of the frequency of the development of immediate complications in general by groups showed that in the comparison group there were 12 (19.7%) with various complications, of which 5 (8.2%) had partial necrosis of the graft, in the main group complications developed in 3 (5.6%) (χ2=5.033; df=1; p=0.025) (fig. 2).
 | Figure 2. The frequency of immediate complications after plastic surgery of all defects with a free skin graft |
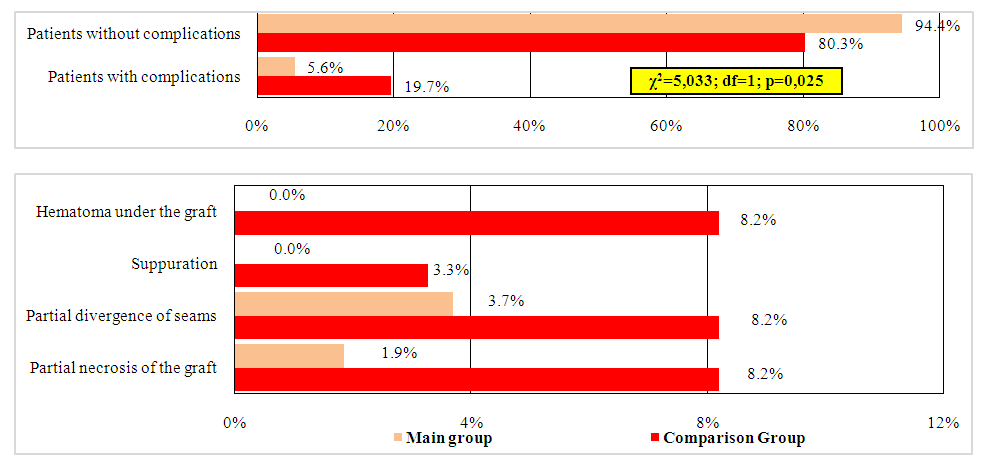
 | Figure 3. The frequency of long-term complications after plastic surgery of all defects with a free skin graft |
|
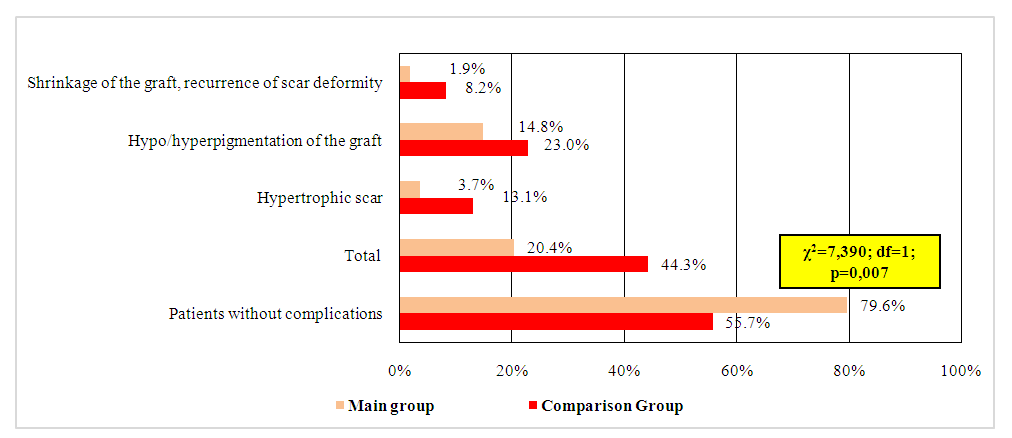
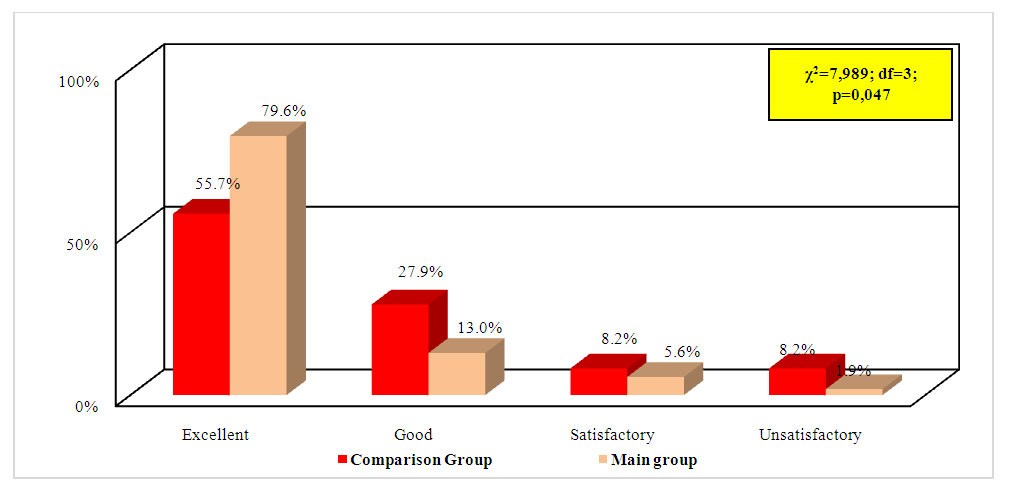 | Figure 5. Summary of long-term functional and aesthetic results of plastic surgery of facial and neck defects with a free skin graft |
4. Conclusions
- An improved method of surgical treatment of post-burn scarring of the face and neck with a free full-layer skin flap is characterized by an improvement in the quality of the graft taken, by reducing the degree of its retraction, as well as stimulation of vascularization, reducing the risk of formation of subcutaneous fluid accumulations, excluding long-term wearing of a pressure bandage, which generally contributes to a more physiological engraftment of transplanted tissues.The use of the proposed method of taking a full-layer skin graft and plasty of post-burn scar deformity in the face and neck due to the strengthening of local reparative processes, reducing the risk of flap tension with partial suture divergence or necrosis allowed to reduce the frequency of immediate postoperative complications from 19.7% to 5.6% (χ2=5.033; df=1; p=0.025) and long-term complications from 44.3% to 20.4% (χ2=7,390; df=1; p=0.007), respectively, reduce the need for the use of hardware cosmetology from 27.9% to 13.0% and repeated surgical intervention from 16.4% to 7.4% (χ2=7.391; df=2; p=0,025).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML